The Beauty of Diversity in Medicine
The year 2020 has changed the fabric of society, compelling us to look within ourselves regarding what we value, what we believe, and how we treat each other. Most of this article was written prior to the deaths of Breonna Taylor, George Floyd, and others at the hands of police violence. Their deaths and the revolution that has followed bring into sharper focus the disparities in health care representation and delivery that exist within our society. This article does not remotely cover the scope of the relationship of race inequality and injustice, but we hope to address why diversity within medicine is so vital.
It is not enough to be impartial; the active promotion of minorities in medicine is of vital importance.
Despite a tumultuous beginning to the year, the 2020-2021 Residency Match season will begin soon. Historically, department leadership focused on grades, scores, and recommendation letters, but do “objective” measurements necessarily equate to the best candidate? As the population in the United States continues to grow and diversify, the medical field faces the task of following suit, providing both access to and representation of the general population. More importantly, those in medicine should actively combat racial inequality for the benefit of all.
The Current State of Under-Represented Minorities in Medicine
Minority underrepresentation is present at all levels of medical training, from medical school to residency, and even beyond into practice and leadership positions. Minority underrepresentation has actually increased since 2002; while the total number of minority medical students has increased since then, it did so at a lower rate than their age-matched counterparts in the population.[1] This in turn translates to decreased representation at a faculty level (Figure 1). Data collected in 2015 by the Association of American Medical Colleges (AAMC) showed that, while there was an increasing percent of female faculty (39%), only 4% of faculty members were both female and identified as a minority[2] (Figure 2).
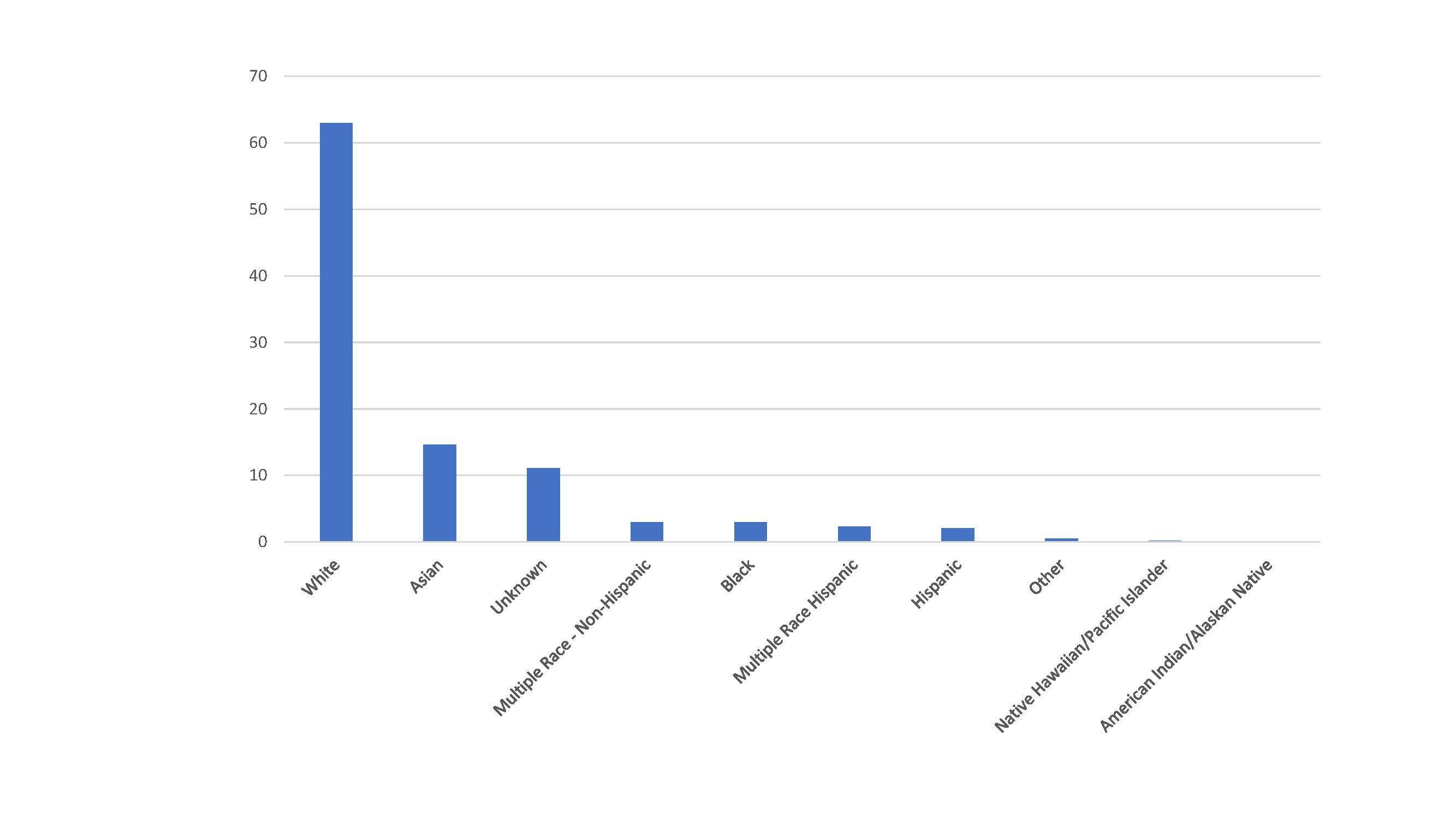
Figure 1: Percentage of full-time U.S. medical school faculty by race and ethnicity.[1]
While minorities are underrepresented in medicine in general, some specialties struggle more to attract minorities and women. Medical specialties show a little more than 25% under-represented minorities (URM), while in surgical subspecialties, URM representation drops to about 20% with the field of urology experiencing the lowest rate of URM representation at 17.7%.[3] The reasons are varied and often multifactorial, but decreased exposure to a specialty in medical school, limited research and shadowing opportunities, and a lack of mentors play a role in preventing both female and URM consideration of a field.[4] Even in the seven medical subspecialties that boasted a female majority in 2012, URM representation lagged far behind the general population with radiology, orthopedic surgery, and otolaryngology struggling the most.[5]
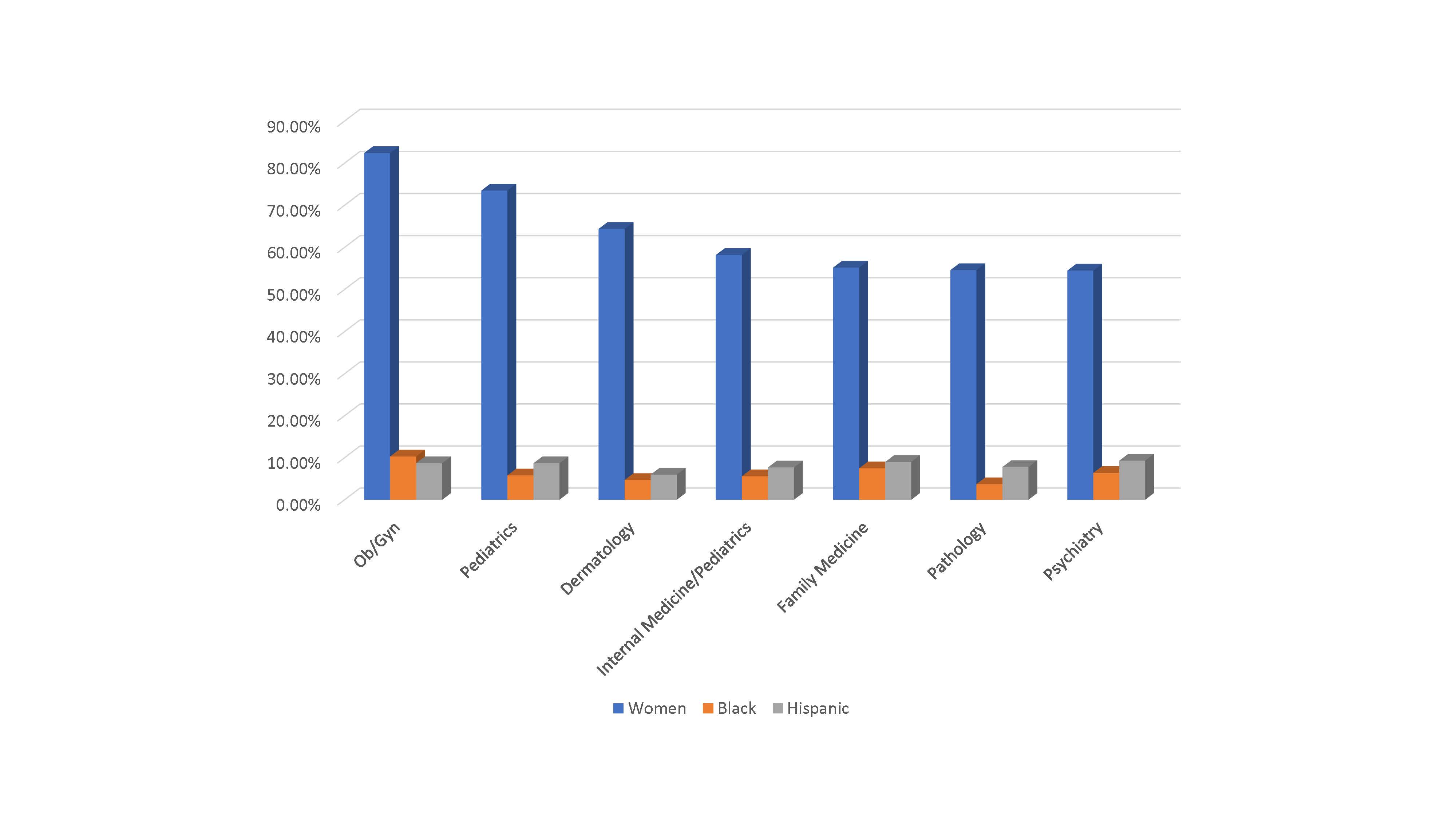
Figure 2: Medical subspecialties with female majority with corresponding underrepresented minority representation.[5]
The field of anesthesiology has seen a surge in female anesthesiologists but still falls short of the female representation in the general medical workforce.[6] Both women and URM lag in leadership positions compared to both representation in the physician workforce and the general population as can be witnessed in the leadership of the American Society of Anesthesiologists (ASA).[7] A major barrier for the field of anesthesiology is the lack of exposure during medical school; anesthesiology is not required as part of the core curriculum and as a “hidden” specialty is not a commonly chosen elective.
Obstacles and Barriers
Appreciating the trials of minority members in the medical field requires understanding of the common barriers that can act as active hindrances or lead to estrangement, decreasing team cohesiveness. A 2018 study queried residents from 21 different programs across the country and found several common elements in their experiences. The top three themes that they discovered included microaggression and bias, being tasked as minority ambassadors, and difficulty defining a professional and personal identity.[8]
Bias
Implicit bias, defined as unconscious attitudes and stereotypes that all members in a population hold and which may or may not affect their behavior to others, becomes problematic in medicine because it affects medical decision making or patient perception of a caregiver.
Although they are not the exception, URMs and women experience both implicit bias and microaggression at a higher rate and face questions and assumptions about training, abilities, traditional roles, background, and cultural differences. This is a pervasive and constant reminder that these groups of people are different and separate. Kaplan et al found that some residents report being constantly mistaken for one of the few other minorities in their program by their own staff which indicates that though they are separate from the majority, they are interchangeable with each other.
Mentorship and Identity
URM were retained at a lower rate in academic institutions compared to white colleagues; they were published and promoted less frequently as well.[9] Lack of mentorship is a potential reason; similar backgrounds are not required to provide career and educational guidance for a URM medical student, resident, or faculty member, but having similar backgrounds can be beneficial in the navigation of common barriers in the professional environment.
URM populations struggle to assimilate into their workplace while maintaining a sense of individual and cultural identity, which can lead to a mismatch between personal and professional identities.
Minority Tasking
In the medical world, minority groups are commonly expected to bear the burden of recruiting their own. In places where diversity is not prevalent, this task falls to a few individuals, adding to their already heavy workloads and potentially limiting opportunities that might lead to promotion. Minority tasking unfairly distributes burden to URM and women what should be shared with many: recruitment, education, curriculum development, and mentorship.
Benefits of Diversity
Financial
Many industries have recognized the lack of minorities in their ranks and the benefits of diversifying their workforce. In the banking industry, growth firms with greater racial diversity were shown to have higher productivity and increased return on equity.[10] Another study looking at gender diversity within service and manufacturing organizations found a positive linear relationship between employee productivity and greater gender diversity, with productivity increasing by $38,824 for every 5-point increase in Blau’s index (an index of group diversity).[11] Medicine is unlike any other industry; while monetary gains can serve as incentive, providing better patient care, access, and representation, as well as improving physician satisfaction, are the real goals for increasing diversity in medicine.
Access and Representation
It has been well documented that health care disparities exist within our country; URM and women can and do positively impact population health. The infant and maternal mortality rate for African-American (AA) and Native-American (NA) women is 2 to 3 times higher than for white women and the highest for a developed nation.[12],[13] HIV infection rates are higher in the AA, Hispanic, and NA populations, and African Americans and Native Americans have much higher rates of diabetes, hypertension, and stroke than their white counterparts.[14],[15]
Coupled with poorer health in minority populations is the finding that minorities are more likely to get lower valued healthcare and less likely to be referred to specialists for time-sensitive surgeries along with diagnostic and therapeutic procedures. African Americans suffer higher rates of amputations with fewer revascularizations than their white counterparts. Provider bias contributes, in part, to this unequal distribution of medical care.[16]
A study found that women account for 50.8% of the U.S. population but only 35.2% of practicing U.S. physicians.[17] The same study documented that URMs and women physicians tend to practice more often in underserved communities and provide care for poorer populations. Minorities patients also were found to receive Medicaid at a higher rate than their white male colleagues even when adjusting for socioeconomic status.[17]
Despite having fewer numbers, female physicians are more likely to care for women and patients with complex psychosocial issues while also providing patients with more preventive care and counseling. Patients of female physicians were more likely to survive a myocardial infarction and had lower hospital readmission rates.[16]
Patients tend to select physicians who resemble them and are more satisfied with care from these physicians.[16] When AA male patients were seen by a racially concordant physician, they were more likely to participate in and adhere to the preventative strategies their physicians prescribed, which could lead to better health.[18] Given that minority communities receive lower quality healthcare more frequently, increasing the population of URM and women physicians to combat the issue of access to care will help to improve the population health of minority patients. This is especially critical given that by 2050, half of the US population will identify as non-white minorities.[19]
Physician Satisfaction
Burnout among physicians has been called a growing public crisis. According to an article published by the Mayo Clinic, nearly 54% of practicing physicians experience symptoms of burnout.[20] In addition, 10.5% of these physicians reported a major medical error within the prior three-month period, and 3.9% had a failing patient safety grade.[20] Not only does the individual physician suffer lower productivity, career dissatisfaction, and suicidal ideation, but patients experience poorer quality of care. Burnout has negative consequences for patients when experienced by resident physicians as well attending physicians. In a study published by JAMA, 55.2% of residents experienced symptoms of burnout and had greater implicit and explicit racial biases.[21]
URM physicians, particularly Hispanic physicians, experience lower stress and higher career satisfaction compared to their white colleagues.[16] Increasing the pool of URM physicians may positively contribute to decreased rates of burnout. Also, increasing the pool of URM residents decreases the risk of depression for URM residents and non-URM residents in the program.[22] By diversifying the physician workforce, we have the potential to provide not just more access to care, but better quality of care for our nation as a whole.
Goals and Plans for Improving Diversity
Promoting diversity is a multifactorial and active process that requires the support of leadership as well as early exposure, encouragement, and mentorship. While increasing female and URM representation within a department, institution, and medicine as a whole may seem like a daunting task, there are success stories. Auseon et al describe improved URM recruiting to the Ohio State University Cardiology Fellowship via prioritization of current URM fellows, forming a subcommittee to focus on URM candidates, reaching out to diverse residency programs, and adjusting the agenda of the interview day to focus on mentorship, among other methods.[23] The study did highlight the importance of both URM faculty and guest speakers to exemplify commitment to URM support and promotion.
Although not a medical specialty, the methods and results from Carmichael et al’s study to increase URM undergraduate student success in science, technology, engineering, and math (STEM) courses could apply to advancing URM and women in medicine.[24] The study focused on understanding the needs of students and used a multi-tiered approach to teaching including use of a resource center, advising, academic success office, and peer tutoring. The investigators worked to identify barriers and obstacles for high-risk students, including isolation and uncertainty, inadequate time management and study skills, and needing to work while in school to provide more well-rounded support to their students. It emphasized data driven, systematic interventions to encourage more active participation by faculty and support staff to increase the success of students.
Combating Myths and Affecting Strategy
Improving strategy for both recruitment and retention of URM and women in medicine requires first the changing of the existing mindset toward diversity in the field. Diversity is often seen in opposition to meritocracy, and it is believed that the real problem lies in the pipeline itself, limiting both female and URM candidates because of low numbers in the first place, as well as family planning and lifestyle priorities.[25] Medical schools currently boast higher numbers of women than men, and the most commonly cited reason for avoiding certain specialties is lack of mentorship and representation. Both women and URM are bypassed secondary to bias rather than lack of merit for positions.
Strategies to improve URM and women recruitment and retention include changing the culture of the organization, training leaders, and using targeted recruitment strategies focusing on both URM and women.
Leadership
Leadership support is paramount to the success of both the recruitment and retention of women and URM within a department. Both populations face challenges that their male and non-URM colleagues do not; implicit and explicit bias, family planning, lack of mentorship, and cultural differences, as well the burden of representation, can quickly lead to burnout. “Program leadership should note that workplace bias is likely underrecognized by institutions” (p. 8).[8] This is the first step to providing an environment that ensures the success of URM and women within a department.
Early Support for URM/Women
Recruitment is not enough, institutions benefit from focusing on efforts surrounding retention. Early support of employees is crucial to establish prioritization of diversity; new employee orientations should include education and support of diversity and provide a socialization process to reduce bias. “Multicultural organizations need new employee diversity orientation programs that create a two-way socialization process ensuring that (1) bias is reduced and (2) minority perspectives influence organizational norms and values” (p.173).[10]
Continued support for URM and women in medicine is required; the path to promotion is paved by opportunities to research and network. “Regional and national initiatives to promote networking, education and professional development may connect URM and female students, residents and practicing [faculty], thereby fostering mentorship opportunities and supportive communities” (p. 5).[4] In doing this, institutions provide an avenue and the laid groundwork for residents and faculty to succeed with the help of those who have shared their path.
Conclusion
While the current state of diversity in medicine is disheartening, more institutions and departments realize the benefits of diversifying the physician workforce. It is not enough to be impartial; the active promotion of minorities in medicine is of vital importance. The first steps include accepting that lack of diversity is problematic and changing the culture and bias within a department. Though it is difficult to avoid implicit bias given its pervasiveness, active vigilance, self-assessment, and de-biasing activities can limit the role of implicit bias in medicine. Increasing the presence of women and URM within medicine will take active participation, early and continued support, and vigilance for bias. Though the road ahead is long, the potential rewards of a more equitable workforce are great and include improved physician satisfaction, improved patient care, greater representation of the national population, and a step toward equality in our society.
References
- Lett LA, Murdock HM, Orji WU, Aysola J, Sebro R. Trends in racial/ethnic representation among US medical students. JAMA Netw Open. 2019; 2(9):e1910490. https://doi.org/10.1001/jamanetworkopen.2019.10490
- Association of American Medical Colleges. Current trends in medical education. https://www.aamcdiversityfactsandfigures2016.org/report-section/section-3/. Published 2016. Accessed July 7, 2020.
- Shantharam G, Tran TY, McGree H, Thavaseelan S. Examining the trends in underrepresented minorities in urology residency. Urology. 2019;127:36-41. https://doi.org/10.1016/j.urology.2018.10.061
- Dai JC, Agochukwu-Mmonu N, Hittelman AB. Strategies for attracting women and underrepresented minorities in urology. Curr Urol Rep. 2019;20(10):61. https://doi.org/10.1007/s11934-019-0921-5
- Deville C, Hwang W-T, Burgos R, Chapman CH, Both S, Thomas CR. Diversity in graduate medical education in the united states by race, ethnicity, and sex, 2012. JAMA Intern Med. 2015;175(10):1706-8. https://doi.org/10.1001/jamainternmed.2015.4324.
- Kenevan MR, Gali B. History, current state, and future of diversity in the anesthesia workforce. Adv Anesth. 2019;37:53-63. https://doi.org/10.1016/j.aan.2019.08.001
- Toledo P, Duce L, Adams J, Ross VH, Thompson KM, Wong CA. Diversity in the American Society of Anesthesiologists leadership. Anesth Analg. 2017;124(5):1611–6. https://doi.org/10.1213/ane.0000000000001837
- Osseo-Asare A, Balasuriya L, Huot SJ, et al. Minority resident physicians’ views on the role of race/ethnicity in their training experiences in the workplace. JAMA Netw Open. 2018;1(5)e182723. https://doi.org/10.1001/jamanetworkopen.2018.2723
- Kaplan SE, Raj A, Carr P, et al. Race/ethnicity and success in academic medicine: findings from a longitudinal multi-institutional study. Acad Med. 2018;93(4):616–22. https://doi.org/10.1097/ACM.0000000000001968
- Richard OC. Racial diversity, business strategy, and firm performance: a resource-based view. Acad Manage J. 2000;43(2):164-77.
- Ali M, Kulik C, Metz I. The gender diversity-performance relationship in services and manufacturing organizations. Int J Hum Resour Manag. 2011;22(7):1464-85. https://doi.org/10.1080/09585192.2011.561961
- Centers for Disease Control and Prevention. Racial and ethnic disparities continue in pregnancy-related deaths. https://www.cdc.gov/media/releases/2019/p0905-racial-ethnic-disparities-pregnancy-deaths.html. Published September 5, 2019. Accessed July 8, 2020.
- Centers for Disease Control and Prevention. Infant mortality. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.htm. Accessed July 9, 2020.
- U.S. Department of Health and Human Services Office of Minority Health. Stroke and American Indians/Alaska Natives. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=43. Accessed July 9, 2020.
- U.S. Department of Health and Human Services Office of Minority Health. Stroke and African Americans. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=28. Accessed July 9, 2020.
- Geiger HJ. Racial and ethnic disparities in diagnosis and treatment: A review of the evidence and a consideration of causes. In: Smedley BD, Stith AY, Nelson AR (eds). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2006;417-44.
- Silver JK, Bean AC, Slocum C, et al. Physician workforce disparities and patient care: a narrative review. Health Equity. 2019;3(1)360-77. https://doi.org/10.1089/heq.2019.0040
- Alsan M, Garrick O, Graziani G. Does diversity matter for health? Experimental evidence from Oakland. National Bureau of Economic Research. https://www.nber.org/papers/w24787. Published June 2018. Accessed July 9, 2020.
- Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff (Millwood). 2002;21(5)90-102. https://doi.org/10.1377/hlthaff.21.5.90
- Tawfik DS, Profit J, Morgenthaler T, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93(11):1571-80. https://doi.org/10.1016/j.mayocp.2018.05.014
- Dyrbye L, Herrin J, West CP, et al. Association of racial bias with burnout among resident physicians. JAMA Netw Open. 2019;2(7):e197457. https://doi.org/10.1001/jamanetworkopen.2019.7457
- Elharake JA, Frank E, Kalmbach DA, Mata DA, Sen S. Racial and ethnic diversity and depression in residency programs: a prospective cohort study. J Gen Intern Med. 2020;35(4):1325-7. https://doi.org/10.1007/s11606-019-05570-x
- Auseon AJ, Kolibash AJ Jr, Capers Q. Successful efforts to increase diversity in a cardiology fellowship training program. J Grad Med Educ. 2013;5(3):481–5. https://doi.org/10.4300/JGME-D-12-00307.1
- Carmichael MC, St Clair C, Edwards AM, et al. Increasing URM undergraduate student success through assessment-driven interventions: a multiyear study using freshman-level general biology as a model system. CBE Life Sci Educ. 2016;15(3): ar38. https://doi.org/10.1187/cbe.16-01-0078
- Backhus LM, Kpodonu J, Romano JC, Pelletier GJ, Preventza O, Cooke DT. An exploration of myths, barriers, and strategies for improving diversity among STS members. Annals Thoracic Surgery. 2019;108(6):1617-24. https://doi.org/10.1016/j.athoracsur.2019.09.007
Leave a commentOrder by
Newest on top Oldest on top