POCUS Spotlight: The Future Is Getting Smaller – Handheld Ultrasound Technology
Cite as: Wilkinson JN, Lim N. The future is getting smaller – handheld ultrasound technology. ASRA News 2021;46. https://doi.org/10.52211/asra080121.048.
The invention of the stethoscope by the French physician René Laennec in 1816 ushered in the era of handheld diagnostics available to the clinician at the patient’s bedside. The evolution of the stethoscope over 150 years led to the most modern offerings that a clinician would bring to a patient’s bedside to perform clinical examination.1,2,3 It has permitted appreciably more accuracy with the fourth pillar of examination: auscultation. However, the stethoscope did not meet immediate approval; in fact, far from it. Facing the same scrutiny our modern ultrasound devices face now, it was put through its paces. Indeed, modern ultrasound devices, especially portable ones, opened up doors that were previously closed in clinical examination as offered by the stethoscope decades ago.
The addition of a fifth pillar into the traditional examination subset with insonation can only benefit our patients.
Portable ultrasound is inarguably one of the many technological innovations that have gripped medical practice. There has been a wealth of publications regarding this easy-access modality and a seemingly exponential uptake of such devices over the last five years. Many individuals have their own devices, and many units and specialities use them in daily practice.
Handheld ultrasound devices (HUDs) may bridge the gap between large cart-based systems and laptop-based systems, providing a convenient happy medium. Some are priced such that users may purchase their own,4,5 although this relative inexpensiveness can lead to the purchase of these devices for novelty and convenience over need. Nonetheless, ultrasound learning can be integrated seamlessly into day-to-day practice.
Despite ongoing debate over the inclusion of ultrasound into everyday practice, ultrasound may be superior to traditional examination in many ways.6-13 Technology is continually advancing in modern medicine, and failure to grasp this concept may deny patients the most efficient care. HUDs (the stethoscope equivalent) permit us to “see” into the body, with insonation. This fifth pillar forms a bridge between clinical examination of the chest and further investigation, such as chest X-ray and computed tomography, although the former is more convenient and efficient.
Outcome data for the use of point-of-care ultrasound (POCUS) within the intensive care unit (ICU) setting are slowly emerging. A recent study showed that regular incorporation of POCUS into morning ICU rounds was associated with shortened duration of mandatory ventilation and length of ICU stay. This may be due to associated reduced fluid administration.14 There is paucity of evidence regarding the use of handheld devices for regional anesthesia and perioperative medicine; most discussion comes from word of mouth among peers or colleagues. We regularly perform perioperative ultrasound and regional anesthesia ultrasound using a range of portable devices within our practice. More studies are warranted to assess the feasibility, productivity, cost effectiveness, and outcomes using handheld devices for POCUS.
Patient engagement may be improved using handheld POCUS devices, as the acquired images are displayed and explained to them with more intimacy than is offered from a larger cart. The examiner is closer and can position the small, handheld screen nearer to the patient while the examination is in progress.15 This may promote increased compliance with the physician's advice and improved patient engagement and satisfaction with the examination as patients can visualize the pathology. Devices are small and less intimidating to patients as well as more readily accessible because departments can purchase a larger number of devices compared to more expensive, larger ultrasound machines. Many physicians also have their own devices due to affordability and the ability to readily transport devices between clinical areas. Another advantage is the aspect of cost effectiveness, through their low cost and ability to direct patients to appropriate diagnostic tests faster and, in some cases, avoid resource demanding transport for advanced imaging.16
The number of vendors providing handheld device has increased exponentially (Table 1), which in turn reduces costs because of the competitive marketplace.
Table 1. Brief Comparison of Handheld Devices
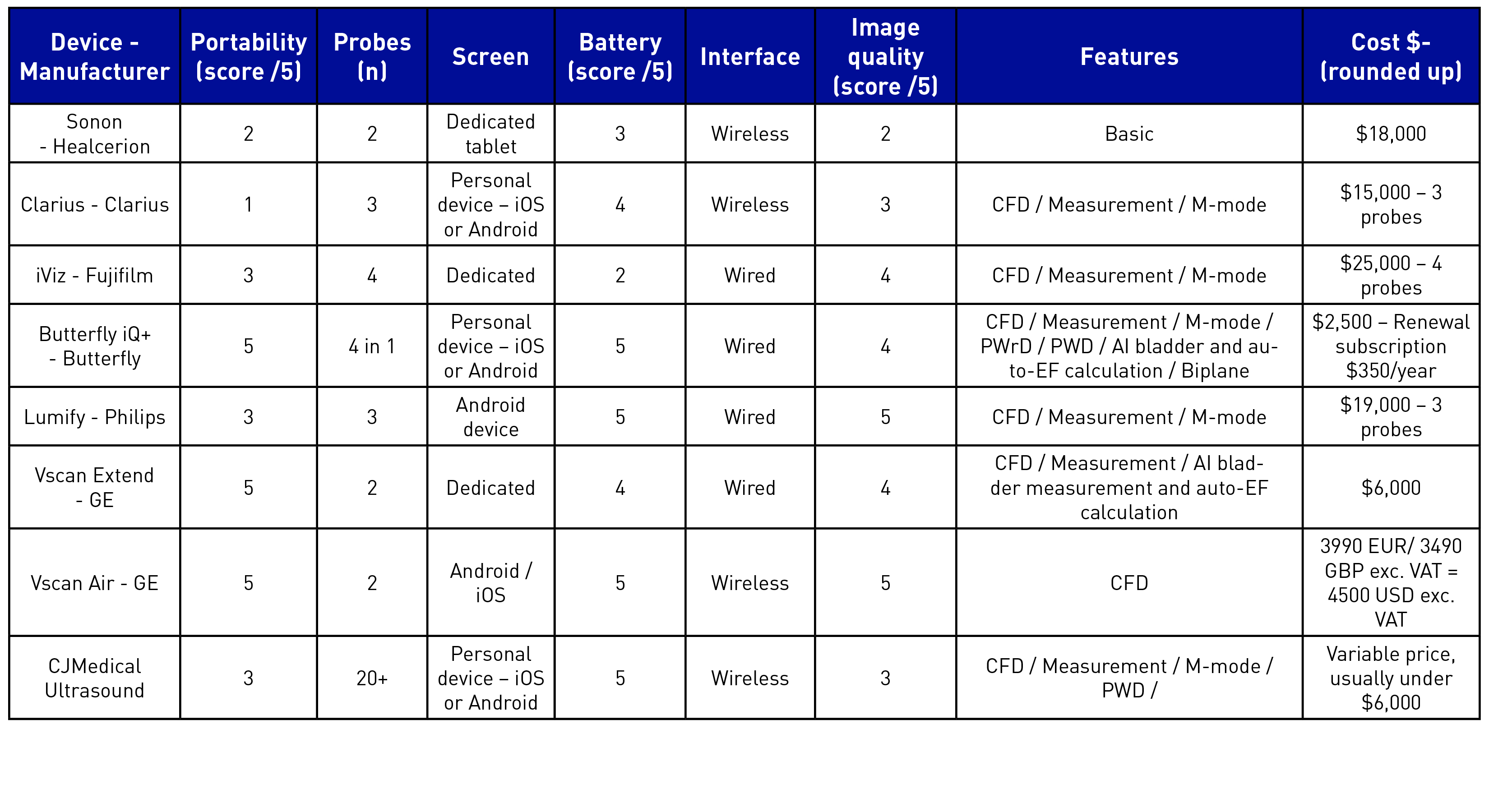
Key: CFD = Colour Flow Doppler / PWD = Pulsed Wave Doppler / PWrD = Power Doppler / AI = Artificial Intelligence / EF = Ejection Fraction
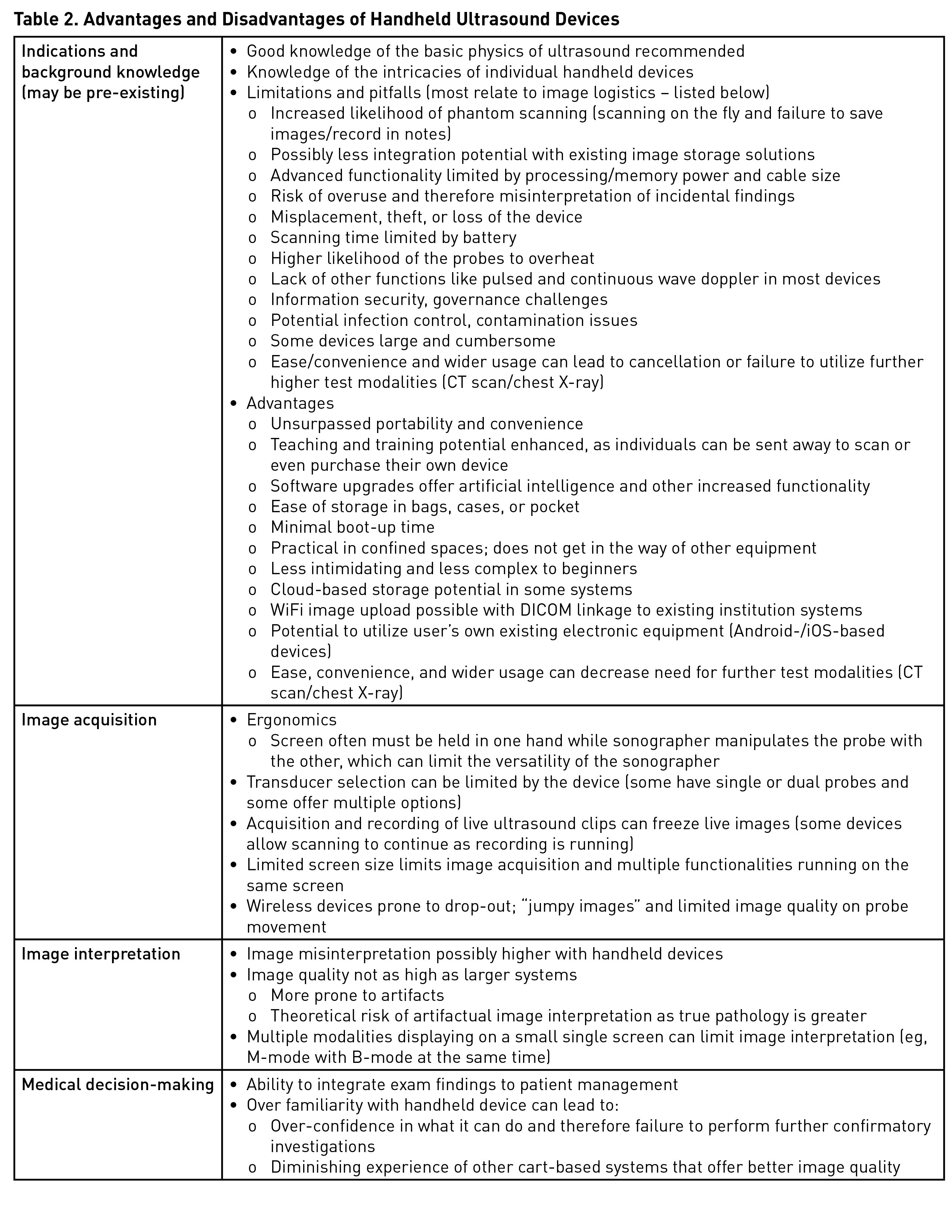
Despite all the advantages of handheld ultrasound machines, there are limitations in image quality as far as image size and resolution (Table 2). The latter is largely due to limited memory capacity to process higher-quality images. Physicians must exercise due diligence and caution while making potential treatment-changing decisions based on handheld device image sets. HUDs might be better viewed as tools to extend the physical examination, rather than tools for comprehensive diagnostics. They also can be a stepping stone for those training to become competent in advanced ultrasound applications, providing the initial training in image acquisition.17 Recognition of their drawbacks are necessary when making clinical decisions informed by handhelds. Failure to do so, especially in inexperienced hands, could lead to mismanagement of patients. By the same token, the devices should be utilized as tools for rule-in, rather than rule-out.
Many HUDs are designed to promote ease of use, with many taking advantage of the skillset required to operate most mobile phones and tablets (eg, swiping, zooming, dragging, operation of menus). Utilizing this basic, built-in skillset may give novice users an advantage to operate the system.
Medical schools also are employing HUDs both as part of the clinical POCUS curriculum and as tools for demonstrating functional anatomy.18,19 This approach equips learners with the additional skills of operation and interpretation of ultrasound imaging.
Fast forwarding into the future, HUDs may be widely incorporated into many specialties within health care, especially with their simple operating systems, convenience, and portability. We regularly use these devices on ICU ward rounds and while assessing patients on the ward, both as a part of routine clinical examination and for teaching junior colleagues.20 Their portability is invaluable during cardiac arrest calls. They also are available to the anesthesiologist in the operating room for regional anesthesia, vascular access, hemodynamic assessment, and lung ultrasound.
With increasing frequency and convenience of usage, so may follow transmission of contaminants between patients. This requires users to be vigilant with scrupulous decontamination of probes and the devices themselves. Stethoscopes also have long been recognised as sources of contamination. The COVID-19 pandemic has emphasised the need for scrupulous cleaning of these devices, as HUDs often were used over carts within isolation zones. During COVID-19, spread of resistant micro-organisms became frequent, as users donned personal protective equipment and stayed in them from patient to patient. Transmission undoubtedly occurred due to this, and similarly, the same could have occurred with probes or devices travelling across patients.21,22 Nonetheless, portable ultrasound machines are easier to decontaminate compared to traditional ultrasound machines.
When properly mentored with a solid governance infrastructure, the addition of a fifth pillar into the traditional examination subset with insonation can only benefit our patients. POCUS is not a replacement for a good physical examination, nor is it a replacement for detailed full-scale imaging. Portable or pocket ultrasound devices offer many advantages that may entice practitioners to use them over traditional ultrasound machines. One must recognize the limitations of portable ultrasound devices to ensure that these devices offer their maximum potential benefits. Could the panacea for all patients in the future be an ultrasound-assisted clinical examination augmented by pocket devices?

Jonathan N. Wilkinson, MBChB, MRCP, FRCA, FFICM, is a staff anesthesiologist, ICU clinical lead, and POCUS lead, at Northampton General Hospital in Northampton, UK. He is the founder of www.criticalcarenorthampton.com.

Nicolas Lim, FRCEM, FJFICMI, FFSEM, MRCSI, is an emergency physician and intensive care medicine fellow at the University College Hospital Galway in Galway, Ireland, and professor at the Ultrasound Leadership Academy, www.ultrasoundleadershipacademy.com.
References
- Laennec R. De l'auscultation médiate ou traité du diagnostic des maladies des poumon et du coeur. Paris: Brosson & Chaudé 1819.
- Laennec RTH, Forbes J. A Treatise on the Diseases of the Chest and on Mediate Auscultation. New York: Samuel Wood & Sons 1835.
- Roguin A. Rene Theophile Hyacinthe Laënnec (1781–1826): the man behind the stethoscope. Clin Med Res 2006;4(3):230-5. https://doi.org/10.3121/cmr.4.3.230.
- Comstock J. UC Irvine Medical School gifts Butterfly handheld ultrasounds to its whole class of 2023. Mobihealthnews 2019, August 26. https://www.mobihealthnews.com/news/north-america/uc-irvine-medical-school-gifts-butterfly-handheld-ultrasounds-its-whole-class. Accessed November 3, 2019.
- Elder A, Japp A, Verghese A. How valuable is physical examination of the cardiovascular system? BMJ 2016;354. https://doi.org/10.1136/bmj.i3309.
- Mehta M, Jacobson T, Peters D, et al. Handheld ultrasound versus physical examination in patients referred for transthoracic echocardiography for a suspected cardiac condition. JACC Cardiovasc Imaging 2014;7:983-90. https://doi.org/10.1016/j.jcmg.2014.05.011.
- Mjolstad OC, Dalen H, Graven T, Kleinau JO, Salvesen O, Haugen BO. Routinely adding ultrasound examinations by pocket-sized ultrasound devices improves inpatient diagnostics in a medical department. Eur J Intern Med 2012;23:185-91. https://doi.org/10.1016/j.ejim.2011.10.009.
- Skjetne K, Graven T, Haugen BO, Salvesen Ø, Kleinau JO, Dalen H. Diagnostic influence of cardiovascular screening by pocket-size ultrasound in a cardiac unit. Eur J Echocardiogr 2011;12:737-43. https://doi.org/10.1093/ejechocard/jer111.
- Haji DL, Royse A, Royse CF. Review article: clinical impact of non-cardiologist-performed transthoracic echocardiography in emergency medicine, intensive care medicine and anaesthesia. Emerg Med Australas 2013;25:4-12. https://doi.org/10.1111/1742-6723.12033.
- Goonewardena SN, Gemignani A, Ronan A, et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging 2008;1:595-601. https://doi.org/10.1016/j.jcmg.2008.06.005.
- Prinz C, Voigt JU. Diagnostic accuracy of a hand-held ultrasound scanner in routine patients referred for echocardiography. J Am Soc Echocardiogr 2011;24:111-6. https://doi.org/10.1016/j.echo.2010.10.017.
- Panoulas VF, Daigeler AL, Malaweera ASN, et al. Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur Heart J Cardiovasc Imaging 2013;14:323-30. https://doi.org/10.1093/ehjci/jes140.
- Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol 2005;96:1002-6. https://doi.org/10.1016/j.amjcard.2005.05.060.
- Chen Z, Hong Y, Dai J, Xing L. Incorporation of point-of-care ultrasound into morning round is associated with improvement in clinical outcomes in critically ill patients with sepsis. J Clin Anesth 2018;48:62-6. https://doi.org/10.1016/j.jclinane.2018.05.010.
- Portable ultrasound improves patient understanding, quality of care. Becker’s Clinical Leadership & Infection Control. https://www.beckershospitalreview.com/quality/portable-ultrasound-improves-patient-understanding-quality-of-care.html. Accessed November 11, 2019.
- Greaves K, Jeetley P, Hickman M, et al. The use of hand-carried ultrasound in the hospital setting – a cost-effective analysis. J Am Soc Echocardiogr 2005;18:620-5. https://doi.org/10.1016/j.echo.2004.09.015.
- Mulvagh SL, Bhagra A, Nelson BP, Narula J. Handheld ultrasound devices and the training conundrum: how to get to “seeing is believing”. J Am Soc Echocardiogr 2014;27:310-3. https://doi.org/10.1016/j.echo.2014.01.011.
- Kim EY, Park KH, Choi SJ, Chung W-J. Educational value of pocket-sized ultrasound devices to improve understanding of ultrasound examination principles and sonographic anatomy for medical student. PLoS One 2017;12(9):e0185031. https://doi.org/10.1371/journal.pone.0185031.
- Swamy M, Searle RF. Anatomy teaching with portable ultrasound to medical students. BMC Med Educ 2012;12:99. https://doi.org/10.1186/1472-6920-12-99.
- Hospital trials pocket-sized ultrasound device that plugs into iPhone. Sky News 2019, September 26. https://news.sky.com/story/hospital-trials-pocket-sized-ultrasound-device-that-plugs-into-iphone-11818586. Accessed January 27, 2020.
- Russotto V, Cortegiani A, Raineri SM, Giarratano A. Bacterial contamination of inanimate surfaces and equipment in the intensive care unit. J Intensive Care 2015;3,54. https://doi.org/10.1186/s40560-015-0120-5.
- Marinella MA, Pierson C, Chenoweth C. The stethoscope: a potential source of nosocomial infection? Arch Intern Med 1997;157:786–90. https://doi.org/10.1001/archinte.1997.00440280114010.
Leave a commentOrder by
Newest on top Oldest on top