Naloxone for the Pain Physician: What Do I Need to Know?
According to the Centers for Disease Control (CDC), health care providers wrote 259 million prescriptions for opioid or narcotic painkillers in 2012.1 Although these medications have a true therapeutic value for some individuals who suffer from intense pain, the incidence of misuse, abuse, and overdose from opioid medications has been steadily rising over the years. The opioid epidemic has become a public health crisis in the United States and is associated with devastating consequences. For example, opioid overdose has overtaken motor vehicle crashes as the number one cause of injury death in the United States.2 Since 2016, opioid overdose has increased by 30% in 45 states.3 Almost a third of patients prescribed opioids for chronic pain misuse them,4 and approximately 10% will develop an opioid use disorder.4 In 2017 alone, more than 70,000 people died of drug overdose (21.7 per 100,000).2 The majority (68%) of these deaths involved a prescribed or illicit opioid, and the number of opioid-related overdose deaths has continued to rise (eg, six times higher than in 1999).2,5
As naloxone has become easier to prescribe and for patients or caregivers to obtain, it is vital for physicians to educate patients about its potential life-saving qualities.
Misuse also can be entirely unintentional, especially for older individuals. Serious memory issues, dementia, or Alzheimer’s disease can exacerbate overdose risk; thus it is important for caregivers to carefully monitor their loved ones’ medications. Polypharmacy, or the use of multiple medications to manage coexisting health problems, also makes it difficult to responsibly manage prescriptions such as opioid painkillers. A study from the Centers for Disease Control and Prevention (CDC) revealed that 76% of Americans aged 60 and older use two or more prescription drugs and 37% use five or more.6 Additionally, many prescription and nonprescription medications, supplements, and vitamins can have significant side effects and interactions with one another. Adding alcohol to this mix increases the risk of an adverse reaction or overdose even further.
It is vital for both patients and physicians to engage in serious discussions about these medications when they are prescribed. This includes conversing about the proper way to take these medicines, acknowledging drug and alcohol interactions, and learning how to recognize and respond to an accidental overdose. "This can be an uncomfortable conversation to have," says Dr Anita Gupta, vice-chair and associate professor at Drexel University College of Medicine and co-chair of the American Society of Anesthesiologist’s Anesthetic and Analgesic Drugs Products Advisory Committee.
Part of this discussion should include education about signs of potential overdose. According to the World Health Organization, a combination of three specific signs can indicate an opioid emergency. This is known as the “opioid overdose triad” and includes slowed or even stopped breathing (respiratory depression), loss of consciousness, and very small pupils. Of growing interest is whether naloxone (an opioid antagonist) should also be part of this discussion.
In 2016, CDC Guidelines for Prescribing Opioids for Chronic Pain recommended considering co-prescribing naloxone in patients at high risk for overdose, such as those who are prescribed ≥ 50 morphine milligram equivalents (MME), are concurrently taking benzodiazepines, or have a history of overdose or substance use disorder (SUD).7 In addition, those at risk may include patients with medical comorbidities including concomitant respiratory, hepatic, or renal dysfunction.7 Social factors also may place patients at higher risk for opioid overdose including having been recently released from incarceration or a medication assist program or having difficulty accessing medical services.7 For those at risk, naloxone can be life-saving. In fact, the CDC reports that naloxone has reversed more than 10,000 opioid overdoses since 2014.5 Despite the CDC’s recommendation, co-prescription of naloxone with opioids only increased from 1.5 to 4.6 per 1,000 patients from 2016 to 2017 (Medicare Part D data).8 Evidence also suggests that state-mandated MME/day threshold guidelines can increase naloxone prescribing; however, at this time only Virginia and Vermont have enacted such policies.8 Despite this data, overall naloxone prescribing appears to remain low according to Morbidity and Mortality Weekly Report (MMWR) Vital Signs.9 Although there have been tremendous strides in recent years with a more than 100% increase in naloxone prescribing from 2017 to 2018 alone, it appears to still be under-prescribed. For example, in 2018 only 1 naloxone prescription was prescribed for every 69 high-dose opioid prescriptions written.9
To improve naloxone co-prescription with opioids, further information is required regarding naloxone prescribing patterns and perceived prescribing barriers. There are varied opinions as to the actual risks and benefits of naloxone that may lead to under-prescribing. Opponents of naloxone believe that possession of an antidote leads to more widespread opioid misuse. News reports suggest the first responders are called to treat the same victim multiple times, thus questioning if naloxone is contributing to rather than alleviating the problem. Advocates, however, suggest that each naloxone reversal gives an opportunity for the recipient to seek a chance at recovery, thus reducing harmful consequences such as death, infection, or incarceration. Developing a greater understanding of naloxone may be beneficial in alleviating controversies in this debate.
What Is Naloxone?
Naloxone is a lipophilic non-selective compound that is a competitive opioid antagonist. It has high binding affinity for the mu opioid receptor.10 It was first approved by the Food and Drug Administration (FDA) in 1971.11
Naloxone is highly effective at reducing overdose if administered at the time of an overdose. While it can take 1-3 hours to develop respiratory depression following an opioid overdose, naloxone works within minutes to decrease or reverse the effects of opioids.10, 12 Although naloxone’s duration of action is short (20-90 minutes), it may allow time for help to arrive.10,13 Naloxone is safe to use even in the absence of opioids (alleviating concern of administration to someone suspected of opioid overdose who is actually suffering from an unrelated medical disorder) and easy to administer.14,15 It is available in different FDA-approved forms including an autoinjector, an intranasal device, and an injectable form. It is also available in a non-FDA approved formulation as a nasal spray (Figures 1-4).16,17
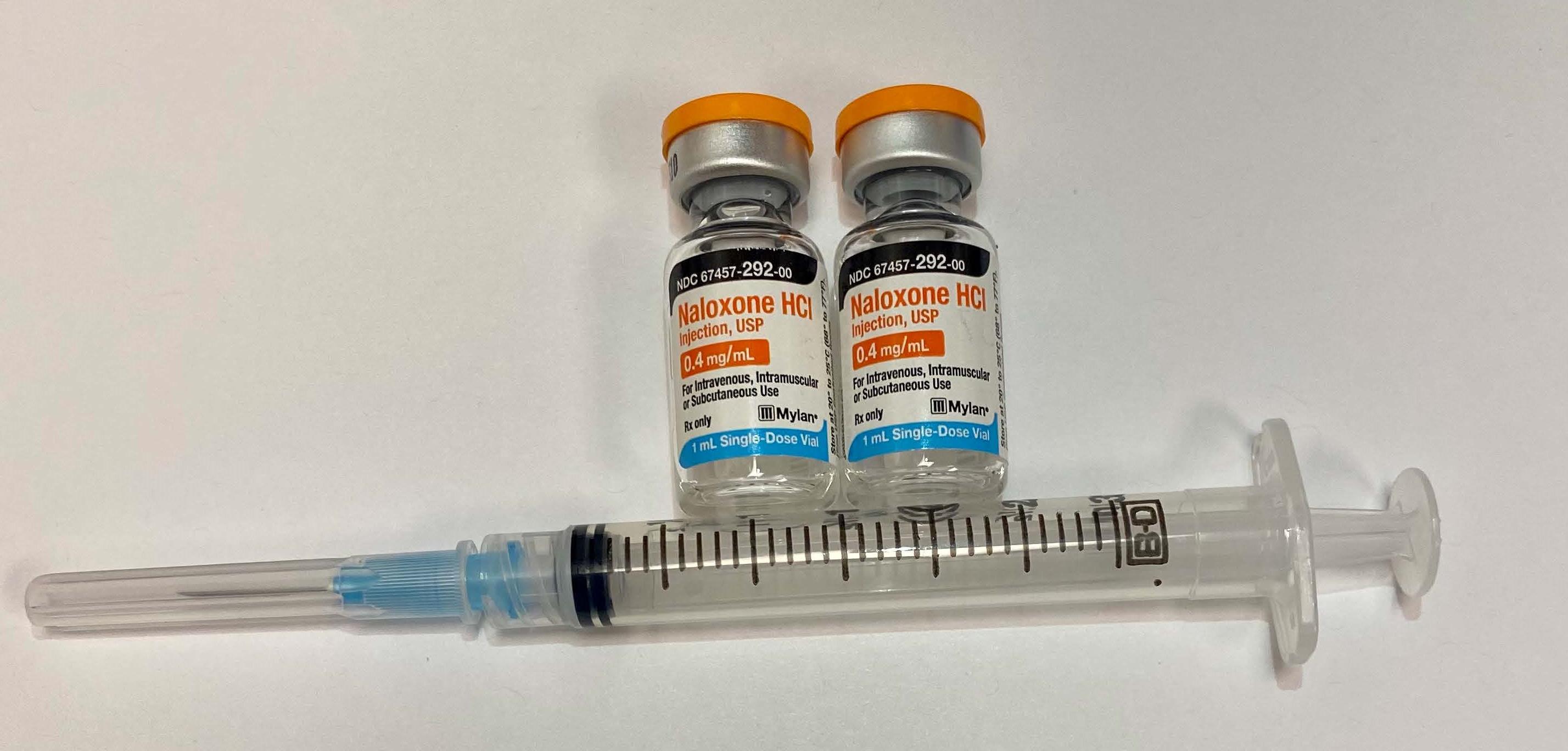
Figure 1. Injectable Naloxone
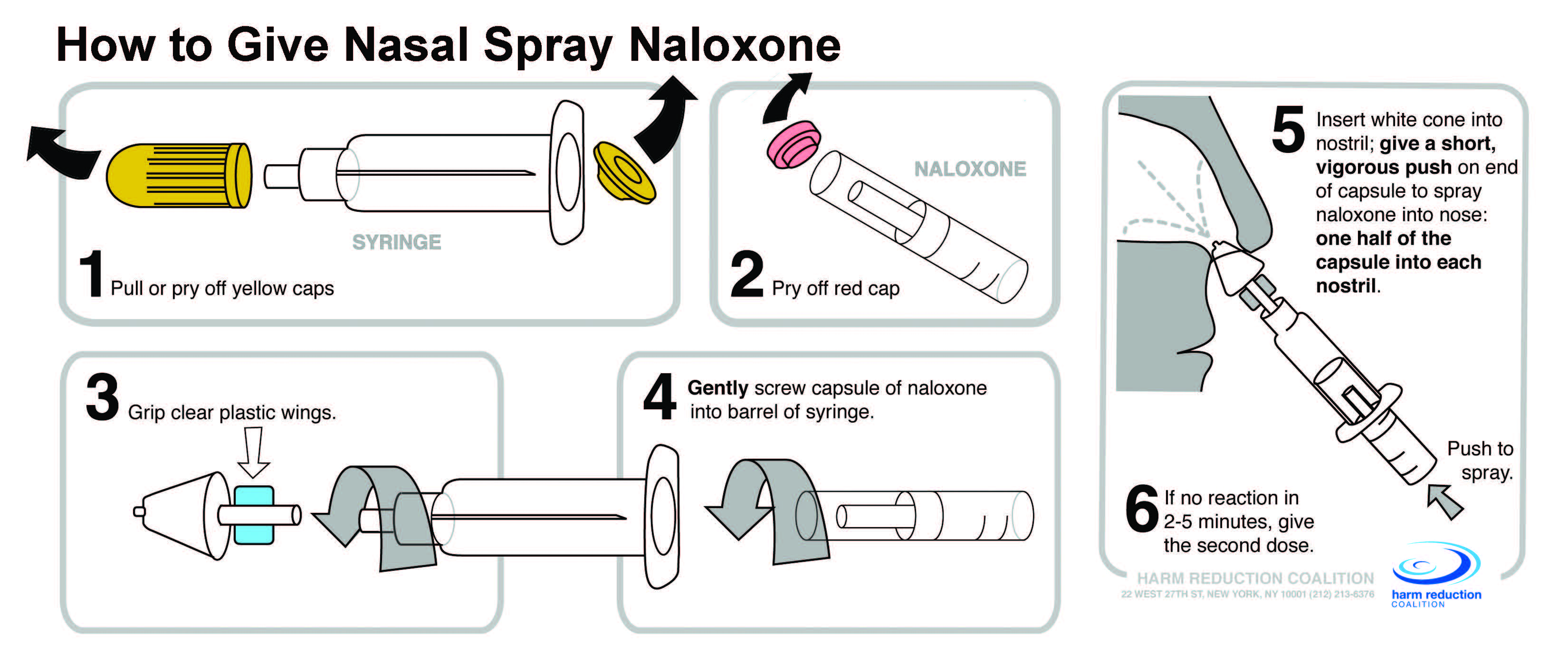 Figure 2. Nasal Spray Naloxone (reprinted with permission from harmreduction.com)
Figure 2. Nasal Spray Naloxone (reprinted with permission from harmreduction.com)
Figure 3. Adapt Autoinjector Nasal Spray Naloxone (reprinted with permission from Adapt Pharma Inc.)
Figure 4. Evzio Autoinjector Naloxone (Reprinted with permission from Kaelo, Inc.)
Naloxone allergy is the only true contraindication.18 Certain situations such as suspected overdose with partial agonists or mixed agonist/antagonists deserve caution, as reversal may take longer and higher doses of naloxone may be required for reversal. Fentanyl overdoses also deserve special consideration. Although overdoses of fentanyl are easy to reverse when naloxone is administered, the current potency of street fentanyl is so strong that overdose might simply be too massive or rapid and eliminate the possibility of rescue. Naloxone also could precipitate acute withdrawal and risks associated with acute withdrawal may occur.19
How Is Naloxone Prescribed?
Naloxone is easy to prescribe in all of its formulations. Physicians can even use prepopulated naloxone prescription pads to make it easy to prescribe. Furthermore, many electronic medical records make naloxone prescribing in a similar manner (auto-populated).
Naloxone Nasal Spray
Naloxone HCL 1mg/ml
2x2 ml, as prefilled Luer Lock needleless syringe
Or
2 x intranasal atomizer device
For suspected overdose spray 1 ml in each nostril.
Repeat after 3 minutes if no or minimal response.
Intramuscular Naloxone
Naloxone HCL 0.4 mg/ml
1x 10 ml as 1 flip-top vial
2 x 1 ml single dose vial
Intramuscular IM syringe, 23 G, 3 cc, 1 inch
For suspected overdose inject 1 ml in IM in shoulder or thigh
Repeat after 3 minutes if no or minimal response
Naloxone can be prescribed via three different methods: patient-specific prescriptions, third-party prescriptions, and non-patient-specific prescriptions.20
- Patient-specific prescriptions:
- All 50 states allow medical professionals to prescribe naloxone directly to patients who are at risk. Pharmacists allowed to dispense [updated infographic 2015].
- Third-party prescriptions:
- Some state laws allow for prescription to be provided to someone other than the actual person at risk such as a family member or friend.
- Non-patient-specific prescriptions:
- Standing order: Some states permit prescription of naloxone by order of the state’s top health professional.
- This allows pharmacists to dispense to patients based on that order (i.e., patients do not need to bring in an actual prescription).
- This also enables community organizations/members to dispense in place of a pharmacist.
The naloxone access laws as described above, differ from state to state, but make it easier to obtain naloxone as they eliminate the need to go to a prescriber or pharmacist. Good Samaritan laws also exist. These laws offer protections that may increase the likelihood of obtaining help and/or using naloxone.21 For example, the Good Samaritan possession laws offer protection from arrest for possession of any controlled substance that is found on a user or one calling for help.22
A great resource to learn each state’s naloxone laws is the Naloxone Overdose Prevention Laws Database.23
Medicare and Medicaid, as well as most private health insurers, cover naloxone; however coverage may vary between states. One can bill for naloxone if proper drug abuse screening is performed, in addition to educating the patient on signs and symptoms of naloxone overdose.
Furthermore, the patient must be educated on the proper use of naloxone administration and referred for treatment if deemed necessary. Cost and ease of use should be considered when deciding which form of naloxone to prescribe. Costs can vary from around $20 for injectable naloxone, $40 for injectable nasal spray, $150 for Adapt nasal spray device, and over $4,000 for the Evzio autoinjector.24,25 The Adapt nasal spray device and Evzio autoinjector are the easiest to use with no real assembly required; however they are more expensive than other options. Some state health departments may offer free naloxone via their state’s standing order. For instance, the Virginia Department of Health offers free naloxone either by appointment or by walk-in.
Conclusion
As naloxone has become easier to prescribe and for patients or caregivers to obtain, it is vital for physicians to educate patients about its potential life-saving qualities. In the midst of the opioid epidemic, naloxone may provide valuable life-saving opportunities for those suffering from opioid misuse disorder. Furthermore, it also may protect those at risk from unintended overdose secondary to comorbidities. Barriers to these difficult conversations need to be broken down to continue to increase access to this life-saving medication.
Lynn Kohan, MD, MS, is an associate professor of Anesthesiology and Pain Medicine and the Pain Fellowship director at the University of Virginia Health System in Charlottesville.

References
- Warner M, Chen LH, Makuc DM, Anderson RN, Minino AM. Drug poisoning deaths in the United States 1980-2008. National Center for Health Statistics. 2011;(81):1-8. Updated with Jones, C.M. Prescription Drug Abuse and Overdose in United States. Presented at: Third Party Payer and PDMP Meeting. 2012
- Hedegaard H, Miniño AM, Warner M. Drug Overdose Deaths in the United States, 1999–2017. Centers for Disease Control and Prevention: National Center for Health Statistics. Retrieved from https://www.cdc.gov/nchs/data/databriefs/db329-h.pdf. Accessed on December 10, 2020.
- Vivolo-Kantor, AM, Seth, P, Gladden, RM, et al. Vital Signs: Trends in Emergency Department Visits for Suspected Opioid Overdoses--United States, July 2016-September 2017. Centers for Disease Control and Prevention.
- Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569-76. doi:10.1097/01.j.pain.0000460357.01998.f1.
- Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths - United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419-1427. doi:10.15585/mmwr.mm675152e1
- Centers for Disease Control and Prevention. Community-Based Opioid Overdose Prevention Programs Providing Naloxone—United States, 2010. Available at: https://www.cdc.gov/mmwr/pdf/wk/mm6106.pdf. Accessed December 12, 2020.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65(1):1-49. doi:10.15585/mmwr.rr6501e1
- Jones CM, Compton W, Vythilingam M, Giroir B. Naloxone co-prescribing to patients receiving prescription opioids in the Medicare Part D program, United States, 2016-2017. JAMA. 2019;322(5):462-4. doi:10.1001/jama.2019.7988
- Guy GP Jr., Haegerich TM, Evans ME, Losby JL, Young R, Jones CM. Vital signs: pharmacy-based naloxone dispensing — United States, 2012–2018. MMWR Morb Mortal Wkly Rep. 2019;68:679–86. DOI: http://dx.doi.org/10.15585/mmwr.mm6831e1external icon.
- Hawk K, Vaca F, D’Onofrio G. Reducing fatal opioid overdose: prevention, treatment and harm reduction strategies. Yale J Bio Med. 2015;88(3):235-45.
- Yardley, W. Jack Fishman dies at 83; saved many from overdose. New York Times. December 15, 2013. Available at: https://www.nytimes.com/2013/12/15/business/jack-fishman-who-helped-develop-a-drug-to-treat-overdoses-dies-at-83.html. Accessed December 10, 2020.
- Doe-Simkins M, Quinn E, Xuan Z, et al. Overdose rescues by trained and untrained participants and change in opioid use among substance-using participants in overdose education and naloxone distribution programs: a retrospective cohort study. BMC Public Health. 2014;14:297.
- National Harm Reduction Coalition. Website. Available at: http://harmreduction.org/. Accessed December 10, 2020.
- Wakeman SE, Bowman SE, McKenzie M, Jeronimo A, Rich JD. Preventing death among the recently incarcerated: an argument for naloxone prescription before release. J Addict Dis. 2009;28(2):124-9.
- Lagu T, Anderson BJ, Stein M. Overdoses among friends: Drug users are willing to administer naloxone to others. J Subst Abuse Treat. 2006;30(2):129-33.
- Prescribe to Prevent. Website. Available at https://prescribetoprevent.org/. Accessed December 10, 2020.
- Lloyd J. The clinical use of naloxone. U.S. Food and Drug Administration. Available at: https://www.fda.gov/files/drugs/published/Presentation--The-Clinical-Use-of-Naloxone.pdf. Accessed December 10, 2020.
- Naloxone: Drug Information. UptoDate. Available at: Naloxone: Drug information - UpToDate. Retrieved December 10, 2020.
- Drugs.com. Naloxone side effects. Available at: https://www.drugs.com/sfx/naloxone-side-effects.html. Accessed December 10, 2020.
- The White House President Barack Obama. Updated Infographic: Overdose Prevention, State by State. Available at: http://www.whitehouse.gov/blog/2014/12/17/updated-infographic-overdose-prevention-state-state. Accessed December 10, 2020.
- Burris S, Norland J, Edlin BR. Legal aspects of providing naloxone to heroin users in the United States. Int J Drug Policy. 2001;12(3):237–48.
- National Conference of State Legislatures. Drug Overdose Immunity and Good Samaritan Laws. Available at: http://www.ncsl.org/research/civil-and-criminal-justice/drug-overdose-immunity-good-samaritan-laws.aspx. Accessed December 10, 2020.
- Prescription Drug Abuse Policy System. Naloxone overdose prevention laws. Available at: http://pdaps.org/datasets/laws-regulating-administration-of-naloxone-1501695139. Accessed December 10, 2020.
- Gupta R, Shah ND, Ross JS. The rising price of naloxone-risks to efforts to stem overdose deaths. NEJM. 2016;375(23): 2213-5.
- Centers for Disease Control and Prevention. CDC grand rounds: prescription drug overdoses - a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61(1):10–3.


Leave a commentOrder by
Newest on top Oldest on top