How I Do It: Genicular Nerve Radiofrequency Ablation
Cite as: Greco G, Torres J, Kohan L. How I do it: genicular nerve RFA. ASRA Pain Medicine News 2022;47. https://doi.org/10.52211/asra020122.006.
Genicular nerve radiofrequency ablation (GNRFA) is one of the most widely used procedures for patients with osteoarthritis that is refractory to conservative management; it is an effective treatment option for patients with moderate to severe knee osteoarthritis who want to delay or are not eligible for surgery. GNRFA can be performed using several techniques, including conventional, cooled, or pulsed radiofrequency ablation. As our knowledge of the anterior knee anatomy has advanced, so has our use of GNRFA through novel technical approaches and improved nerve targets.
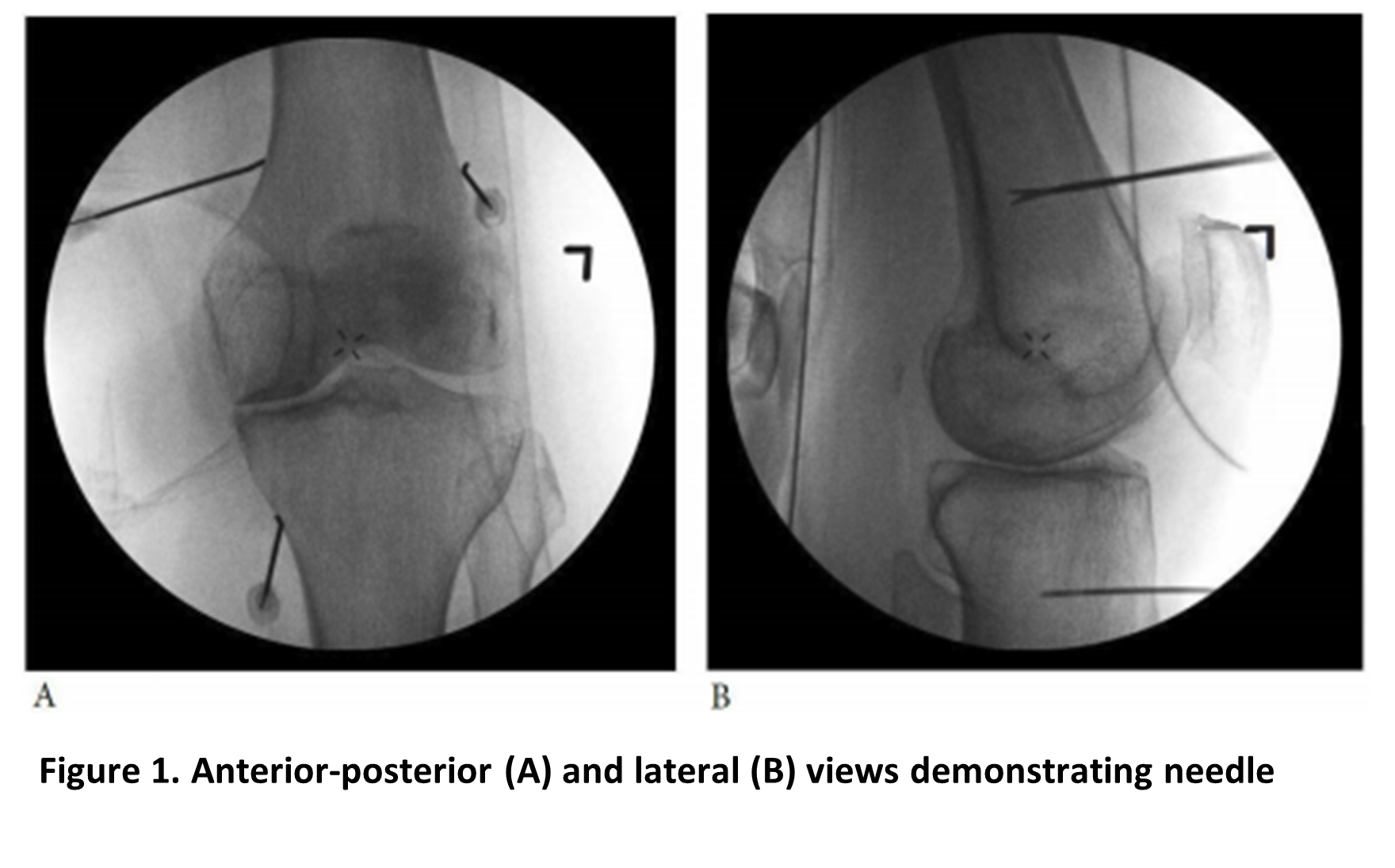
The classic approach described by Choi et al. identifies the knee’s optimal nerve targets as the superior medial genicular nerve (SMGN), superior lateral genicular nerve (SLGN), and inferior medial genicular nerve (IMGN).1 Needle placement for the SMGN and SLGN is at the junction between the distal femoral shaft and medial and lateral femoral epicondyles, respectively; placement for the IMGN is at the junction between the proximal tibial shaft and medial tibial epicondyle (see Figure 1). However, more recent studies indicate that the innervation of the knee joint goes far beyond those three nerves. Today we understand that a total of 14 nerves innervate the knee joint, 10 of which solely innervate the anterior knee,2 and the literature suggests that using additional denervation targets improves outcomes.3
Reprinted with permission from McCormick ZL, Cohen SP, Walega DR, Kohan L. Technical considerations for genicular nerve radiofrequency ablation: optimizing outcomes. Reg Anesth Pain Med. 2021;46(6):518–523. https://doi.org/10.1136/rapm-2020-102117
Pertinent Anatomy
The knee joint’s innervation is divided into four quadrants: superior medial, superior lateral, inferior medial, and inferior lateral. Ideally, the nerve targets in each quadrant are accessed with one skin entry point to minimize patient trauma and discomfort. The superior lateral quadrant encompasses the SLGN, nerve to vastus lateralis, and lateral branch of the nerve to vastus intermedius; the superior medial quadrant encompasses the SMGN, nerve to vastus medialis, and medial branch of the nerve to vastus intermedius; the inferior medial quadrant encompasses the IMGN and infrapatellar branch of the saphenous nerve; and the inferior lateral quadrant encompasses the ILGN and recurrent fibular nerve. The innervation of the anterior knee joint is summarized in Table 1.
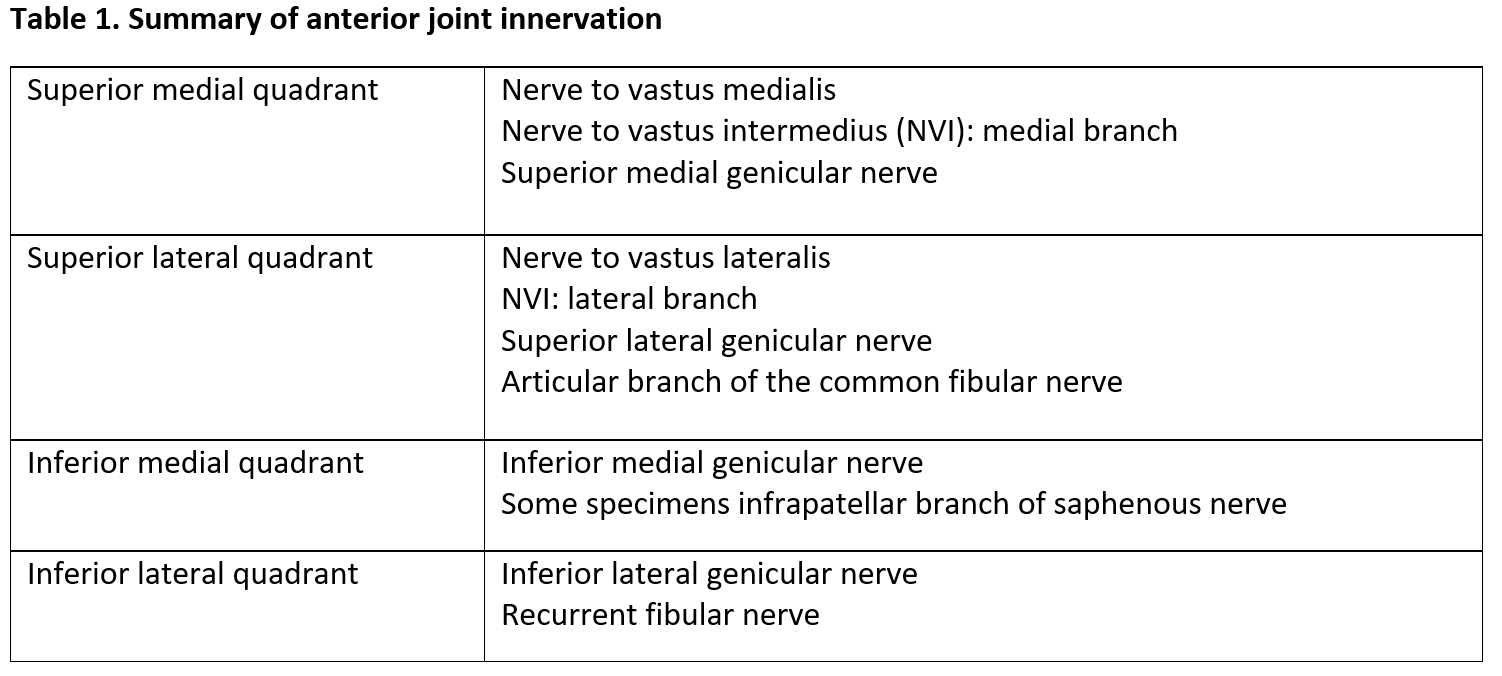
Reprinted with permission from McCormick ZL, Cohen SP, Walega DR, Kohan L. Technical considerations for genicular nerve radiofrequency ablation: optimizing outcomes. Reg Anesth Pain Med. 2021;46(6):518–523. https://doi.org/10.1136/rapm-2020-102117
Description of Technique
Position the patient supine with the target knee flexed at 25–30 degrees using a bolster. Prep and drape the knee in usual sterile procedure, and visualize the joint in anterior-posterior (AP) view. Typically, tilting the C-arm cephalad enables better visualization of the femoral condyles for the SMGN and SLGN and is generally used when entering the skin for the IMGN.
Superior lateral quadrant: To capture the SLGN, nerve to vastus lateralis, and lateral branch of nerve to vastus intermedius, Fonkoue et al recommend targeting the area where the posterior femoral shaft meets the superior edge of the lateral femoral condyle.4 The initial step involves using an AP window and advancing the radiofrequency cannula to the confluence of the lateral shaft of the femur and the epicondyle. Place the first lesion in this location approximately 2 mm from the periosteum. For the second lesion, withdraw the electrode until the tip is halfway across the femoral shaft and 2 mm superficial to the periosteum. The two lesions will denervate the SLGN (labeled C in Figures 2A and 2B).
To target the nerve to vastus lateralis, using the same entry point withdraw the needle and advance 5 cm cephalad to the superior aspect of the patella and 5 mm toward the midline from the lateral border of the femoral shaft until it lightly contacts periosteum. Lastly, to capture the nerve to vastus intermedius, withdraw the cannula about 1 cm until the tip is at the same depth as the quadriceps tendon (labeled A and B1 in Figures 2A and 2B).
Superior medial quadrant: For the first lesion, use an AP view and advance the cannula to the confluence of the medial femoral shaft and medial epicondyle (labeled D1 and D2 in Figure 2A). Then use a lateral view to advance the cannula posteriorly approximately nine-tenths of the way across the femoral shaft. According to Funkoue et al, approximately 2–3 mm anterior to the adductor tubercle is the best target to capture the SMGN.4 For the second lesion, withdraw the cannula until it is one-third of the way across the femoral shaft and 1 cm superficial to the periosteum to capture the vastus medialis.
To capture the nerve to vastus intermedius medial branch, use the same skin entry point but withdraw the cannula to subcutaneous tissue and then advance it 5 cm cephalad to the superior aspect of the patella. Aim for 5 mm toward the femoral shaft’s medial border, avoiding the quadriceps tendon, until it contacts periosteum. Confirm the position with a lateral view, and create the lesion 2 mm above periosteum (labeled B2 in Figures 2A and 2C).
Inferior medial quadrant: The first lesion targets the IMGN. Use AP view and direct the cannula toward the confluence of the medial tibial shaft and tibial flare with a slight cephalad projection (labeled H in Figure 2A). Confirm placement using lateral view, advance the cannula three-quarters of the distance across the tibial shaft, then create the lesion 4 mm superficial to the periosteum. The second lesion targets the infrapatellar branch of the saphenous nerve. With the same canula, withdrawal the tip and redirect it 4 cm medial to the apex of the patella and the tibial tuberosity, at the transverse level of the tibial tuberosity. Create the lesion here, 2 mm above the periosteum, using ultrasound or sensory stimulation if necessary (labeled F in Figure 2A).
Inferior lateral quadrant: Because of its proximity to the common peroneal nerve, the knee’s inferior lateral quadrant may be challenging to target, but Fonkoue et al outlined a prudent approach to avoid damage to important nearby structures.4 To target the recurrent fibular nerve, use the AP view and advance the cannula to the lateral tibial flare at the craniocaudal level of the lower third of the fibular head (labeled G in Figure 2A). With a lateral view, confirm that the cannula tip is 2 mm anterior to the fibular head (two-thirds of the way across the tibia), then create the lesion 2 mm superficial to periosteum (labeled G in Figure 2B). To target the inferior lateral genicular nerve, use an AP view to advance the cannula to the lower end of the femoral condyle, just below the upper border of the tibial condyle (labeled E in Figure 2A). Using a lateral view, reposition the cannula approximately two-thirds of the depth of the tibia (labeled E in Figure 2B). Next, perform motor testing on the patient to ensure that the cannula is a safe distance away from the common peroneal nerve, and created the lesion 2 mm above the periosteum.
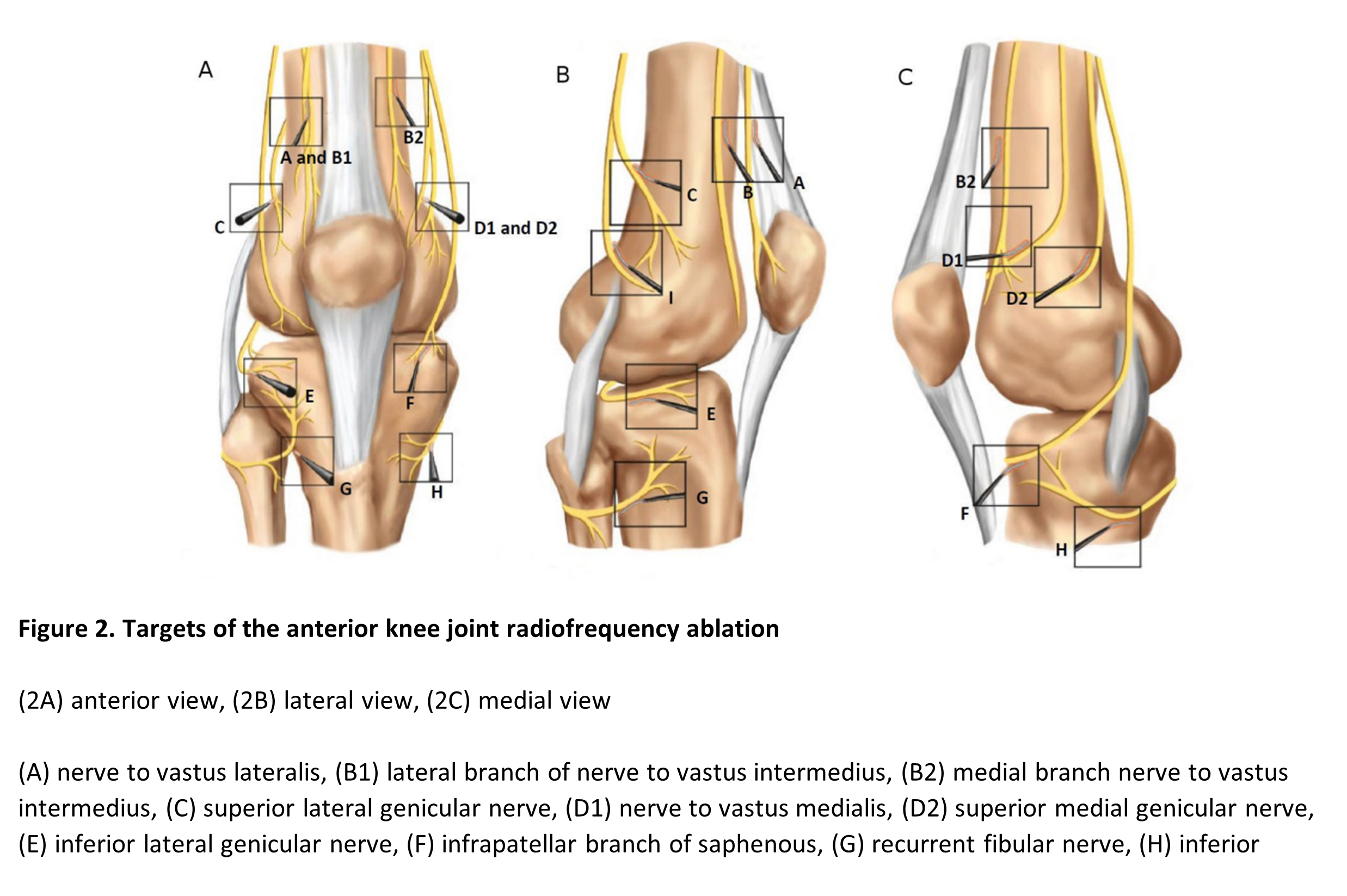
Reprinted with permission from McCormick ZL, Cohen SP, Walega DR, Kohan L. Technical considerations for genicular nerve radiofrequency ablation: optimizing outcomes. Reg Anesth Pain Med. 2021;46(6):518–523. https://doi.org/10.1136/rapm-2020-102117
Conclusion
Executing radiofrequency ablation of the knee joint requires a thorough understanding of knee anatomy to reliably achieve pain relief in patients experiencing osteoarthritis. Since its development, GNFRA has undergone changes that incorporate the latest research findings. More studies are needed to compare the effectiveness of the traditional three-nerve approach (ie, SMGN, SLGN, and IMGN) with a more comprehensive approach such as described in this article. Nonetheless, radiofrequency ablation remains a viable option for patients with moderate to severe osteoarthritis to reduce pain symptoms and opioid use and improve overall quality of life.
Acknowledgements: The authors would like to thank would like to thank Drs. Zachary L. McCormick, Steven P. Cohen, and David R. Walega as authors of the article, “Technical Considerations for Genicular Nerve Radiofrequency Ablation: Optimizing Outcomes,” published in the June 2021 issue of Regional Anesthesia and Pain Medicine (https://doi.org/10.1136/rapm-2020-102117).

Guy Greco, MD, is a resident physician in neurology at George Washington University in Washington, District of Columbia.

Joseph Torres, MD, is a fellow physician in pain management at the University of Virginia in Charlottesville, Virginia.
Lynn Kohan, MD, is an associate professor of anesthesiology and pain management in the Department of Anesthesiology at the University of Virginia in Charlottesville, Virginia.
References
- Choi W-J, Hwang S-J, Song J-G, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain. 2011;152(3):481–7. https://doi.org/10.1016/j.pain.2010.09.029
- Tran J, Peng PWH, Lam K, et al. Anatomical study of the innervation of anterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2018;43(4):407–14. https://doi.org/10.1097/aap.0000000000000778
- Chen Y, Vu TH, Chinchilli VM, et al. Clinical and technical factors associated with knee radiofrequency ablation outcomes: a multicenter analysis. Reg Anesth Pain Med. 2021;46(4):298–304. https://doi.org/10.1136/rapm-2020-102017
- Fonkoue L, Behets CW, Steyaert A, et al. Accuracy of fluoroscopic-guided genicular nerve blockade: a need for revisiting anatomical landmarks. Reg Anesth Pain Med. 2019;44:950–8. https://doi.org/10.1136/rapm-2019-100451

Leave a commentOrder by
Newest on top Oldest on top