How I Do It: Regional Anesthesia for Shoulder Surgery
Cite as: Pai P, Bohaczuk S. How I do it: regional anesthesia for shoulder surgery. ASRA News 2020;45. https://doi.org/10.52211/asra110120.065
Introduction
The first brachial plexus block was performed by William Stewart Halsted at the Roosevelt Hospital in New York City in 1885 for minor surgery of the arm.[1] In 1925, Professor Henryk Hilarowicz, a Polish surgeon, described the technique of brachial plexus block performed in the interscalene groove.[2] Forty-five years later, Alon Winnie reintroduced this technique into current practice. Comparing the two techniques, Hilarowicz’s method relied on a single skin puncture followed by successive changes in the direction and depth of needle placement to evoke paresthesia of the individual branches of the brachial plexus and deposit the local anesthetic, while Winnie’s method described needle insertion into the fossa between the anterior and middle scalene muscles, perpendicular to the skin in all planes, and advancement medially, dorsally, and caudally. Local anesthesia (LA) was injected in the interscalene groove once the patient reported paresthesia to the arm and or shoulder.
The interscalene block (ISB) remains the gold standard regional technique for shoulder surgery.
The interscalene block (ISB) remains the gold standard regional technique for shoulder surgery due to the proximal position of the targets, with injection at the level of roots/early trunks. By injecting local anesthesia in the interscalene groove at the level of the cricoid cartilage, C5-C7 roots are likely to be blocked, along with all of their distal branches. This makes interscalene block ideal for use during shoulder arthroscopies and total shoulder arthroplasties (TSAs).
Anatomy
The innervation to the shoulder is complex, involving divisions of the brachial plexus at multiple levels (Figure 1). The bones and muscles of the shoulder are innervated primarily by branches of C5-C6, including the suprascapular and subclavian nerves (which branch off at level of trunks), the subscapular nerves (branching off at level of cords), and the axillary nerve (a terminal branch). The musculocutaneous nerve (terminal branch) contributes to the upper humerus innervation, and the long thoracic nerve (from combination of root level division of C5-C7) contributes to the scapula. Major muscles of the shoulder include the pecs major (innervated by the lateral pectoral nerve, a branch off the lateral cord), the deltoid (innervated by the axillary nerve), and the muscles of the rotator cuff: subscapularis (innervated by upper and lower subscapular nerves, which contain C5-C6 fibers that branch off from the posterior cord), teres minor (innervated by the axillary nerve), and supraspinatus and infraspinatus (both innervated by the suprascapular nerve). The cutaneous innervation primarily affected by surgery in this region includes C5-C7.
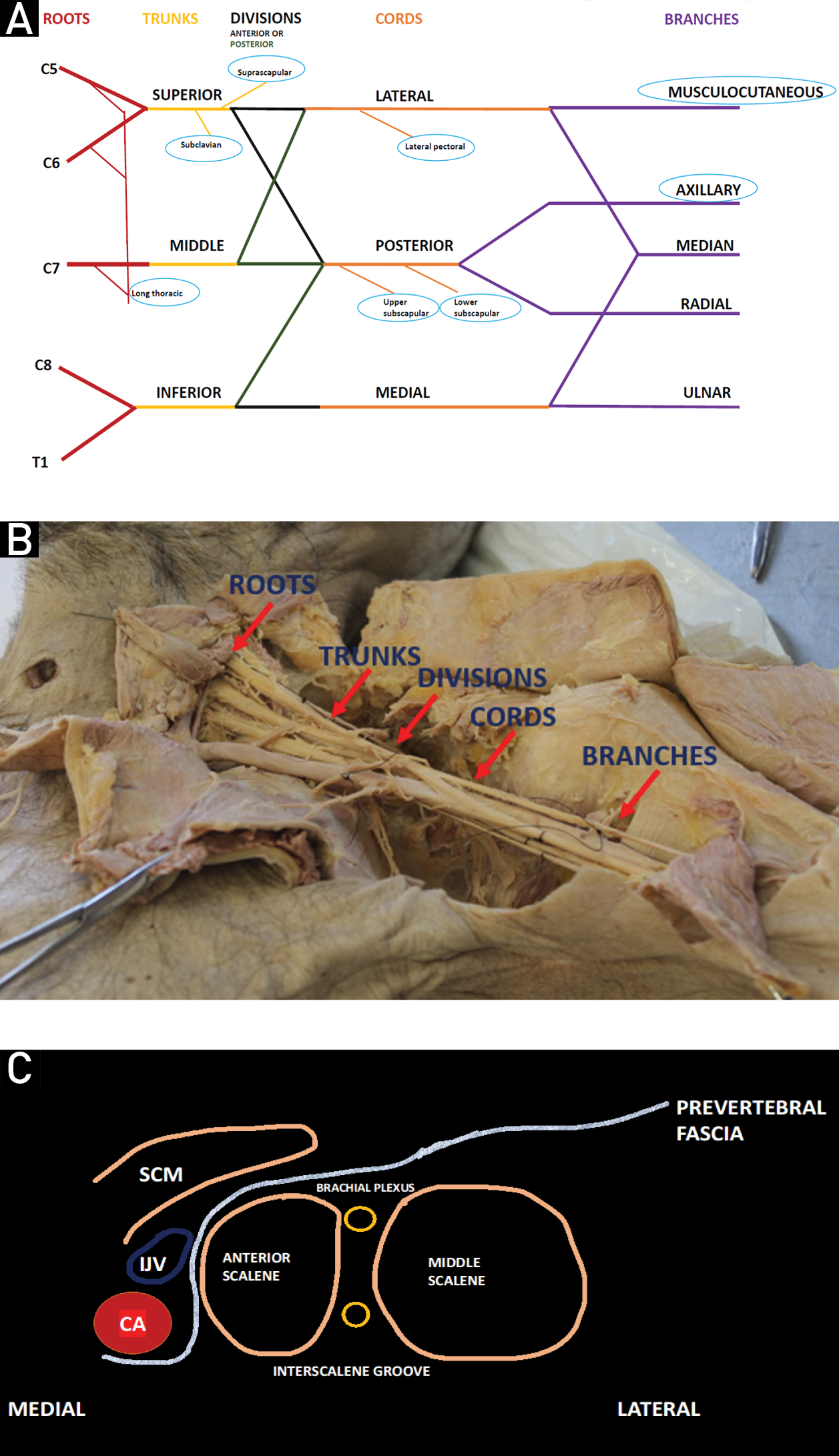
Figure 1: Brachial plexus anatomy. 1A: Brachial plexus line outline with attention to shoulder contributors (circled). 1B: Cadaveric dissection of brachial plexus. 1C: Sketch of interscalene block anatomy
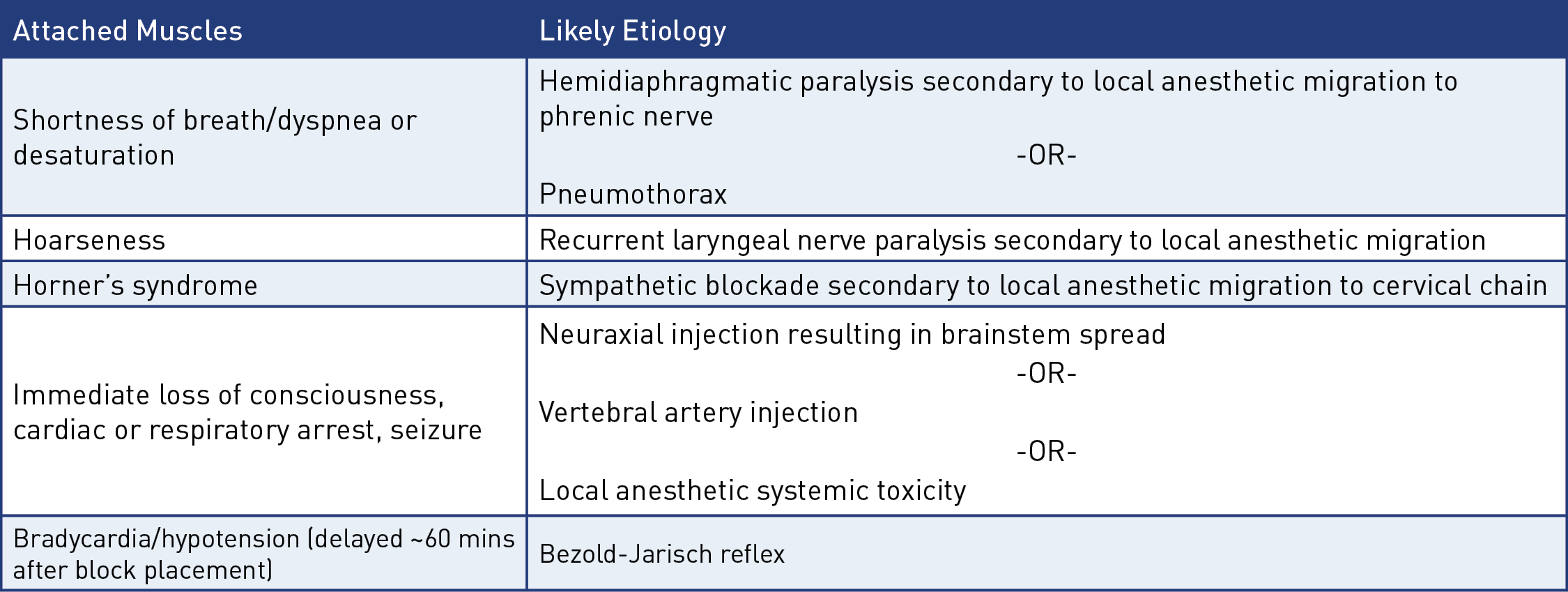
Osteotomes are shown in Figure 2. Expected dermatomal coverage of the interscalene block appears in Figure 3. Side effects and complications unique to the interscalene block are offered in Table 1.
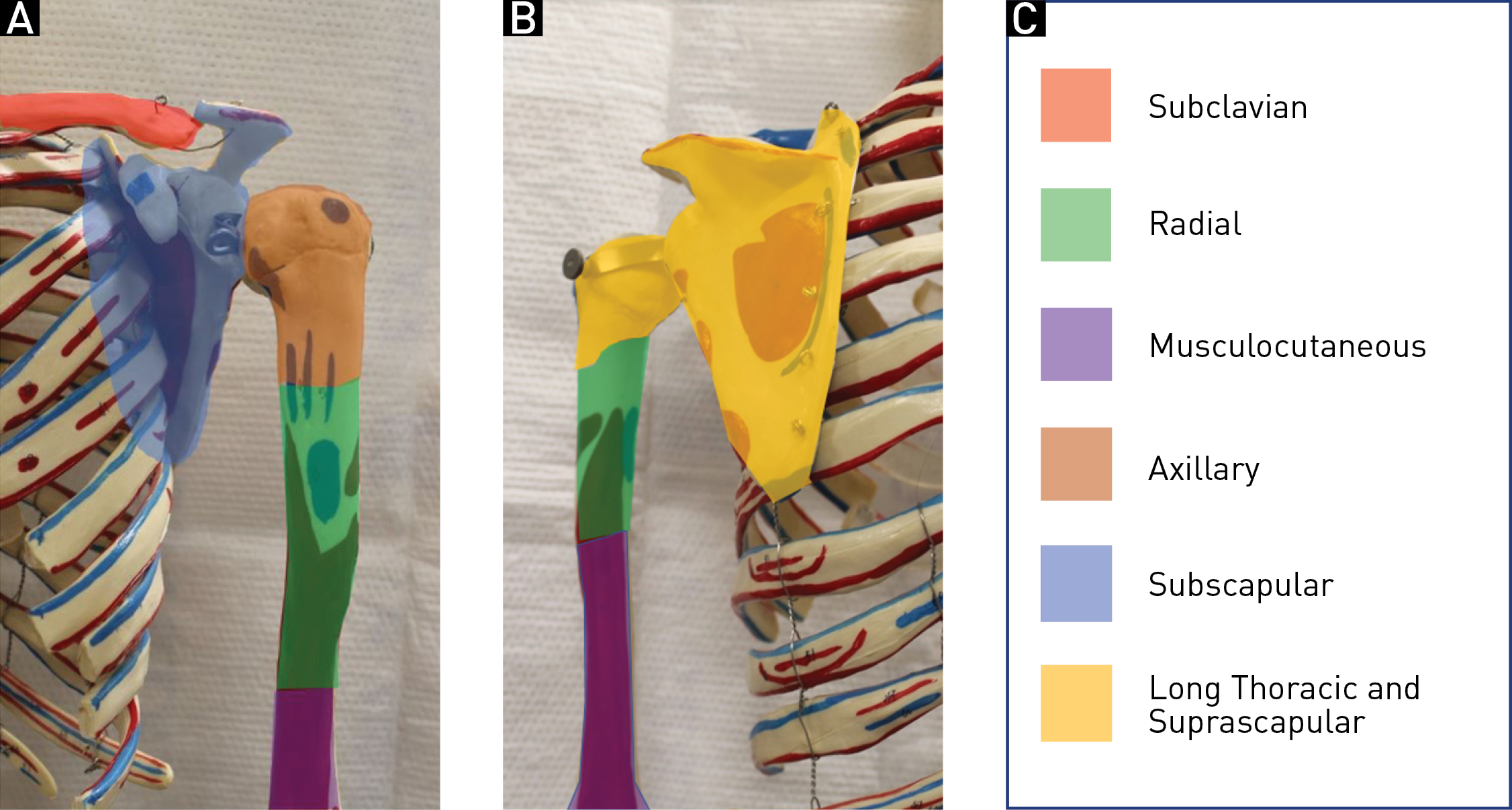
Figure 2: Osteotomes. 2A: Anterior. 2B: Posterior. 2C: Key
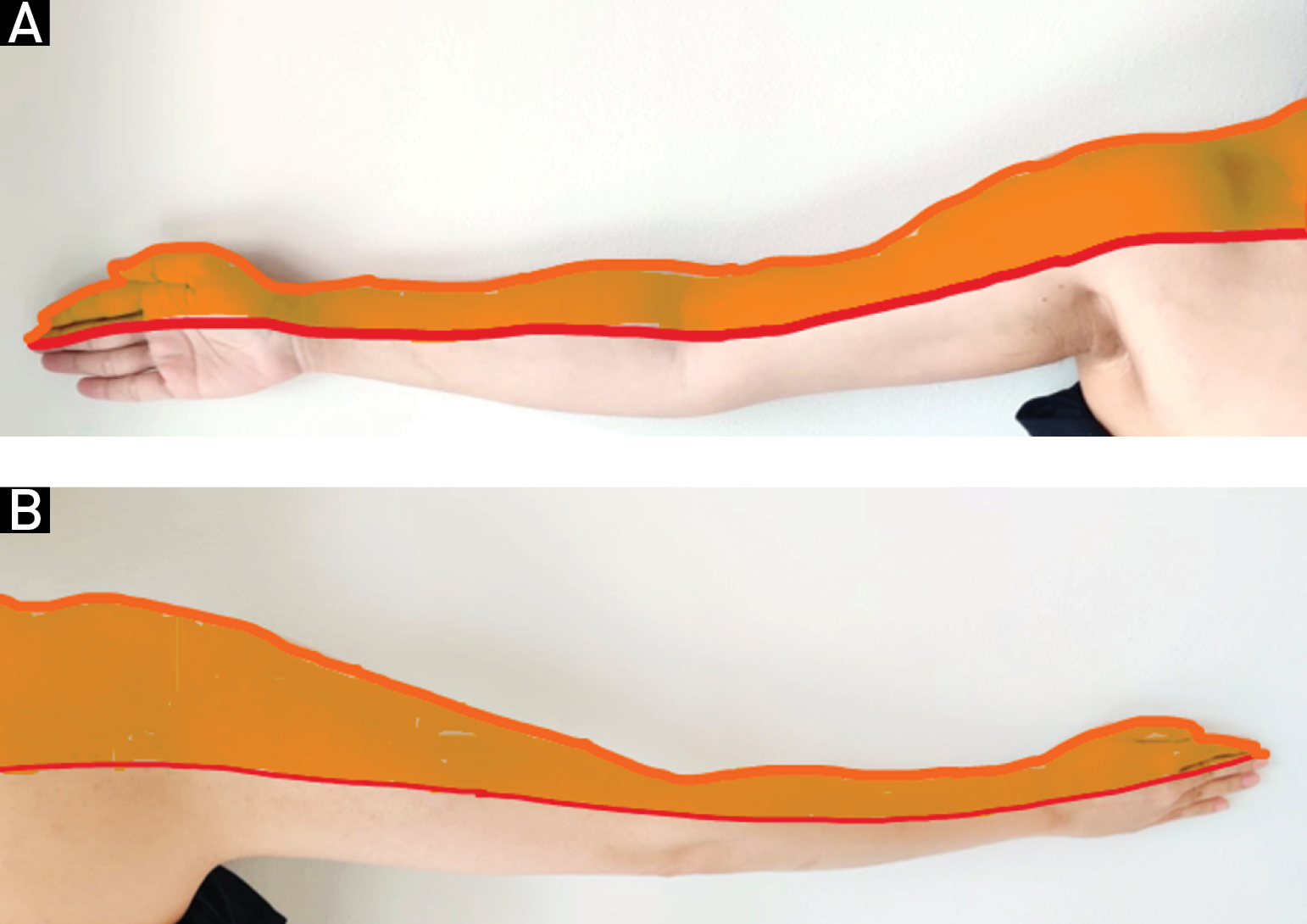
Figure 3: Expected dermatomal coverage of interscalene block. 3A: Anterior. 3B: Posterior.
Table 1: Potential side effects and complications of interscalene block.[3-5]
The proximity of the phrenic nerve to the brachial plexus at the level of the interscalene block, only about 1.8 mm from anatomic ultrasound studies,[6] leads to an almost certain phrenic nerve palsy on the side of the block. Arising from C3-C5 roots, the phrenic nerve crosses under the prevertebral fascia from the upper lateral border of the anterior scalene muscle and descends medially along the anterior scalene muscle toward its diaphragmatic target (Figure 4).
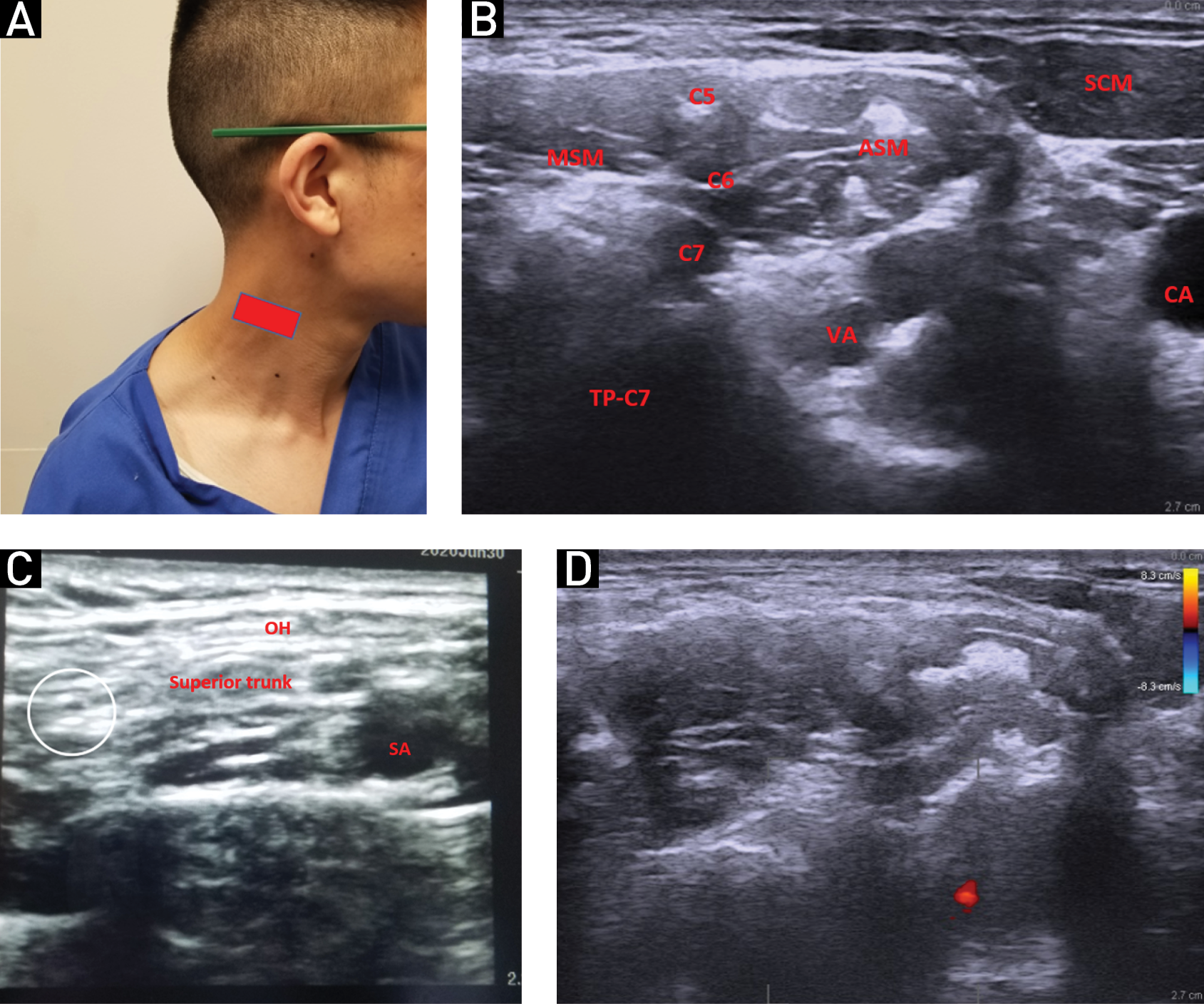
Figure 4: Phrenic nerve anatomy. 4A: Ultrasound probe position as the phrenic nerve is traced. 4B: At level of C6, phrenic nerve (green circle) lies laterally over the anterior scalene muscle, near the interscalene groove (red circle). 4C: As probe descends toward supraclavicular view, phrenic nerve has crossed medially
For healthy patients, transient hemidiaphragmatic palsy (HDP) is typically well tolerated, as accessory muscles compensate. Pulse oximetry is not a sensitive assessment, with values generally unchanged.[7] Bedside spirometry can be performed, ideally by comparing to baseline values obtained prior to block, and HDP is reflected by a decrease in forced expiratory volume in 1st second, forced vital capacity, and peak expiratory flow rate (PEFR). Ultrasound assessment is performed using a curvilinear probe oriented along the anterior axillary line on the left to image through the spleen or parasagittal midclavicular or anterior axillary line on the right to image through the liver. Once the diaphragm is identified, M-mode measurements are made with quiet breathing, deep breathing, and sniff (a rapid breath with closed mouth) (Figure 5). A partial phrenic nerve palsy will result in 25-75% reduction in caudal motion of the diaphragm.[7] The M-mode trace in a complete phrenic palsy shows >75% reduction in caudal motion or no active caudal movement of the diaphragm with inspiration and abnormal paradoxical movement (cranial movement on inspiration) particularly with the sniff test.
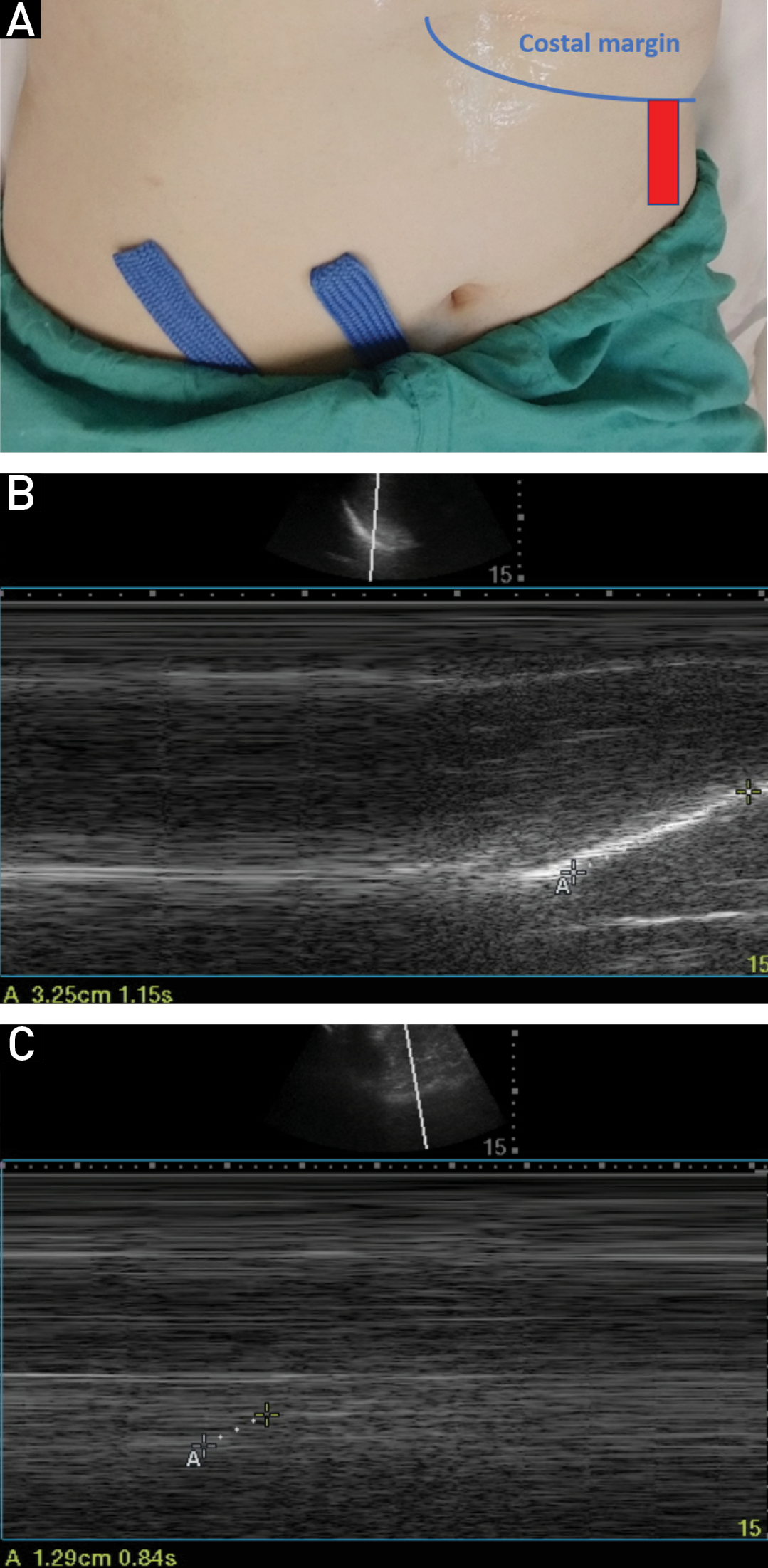
Figure 5: Ultrasound assessment and M-mode measurements. 5A: Location and orientation of ultrasound probe for left hemidiaphragmatic scan. 5B: Prior to interscalene block, sniff results in 3.25 cm excursion, consistent with normal diaphragmatic movement. 5C: After interscalene block, sniff results in 1.29 cm excursion, a 60% decrease consistent with partial phrenic nerve palsy
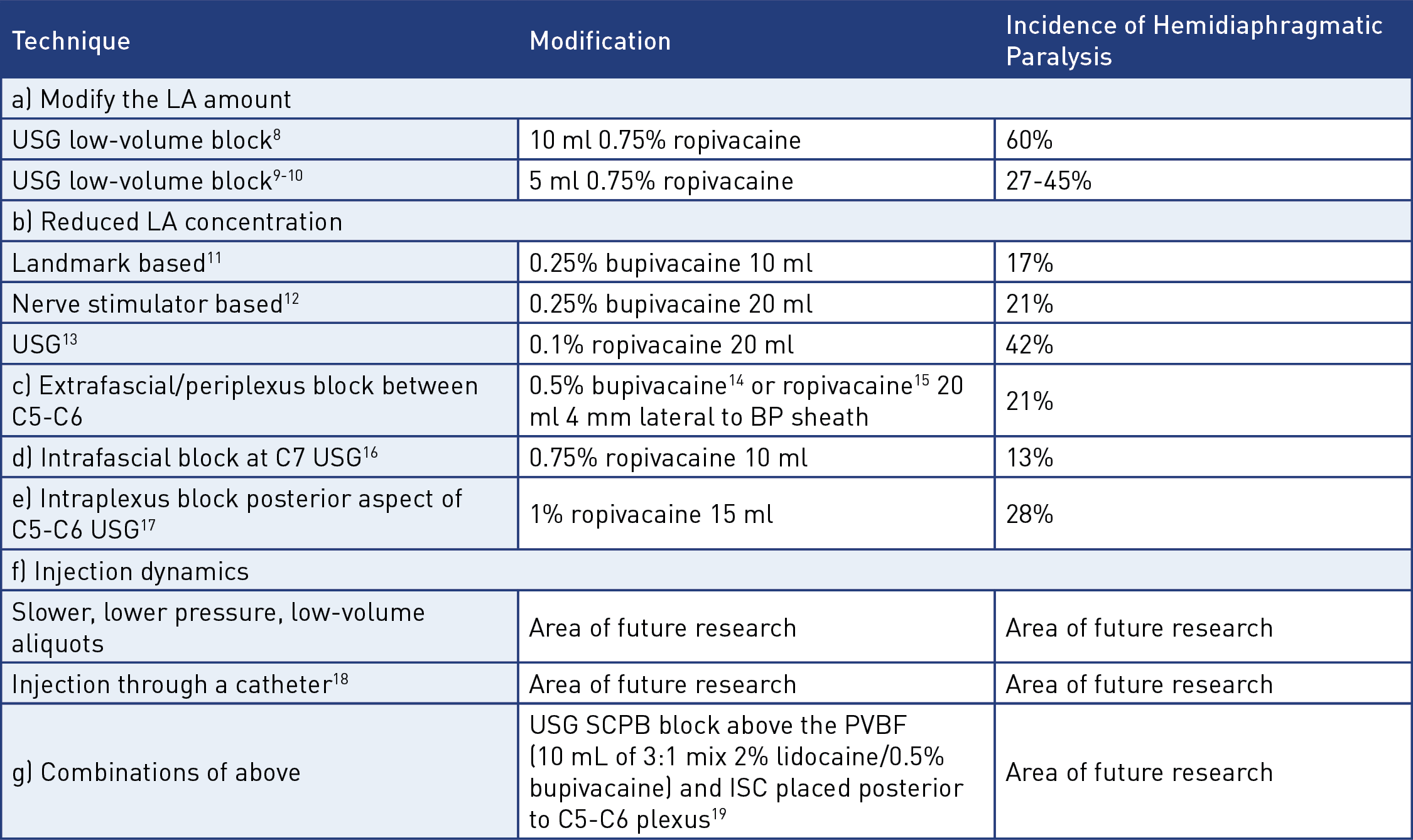
Table 2 addresses modifications of the interscalene block that attempt to reduce the incidence of HDP. Reducing the volume of the block to 5 mL will result in a 27-45% reduction of HDP but may necessitate the use of general anesthesia rather than sedation for the surgical procedure. Combinations of these modifications may further reduce the risk of HDP or increase the chance of avoidance of general anesthesia (ie, ultrasound-guided (USG) low-volume block with the catheter positioned posterior to the C5-C6 plexus to allow for additional titration of local anesthetic during surgery as needed).[19]
Table 2: Phrenic sparing options - modification of interscalene block.[8-19]
Though these reductions in HDP are significant, any risk could be unacceptable in a particularly complicated patient and an ideal alternative would be one in which the incidence of HDP approaches zero. Performing the block more peripherally, farther away from the level of roots, reduces the risk of phrenic nerve palsy, but attention must be given to the sensory contributors, particularly the suprascapular nerve as it branches off proximally from the superior trunk.
The suprascapular nerve can be blocked individually, either via an anterior approach, targeting the nerve as it branches off the superior trunk in a sub-omohyoid view, or via a posterior approach, targeting the nerve once it reaches the suprascapular notch of the scapula. Though the posterior approach to the suprascapular block offers inferior analgesia to the interscalene block, recent studies focusing on the anterior approach have demonstrated non-inferiority for the first 24 hours postoperatively, likely due to early articular branches that are missed when the block is performed more distally (posteriorly).[20-22] Unfortunately, the anterior approach appears to carry a higher risk of phrenic nerve palsy than the posterior approach.[23] Table 3 offers a review and comparison of alternatives to interscalene block.
Table 3: Review of alternatives to interscalene block.[24-34]
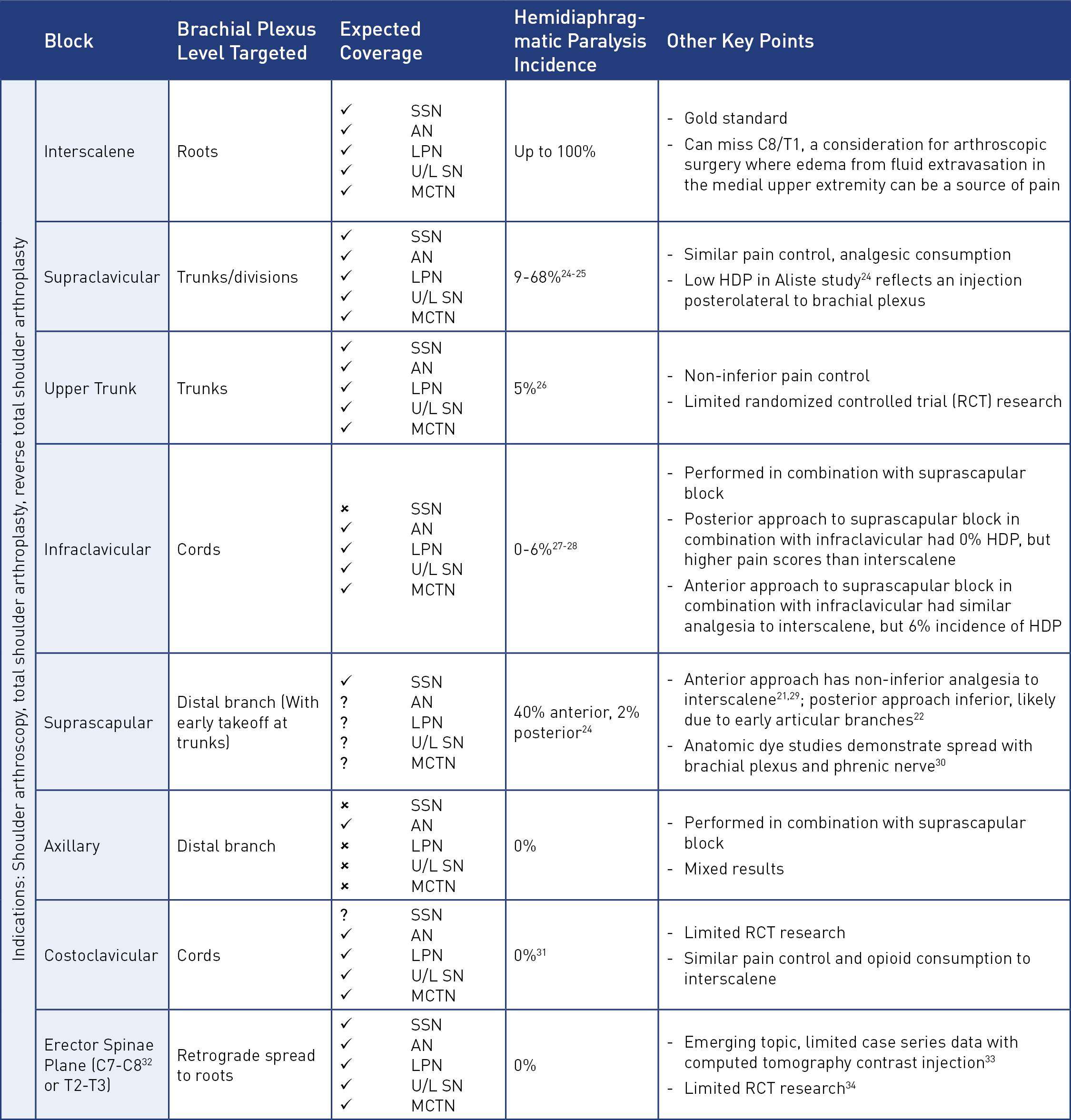
SSN, suprascapular nerve; AN, axillary nerve; LPN, lateral pectoral nerve; U/L SN, upper and lower subscapular nerve; MCTN, musculocutaneous nerve; HDP, hemidiaphragmatic paralysis.
Our Experience
Single shot vs. catheter: Patients undergoing shoulder arthroscopy are offered an interscalene catheter (ISC) or single shot interscalene block depending on patient preference. Patients having total shoulder arthroplasties or complicated joint repairs are encouraged to choose an interscalene catheter.
Some practitioners choose to add perineural dexamethasone to local anesthetic or use liposomal bupivacaine in their single shot block. Adjuvants such as buprenorphine, clonidine, dexmedetomidine, and magnesium, though promising for prolongation of single shot blocks,[35] are not routinely used at our institution (Table 4).
Table 4: Regional anesthesia block protocol Mount Sinai West-Mount Sinai Morningside for shoulder surgeries.
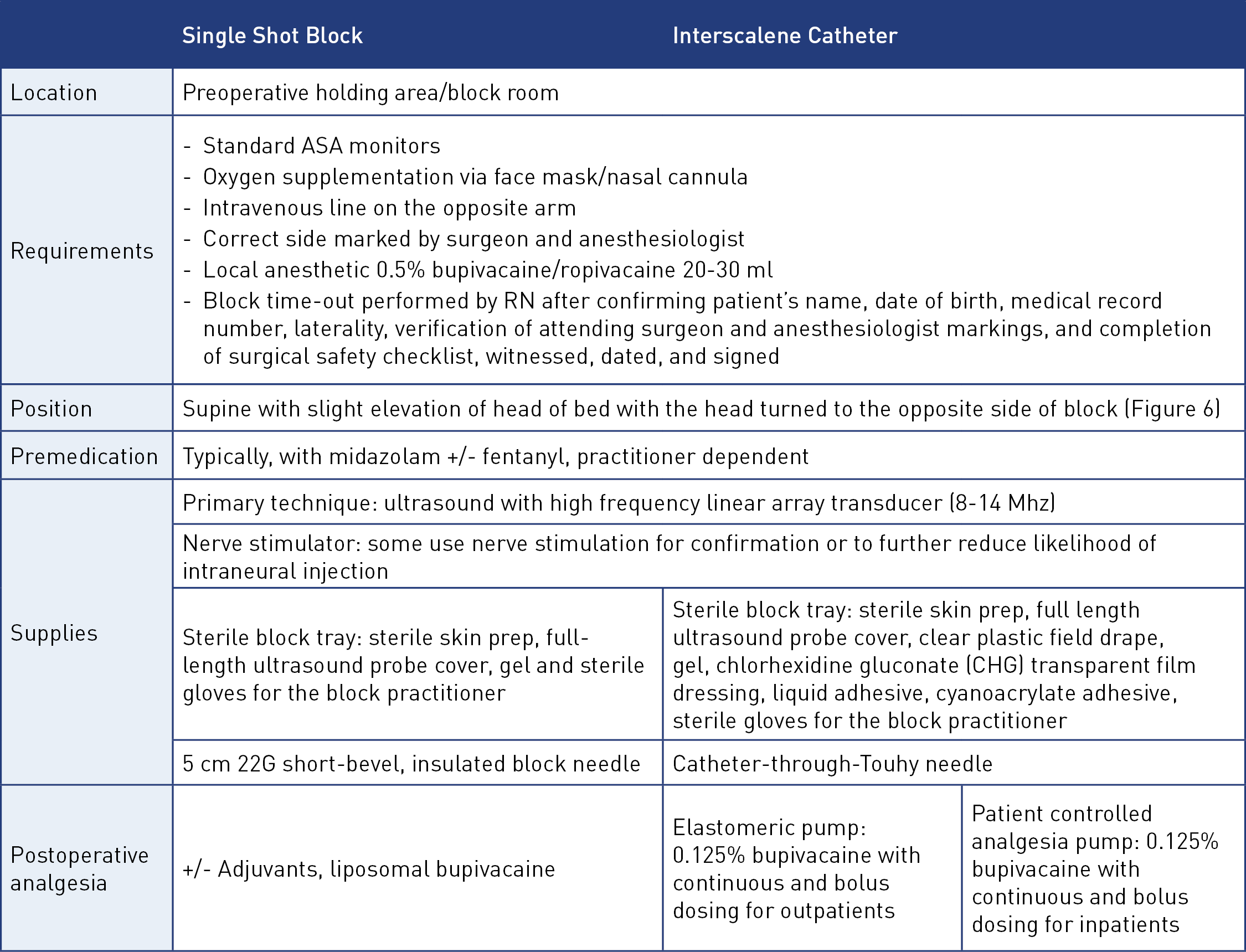

Figure 6: Scanning positioning
Scanning technique and injection: The probe is positioned approximately at the level of the cricoid cartilage (C6) in a transverse orientation, lateral to the sternocleidomastoid muscle (Figure 7A). Anterior and middle scalene muscles are identified, with the interscalene groove in between (Figure 7B). If landmarks are not immediately apparent, the probe is either moved medially to identify the carotid artery and internal jugular vein before scanning back laterally or slid down to the supraclavicular fossa to identify the supraclavicular view, where trunks may then be traced back up to their interscalene origin (Figure 7C). A slight caudal tilt of the probe is often helpful to bring the nerve roots into clearest view.
Careful attention is paid to the surrounding vasculature, particularly the vertebral artery, arteries of the thyrocervical trunk, and external jugular vein (which also runs along the lateral border of the sternocleidomastoid). Color flow Doppler may be used to verify (Figure 7D). The block is performed in plane from a lateral to medial approach or out of plane in a cephalad to caudad orientation depending on patient anatomy and practitioner preference, with path of needle selected to avoid traversing the external jugular vein with the Tuohy needle or catheter.
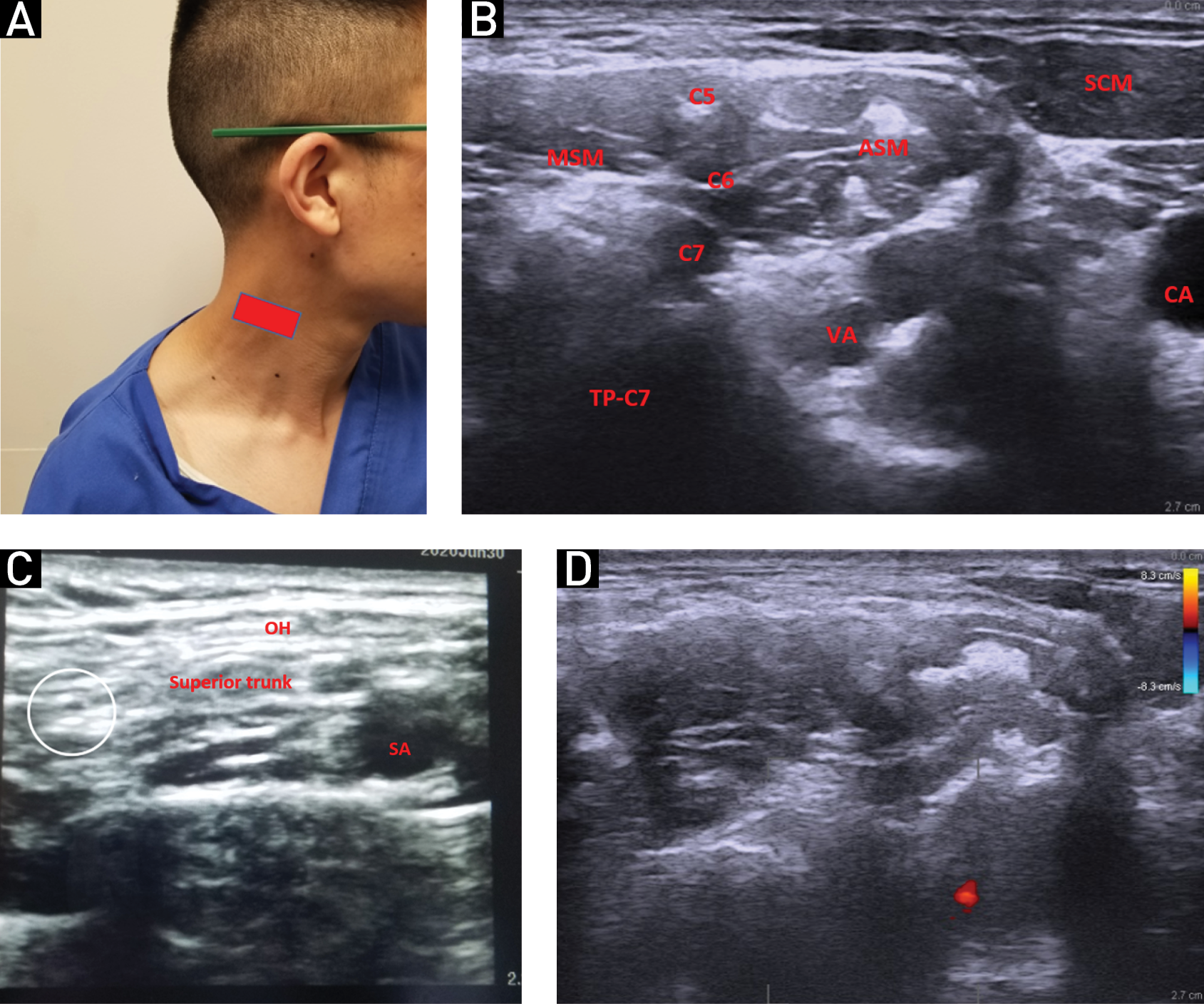
Figure 7: Interscalene block. 7A: Ultrasound probe position. 7B: Classic view at cricoid level with C5, (split) C6, and C7 root visible. 7C: Supraclavicular view (note that the suprascapular nerve is visible as it leaves the superior trunk [white circle]). 7D: Color flow Doppler of vertebral artery
MSM, middle scalene muscle; ASM, anterior scalene muscle; VA, vertebral artery; SCM, sternocleidomastoid; SA, subclavian artery; OH, omohyoid; CA, carotid artery; TP-C7, transverse process of C7.
The needle tip is targeted to end up through the prevertebral fascia, between roots of the brachial plexus (Figure 8A). After negative aspiration, local anesthetic is injected with attention to the spread of local along the interscalene groove (Figure 8B). Local anesthetic spread may be tracked down to the upper trunk. Volumes of 20-30 mL of 0.5% ropivacaine or bupivacaine are routinely used, with volume depending on visualization of spread, weight/comorbidities of patient, and practitioner. Patients are then brought to the operating room, where monitored anesthesia care is administered after additional surgical infiltration to cover posterior scope insertion ports for arthroscopy or general anesthesia is induced and airway is secured either with a laryngeal mask airway or an endotracheal tube, with a goal of spontaneous ventilation[36] for patients in a beach chair position.
When a catheter is utilized, efforts are made to see the entire path of the catheter terminating in the interscalene groove, or to clearly see spread of local anesthetic along the brachial plexus sheath with injection of air or local anesthetic (Figure 8C). A typical depth of securement is 6-8 cm, and our catheters are usually not tunneled. The insertion site is plugged with cyanoacrylate adhesive, and liquid adhesive is used to provide additional adherence for a chlorhexidine gluconate impregnated transparent film dressing. The length of the catheter is secured above the clavicle so as to avoid interference with the surgical field.
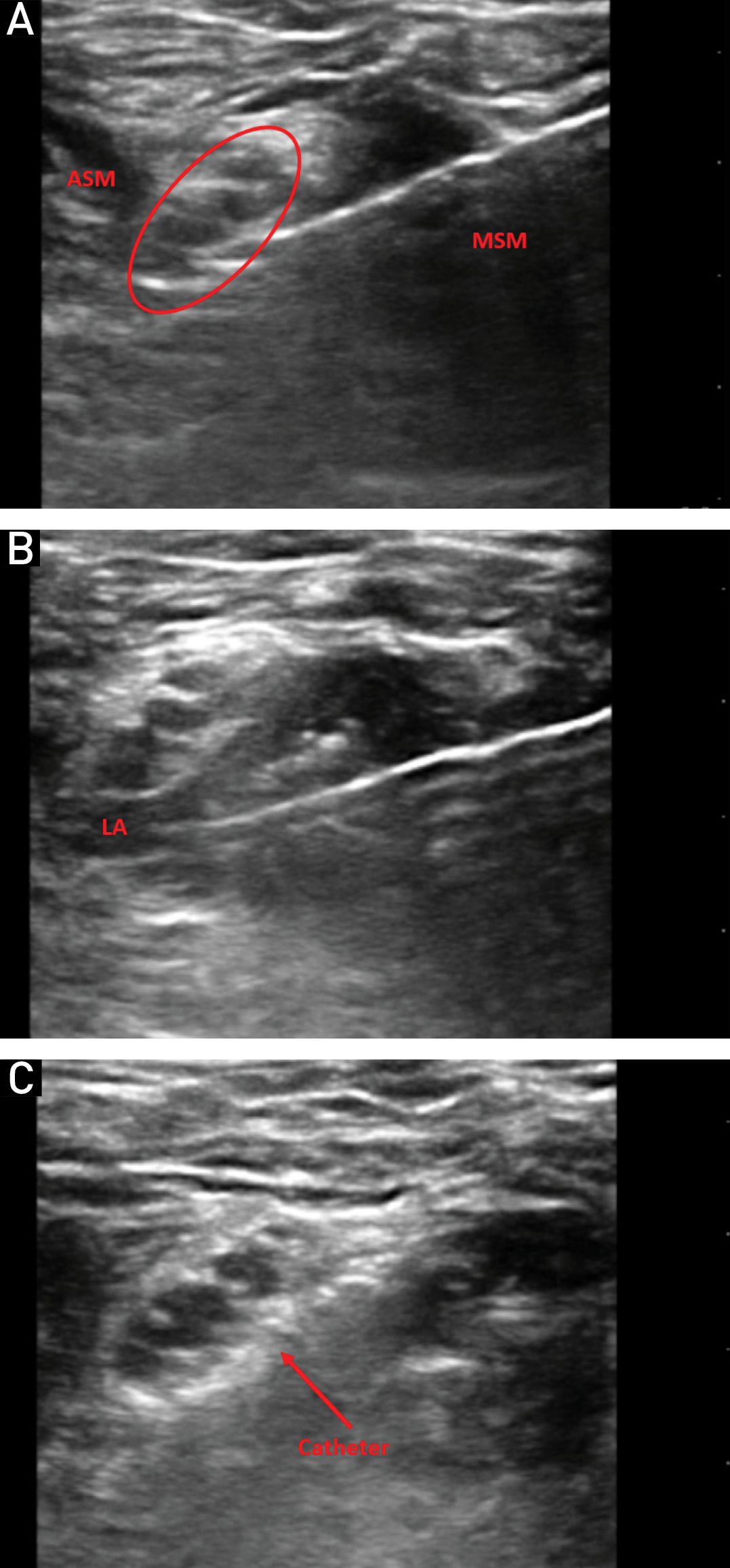
Figure 8: Interscalene catheter insertion. 8A:Tuohy needle approaching target roots (circled). 8B: After injection of local anesthetic. 8C: Catheter visualized
MSM, middle scalene muscle; ASM, anterior scalene muscle; LA, local anesthetic.
Catheter dosing, management, and follow up: Patients are typically discharged on the same day after arthroscopy or on the first postoperative day following TSA. Discharged patients with continuous interscalene catheters are sent home with an elastomeric pump, providing 0.125% bupivacaine via continuous and patient-controlled analgesia (PCA) bolus dosing options for approximately 48 hours. They are followed with a daily postoperative phone call from their anesthesia team and are provided with thorough catheter care and removal instructions, as well as a direct phone number that allows them to reach the on-call anesthesiologist at any time. Inpatients are followed by the acute pain service and are also managed with a continuous and PCA bolus regimen of 0.1% bupivacaine. Depending on hospital length of stay, the catheter may be removed by the acute pain team prior to discharge or patients may be discharged with an elastomeric pump.
There are two types of perineural catheters: catheter-through-needle or catheter-over-needle. Common complications for catheter-through-needle include dislodgement of the alligator clip, leakage at the insertion site, difficulty in visualizing catheter tip on ultrasound, and accidental removal of the catheter during positioning or movement. Complications for catheter-over-needle include catheter migration, especially if an incorrect length of catheter was chosen, which is usually apparent during catheter insertion. Inadequate analgesia is treated with additional boluses of local anesthetic or oral/IV opioids and catheter replacement, if needed. Patients are also discharged with an oral opioid prescription, in the event of inadequate analgesia or breakthrough pain.
Assessment of patient satisfaction is an important outcome measurement and indicator of quality of anesthesia care. Several studies have shown higher satisfaction scores in patients who underwent shoulder surgeries with an interscalene block. Other advantages to interscalene block in shoulder surgeries include a reduced incidence of postoperative nausea and vomiting and decreased opioid consumption. In our experience, incorporating interscalene block as an analgesic modality for shoulder surgery provides many additional potential benefits including facilitating post-anesthesia care unit (PACU) bypass, preventing PACU delays, facilitating early discharge, and reducing costs.[37] Based on our experience, interscalene block is an invaluable regional anesthetic tool for shoulder surgeries performed at our hospital. Interscalene block is easy to perform and relatively safe, and it should be a staple of every practitioner’s armamentarium of blocks.
References
- López-Valverde A, De Vicente J, Cutando A. The surgeons Halsted and Hall, cocaine and the discovery of dental anesthesia by nerve blocking. Br Dent J. 2011;211(10):485-7. https://doi.org/10.1038/sj.bdj.2011.961
- Wordliczek J, Jakowicka-Wordliczek J, Zajaczkowska R. Henryk Hilarowicz: the forgotten Polish inventor and pioneer of the interscalene brachial plexus block. J Anesth Hist. 2018;4(1):11-7. https://doi.org/10.1016/j.janh.2018.01.001
- Tran DQH, Elgueta MF, Asenjo JF. Upper extremity nerve blocks. In: Kaye A, Urman R, Vadivelu N. Essentials of Regional Anesthesia. Springer International Publishing; 2018. https://doi.org/10.1007/978-3-319-74838-2
- D'Alessio JG, Weller RS, Rosenblum M. Activation of the Bezold-Jarisch reflex in the sitting position for shoulder arthroscopy using interscalene block. Anesth Analg. 1995;80(6):1158-62. https://doi.org/10.1097/00000539-199506000-00016
- Dutton RP, Eckhardt WF, Sunder N. Total spinal anesthesia after interscalene blockade of the brachial plexus. Anesthesiology. 1994;80(4):939-41. https://doi.org/10.1097/00000542-199404000-00028
- Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: implications for the interscalene brachial plexus block. Reg Anesth Pain Med. 2008;33(6):545-50.
- El-Boghdadly K, Chin KJ, Chan VWS. Phrenic nerve palsy and regional anesthesia for shoulder surgery: anatomical, physiologic, and clinical considerations. Anesthesiology. 2017;127(1):173-91. https://doi.org/10.1097/ALN.0000000000001668
- Lee JH, Cho SH, Kim SH, et al. Ropivacaine for ultrasound-guided interscalene block: 5ml provides similar analgesia but less phrenic nerve paralysis than 10 mL. Can J Anaesth. 2011;58(11):1001–6. https://doi.org/10.1007/s12630-011-9568-5
- Stundner O, Meissnitzer M, Brummett CM, et al. Comparison of tissue distribution, phrenic nerve involvement, and epidural spread in standard- vs low-volume ultrasound-guided interscalene plexus block using contrast magnetic resonance imaging: a randomized, controlled trial. Br J Anaesth.2016;116(3):405–12. https://doi.org/10.1093/bja/aev550
- Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJL. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008;101(4):549-56. https://doi.org/10.1093/bja/aen229
- Al-Kaisy AA, Chan VW, Perlas A. Respiratory effects of low-dose bupivacaine interscalene block. Br J Anaesth. 1999;82(2):217-20. https://doi.org/10.1093/bja/82.2.217
- Thackeray EM, Swenson JD, Gertsch MC, et al. Diaphragm function after interscalene brachial plexus block: A double-blind, randomized comparison of 0.25% and 0.125% bupivacaine. JShoulder Elbow Surg. 2013;22(3):381–6. https://doi.org/10.1016/j.jse.2012.06.011
- Wong AK, Keeney LG, Chen L, Williams R, Liu J, Elkassabany NM. Effect of local anesthetic concentration (0.2% vs 0.1% ropivacaine) on pulmonary function and analgesia after ultrasound-guided interscalene brachial plexus block: a randomized controlled study. Pain Med. 2016;17(12):2397-403. https://doi.org/10.1093/pm/pnw057
- Palhais N, Brull R, Kern C, et al. Extrafascial injection for interscalene brachial plexus block reduces respiratory complications compared with a conventional intrafascial injection: a randomized, controlled, double-blind trial. Br J Anaesth.2016;116(4):531-7. https://doi.org/10.1093/bja/aew028
- Ayyanagouda B, Hosalli V, Kaur P, Ambi U, Hulkund SY. Hemidiaphragmatic paresis following extrafascial versus conventional intrafascial approach for interscalene brachial plexus block: a double-blind randomised, controlled trial. Indian J Anaesth. 2019;63(5):375–81.
- Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009;34(5):498–502. https://doi.org/10.1097/AAP.0b013e3181b49256
- Bergmann L, Martini S, Kesselmeier M, et al. Phrenic nerve block caused by interscalene brachial plexus block: breathing effects of different sites of injection. BMC Anesthesiol. 2016;16(1):45. https://doi.org/10.1186/s12871-016-0218-x
- Borgeat A, Perschak H, Bird P, Hodler J, Gerber C. Patient controlled interscalene analgesia with ropivacaine 0.2% versus patient-controlled intravenous analgesia after major shoulder surgery: effects on diaphragmatic and respiratory function. Anesthesiology. 2000;92(1):102–8. https://doi.org/10.1097/00000542-200001000-00020
- Ip V, Achen B, Nagendran J. Subclavian transcatheter aortic valve implantation (TAVI): superficial cervical plexus block combined with low-dose interscalene block. Can J Anesth. 2020;67(10):1389-92. https://doi.org/10.1007/s12630-020-01764-8
- Tran DQ, Layera S, Bravo D, Cristi-Sanchez I, Bermudez L, Aliste J. Diaphragm-sparing nerve blocks for shoulder surgery, revisited. Reg Anesth Pain Med. 2020;45:73-8. https://doi.org/10.1136/rapm-2019-100908
- Abdallah FW, Wijeysundera DN, Laupacis A, et al. Subomohyoid anterior suprascapular block versus interscalene block for arthroscopic shoulder surgery: a multicenter randomized trial. Anesthesiology. 2020;132(4):839-53. https://doi.org/10.1097/ALN.0000000000003132
- Ebraheim NA, Whitehead JL, Alla SR, et al. The suprascapular nerve and its articular branch to the acromioclavicular joint: an anatomic study. J Shoulder Elbow Surg. 2011;20(2):e13-7. https://doi.org/10.1016/j.jse.2010.09.004
- Ferré F, Pommier M, Laumonerie P, et al. Hemidiaphragmatic paralysis following ultrasound-guided anterior vs. posterior suprascapular nerve block: a double-blind, randomised control trial. Anaesthesia. 2020;75(4):499-508. https://doi.org/10.1111/anae.14978
- Aliste J, Bravo D, Fernández D, Layera S, Finlayson RJ, Tran DQ. A randomized comparison between interscalene and small-volume supraclavicular blocks for arthroscopic shoulder surgery. Reg Anesth Pain Med. 2018;43(6):590-5. https://doi.org/10.1097/AAP.0000000000000767
- Koh WU, Kim HJ, Park HS, Choi WJ, Yang HS, Ro YJ. A randomised controlled trial comparing continuous supraclavicular and interscalene brachial plexus blockade for open rotator cuff surgery. Anaesthesia. 2016;71(6):692-9. https://doi.org/10.1111/anae.13419
- Kim DH, Lin Y, Beathe JC, et al. Superior trunk block: a phrenic-sparing alternative to the interscalene block: a randomized controlled trial. Anesthesiology. 2019;131(3):521-33. https://doi.org/10.1097/ALN.0000000000002841
- Aliste J, Bravo D, Finlayson RJ, Tran DQ. A randomized comparison between interscalene and combined infraclavicular-suprascapular blocks for arthroscopic shoulder surgery. Can J Anaesth. 2018;65(3):280-7. https://doi.org/10.1007/s12630-017-1048-0
- Taha AM, Yurdi NA, Elahl MI, Abd-Elmaksoud AM. Diaphragm-sparing effect of the infraclavicular subomohyoid block vs low volume interscalene block. A randomized blinded study. Acta Anaesthesiol Scand. 2019;63(5):653-8. https://doi.org/10.1111/aas.13322
- Auyong DB, Hanson NA, Joseph RS, Schmidt BE, Slee AE, Yuan SC. Comparison of anterior suprascapular, supraclavicular, and interscalene nerve block approaches for major outpatient arthroscopic shoulder surgery: a randomized, double-blind, noninferiority trial. Anesthesiology. 2018;129(1):47–57. https://doi.org/10.1097/ALN.0000000000002208
- Sehmbi H, Johnson M, Dhir S. Ultrasound-guided subomohyoid suprascapular nerve block and phrenic nerve involvement: a cadaveric dye study. Reg Anesth Pain Med. 2019;44(5):561–4. https://doi.org/10.1136/rapm-2018-100075
- Aliste J, Bravo D, Layera S, et al. Randomized comparison between interscalene and costoclavicular blocks for arthroscopic shoulder surgery. Reg Anesth Pain Med. 2019;44:472–7. https://doi.org/10.1136/rapm-2018-100055
- Tsui BCH, Sun LY, Ip VHY, Malik MF, Ince I, Elsharkawy H. Diaphragm-sparing erector spinae plane block for shoulder surgery: emerging evidence. Reg Anesth Pain Med. 2020;rapm-2020-101599. https://doi.org/10.1136/rapm-2020-101599
- Diwan S, Nair A. Erector spinae plane block for proximal shoulder surgery: a phrenic nerve sparing block! Turk J Anaesthesiol Reanim. 2020;48(4):331-3. https://doi.org/10.5152/TJAR.2019.55047
- Sun L, Basireddy S, Gerber L, et al. Erector spinae plane block for total shoulder arthroplasty avoids phrenic nerve complication: a randomized trial. 45th annual regional anesthesiology and acute pain medicine (ASRA) meeting. San Francisco, 2020. Available: https://epostersonline.com/ASRASPRING20/node/308
- Kirksey MA, Haskins SC, Cheng J, Liu S. Local anesthetic peripheral nerve block adjuvants for prolongation of analgesia: a systematic qualitative review. PLoS One. 2015;10(9):e0137312. https://doi.org/10.1371/journal.pone.0137312
- Orebaugh S, Palmeri S, Lin C, YaDeau J. Daring discourse: is nerve block with sedation the safest anesthetic for beach chair position? Reg Anesth Pain Med. 2019;44(7):707-12. https://doi.org/10.1136/rapm-2018-100230
- Hadzic A, Williams BA, Karaca PE, et al. For outpatient rotator cuff surgery, nerve block anesthesia provides superior same-day recovery over general anesthesia. Anesthesiology.2005;102(5):1001-7. https://doi.org/10.1097/00000542-200505000-00020
Leave a commentOrder by
Newest on top Oldest on top