How We Do It: Enhanced Recovery Pathway for Geriatric Hip Fracture
Cite as: Machi A., Sorich M., Street A. How we do it: enhanced recovery pathway for geriatric hip fracture. ASRA News. 2021;46. https://doi.org/10.52211/asra050121.035.
Enhanced recovery after surgery (ERAS) pathways or enhanced recovery pathways (ERPs) are cohesive, evidence-based, multidisciplinary protocols used to guide the perioperative management of surgical patients.1 Although this innovative process started in the colorectal surgery realm, it has quickly progressed to other surgical fields, including a robust effort within the orthopedic surgery arena.2-5 While these protocols are applicable and beneficial to patients of all ages, we know that geriatric patients often need unique strategies to optimize their care. The recent introduction of the Perioperative Optimization of Senior Health (POSH) initiatives has aimed to design care plans specifically for elderly hospital patients.6 We established the first ERP at our institution in 2016 and currently have 12 successful pathways for different types of surgery.7 As we embarked on establishing an ERP for geriatric patients with hip fractures, we sought to combine our experience with ERPs and the specialized medical care found in the POSH initiatives. The essential feature of developing this pathway was forming a comprehensive multidisciplinary team of physicians, nurses, pharmacists, advanced practice providers, therapists, and other experts to develop management strategies guided by the best available evidence for this specific geriatric orthopedic patient population from a broad array of perspectives.
This collaborative effort to optimize acute perioperative care while aggressively addressing secondary prevention measures will lead to improved overall health for our geriatric patients for years to come.
Two aspects of geriatric hip fractures make it challenging to follow other common pathways. First is the timing of presentation. Typically, a patient presents with a hip fracture acutely. In an effort to decrease morbidity and mortality and improve functional recovery, it is optimal that the surgery occurs within 24-48 hours of the fracture.8,9 Lack of time prior to surgery is often the main difficulty in applying the common ERP principles such as full optimization of medical conditions and nutrition, encouraging the consumption of clear fluids or carbohydrate drinks, fully educating patients and their families, and setting comprehensive postoperative expectations. Furthermore, the vast majority of patients presenting with these fractures are 65 years or older. This population is associated with high-risk comorbidities and physiological changes related to aging, which necessitate specific recommendations for the perioperative and postoperative periods to improve overall outcomes. Efforts to reduce polypharmacy and delirium are essential, while striving to increase mobility, mitigate the impact of comorbidities such as anemia and malnutrition, as well as acquire appropriate disposition and timely follow up postoperatively are all crucial elements.
Our initial collaborative effort was led by our lead orthopedic surgeon, Megan Sorich, DO, and a group of dedicated anesthesiology faculty (including Anthony Machi, MD, and Austin Street, MD, FASA). We used the national recommendations of the ERAS® Society for hip replacement surgery as a starting point and incorporated applicable evidence-based and expert recommended interventions.5,8,10-13 We then worked with our geriatric medicine team and identified key goals for perioperative management of elderly patients: avoiding polypharmacy and certain high-risk medications, daily delirium screenings, and postoperative management in conjunction with our surgical team.14 As appropriate and timely analgesia is extremely important in management of these patients, we also collaborated with our emergency medicine physician colleagues. For the first time at our institution, the Acute Pain Service (staffed by anesthesiology) and emergency medicine physicians shared the responsibility of placing fascia iliaca blocks within 8 hours of admission to both improve pain control and decrease opioid needs in these patients.15
This pathway was also designed to work in harmony with our geriatric hip fracture co-management program. The primary champions of this program include emergency medicine, orthopedic surgery, anesthesiology, geriatric medicine, nutrition, physical therapy, internal medicine, physical medicine and rehab, and bone mineral metabolism. The goals of this program are broader than those of the ERP, encompassing the acute, immediate intraoperative, and postoperative outcomes, as well as secondary prevention. Therefore, this pathway was designed to not only reduce hip fracture morbidity and mortality and decrease hospital length of stay but also to prevent the next osteoporosis fracture from occurring and improve longer-term outcomes. This alignment permitted an integration of features in our electronic medical record and for care to be optimized and coordinated across consulting teams while facilitating discharge planning. The additional benefits of the electronic medical record include the creation of a database and patient registry for future audits and research purposes.
After months of lengthy discussion and meetings with various teams of specialists as well as hours of literature review, a protocol emerged that required dedication and collaboration between multiple teams. Key features of the protocol are included in Appendix 1.
Early Diagnosis
The pathway is automatically initiated when a fracture is diagnosed radiographically in the emergency department (ED) and consultation is placed to the orthopedic surgeon. When the orthopedic surgeon determines the patient is operable, the ERP launches and a cascade of events are initiated.
Preoperative
Analgesia begins in the ED and includes an ultrasound-guided single injection fascia iliaca block by either an emergency medicine physician or an anesthesiologist from the Acute Pain Service. The patient is admitted to a General Internal Medicine Service, and a pathway specific order set is used to ensure appropriate optimization for surgery including ordering of any laboratory tests or electrocardiogram, NPO guidelines, delirium prophylaxis, anticoagulation management, and multimodal opioid-sparing analgesia. Additionally, the patient and patient caregivers are invited to be proactive in the patient’s recovery and encouraged to define their own goals for recovery and review educational material that is provided on physical and digital platforms.
Intraoperative
When possible, a neuraxial anesthetic is administered to provide intraoperative anesthesia. In all cases, key elements include antibiotic prophylaxis, thromboembolic prophylaxis, standard ASA monitors, minimization of invasive monitors except when a patient meets predefined criteria, perioperative nausea and vomiting prophylaxis, fluid management goals to maintain euvolemia and normotension, and blood loss prevention including tranexamic acid when possible. Finally, multimodal analgesia is used with acetaminophen, celecoxib, and minimal administration of intravenous fentanyl. Long-acting opioids, gabapentinoids, muscle relaxants, and alpha-2 agonists are avoided. If greater than 18 hours has elapsed since the initial fascia iliaca block, a repeat single injection block is performed immediately prior to the induction of anesthesia or administration of neuraxial anesthetic.
Postoperative
During the postoperative period, early ambulation and return to activities of daily living are facilitated by the physical and occupational therapy teams, while discharge planning is strategized by social work and home health consultants. Comorbid conditions are addressed with special attention to anemia, malnutrition, and bone health. In patients at elevated risk for the development of perioperative cognitive dysfunction (age > 80 years, polypharmacy, preexisting dementia, or multiple comorbidities with high risk for delirium) additional assistance is targeted through early consultations with physical medicine and rehabilitation or geriatric medicine via general internal medicine coordination.
Our aims of ERP for geriatric hip fracture are ambitious. They combine not only the typical ERP goals but also those specific to the geriatric population.
We believe this collaborative effort to optimize acute perioperative care while aggressively addressing secondary prevention measures will lead to improved overall health for our geriatric patients for years to come.
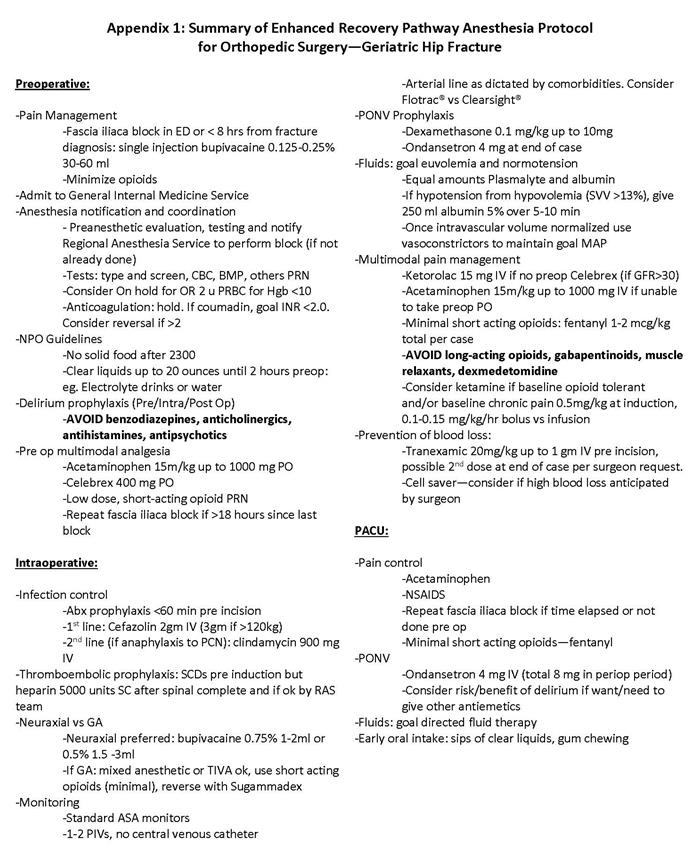
Appendix 1: Summary of Enhanced Recovery Pathway Anesthesia Protocol for Orthopedic Surgery - Geriatric Hip Fracture. Download as a pdf

Anthony Machi, MD, is an assistant professor in the department of anesthesiology and pain management and the fellowship director for regional anesthesia and acute pain medicine at the University of Texas Southwestern Medical Center in Dallas.

Megan Sorich, DO, is an assistant professor in the department of orthopedic surgery at the University of Texas Southwestern Medical Center in Dallas.

Austin Street, MD, FASA, is the medical director of Enhanced Recovery After Surgery and an assistant professor in the department of anesthesiology and pain management at the University of Texas Southwestern Medical Center in Dallas.
References
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606-617. https://doi.org/10.1093/bja/78.5.606.
- Wainwright T, Middleton R. An orthopaedic enhanced recovery pathway. Curr Anaesth Crit Care. 2010;21(3):114-120. https://doi.org/10.1016/j.cacc.2010.01.003.
- Wainwright TW, Immins T, Middleton RG. Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best Pract Res Clin Anaesthesiol. 2016;30(1):91-102. https://doi.org/10.1016/j.bpa.2015.11.001.
- Garriga C, Murphy J, Leal J, et al. Assessment on patient outcomes of primary hip replacement: an interrupted time series analysis from 'The National Joint Registry of England and Wales'. BMJ Open. 2019;9(11):e031599. https://doi.org/10.1136/bmjopen-2019-031599.
- Wainwright TW, Gill M, McDonald DA, et al. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. Acta Orthop. 2020;91(1):3-19. https://doi.org/10.1080/17453674.2019.1683790.
- McDonald SR, Heflin MT, Whitson HE, et al. Association of integrated care coordination with postsurgical outcomes in high-risk older adults: The Perioperative Optimization of Senior Health (POSH) Initiative. JAMA Surg. 2018;153(5):454-462. https://doi.org/10.1001/jamasurg.2017.5513.
- Street AD, Elia JM, McBroom MM, et al. The impact of implementation of a hysterectomy enhanced recovery pathway on anesthetic medication costs. J Comp Eff Res. 2020;9(15):1067-1077. https://doi.org/10.2217/cer-2020-0142.
- Boddaert J, Raux M, Khiami F, Riou B: Perioperative management of elderly patients with hip fracture. Anesthesiology. 2014;121:1336-1341. https://doi.org/10.1097/ALN.0000000000000478.
- Maheshwari K, Planchard J, You J, et al. Early surgery confers 1-year mortality benefit in hip-fracture patients. J Orthop Trauma. 2018;32(3):105-110. https://doi.org/10.1097/BOT.0000000000001043.
- Morrison RS, Dickman E, Hwang U, et al. Regional nerve blocks improve pain and functional outcomes in hip fracture: a randomized controlled trial. J Am Geriatr Soc. 2016;64:2433-2439. https://doi.org/10.1111/jgs.14386.
- Basu N, Natour M, Mounasamy V, Kates SL: Geriatric hip fracture management: keys to providing a successful program. Eur J Trauma Emerg Surg. 2016;42:565-569. https://doi.org/10.1007/s00068-016-0685-2.
- Chuan A, Zhao L, Tillekeratne N, et al. The effect of a multidisciplinary care bundle on the incidence of delirium after hip fracture surgery: a quality improvement study. Anaesthesia. 2020;75(1):63-71. https://doi.org/10.1111/anae.14840.
- Hecht G, Slee CA, Goodell PB, et al. Predictive modeling for geriatric hip fracture patients: early surgery and delirium have the largest influence on length of stay. J Am Acad Orthop Surg 2019, 27(6):e293-e300. https://doi.org/10.1111/anae.15202.
- Friedman SM, Mendelson DA, Kates SL, et al. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56(7):1349-1356. https://doi.org/10.1111/j.1532-5415.2008.01770.x.
- Garlich JM, Pujari A, Debbi EM, et al. Time to block: early regional anesthesia improves pain control in geriatric hip fractures. J Bone Joint Surg Am. 2020;102(10):866-872. https://doi.org/10.2106/JBJS.19.01148.
Leave a commentOrder by
Newest on top Oldest on top