Five Institutions Share Their Perspectives on the Future of Chronic Pain Fellowship Training and Key Advice for Aspiring Pain Fellows
Cite as: Francio VT. Five institutions share their perspectives on the future of chronic pain fellowship training and key advice for aspiring pain fellows. ASRA Pain Medicine News 2022;47. https://doi.org/10.52211/asra020122.011.
Innovative interventions and promising outcomes are evolving the field of chronic pain medicine, including fellowship training. Programs have adapted to newer technologies and research to become more competitive than ever, attracting applicants from multiple specialties, while adjusting to today’s challenges.1–3
Applicants say they are drawn to the chronic pain subspecialty because of interest in procedural skills, personal experiences with pain, mentor guidance, and a desire to help a population in need.4 Current literature is helpful in understanding fellowship matching trends; however, applicants say that the key factors essential to a successful chronic pain fellowship are still unclear.
What makes an applicant a good pain fellow? What concepts in chronic pain medicine are important for aspiring fellows to understand? What challenges should aspiring fellows prepare for when transitioning from residency to fellowship or fellowship to practice? What changes are anticipated in future chronic pain fellowship training? And how do fellows adapt to those changes?
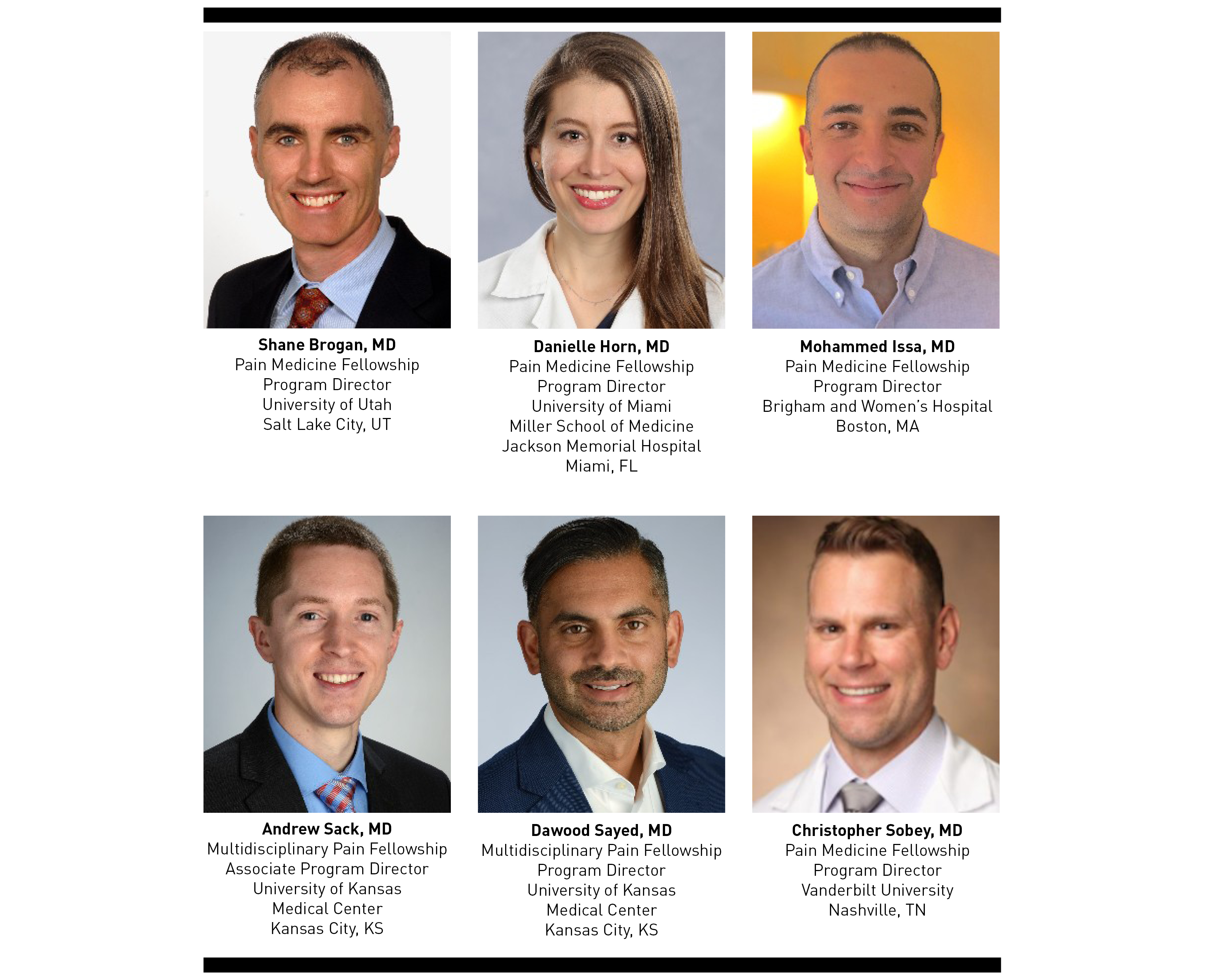
With those questions in mind, I approached chronic pain fellowship program directors (PDs) from five institutions across the United States for an interactive discussion about future perspectives in fellowship training and key factors for aspiring fellows joining the specialty making a prescient topic as we approach chronic pain fellowship interview season.
What Makes a Good Pain Fellow?
Christopher Sobey, MD: Building a fellowship class is about accumulating a complementary team capable of producing durable outcomes from their work while fostering diverse personalities, enthusiasm, and readiness to learn from and care for their patients. In the world of pain, a sympathetic demeanor is a must.
Shane Brogan, MD: Fellows should be from a diverse background, motivated to learn all aspects of interdisciplinary pain management, fun to be around, and good team players.
Danielle Horn, MD: Empathy, kindness, compassion, dedication, and a continuous desire to learn with a strong investment in helping patients improve their quality of life are key values for pain fellows.
Andrew Sack, MD: It is important for applicants to understand the landscape in the fast-paced industry of pain medicine. Motivation and an eagerness to learn are key, along with a sincere interest to help patients long term.
Mohammed Issa, MD: Passion for the field, leadership skills, and teamwork are the top three important characteristics for pain fellows. Passion drives creativity, which in turns drives discovery and entrepreneurship in the growing field of pain medicine.
What Do You Look For in an Applicant?
Sayed: I seek a genuine interest and strong commitment to the specialty of pain medicine—and often that is evidenced by an applicant’s scholarly activities, academic success during residency, leadership engagement, and outstanding letters of recommendation (LORs) reflecting their dedication to the field.
Sobey: Understanding a candidate’s personality and whether it fits in an institution is difficult based solely on paper applications, so LORs with good insight on their clinical experience and technical skills are usually the best way to determine whether they have traits that would translate to success in pain medicine. In-training exams and board scores may predict whether a candidate is likely to pass their primary and specialty boards; however, they are not a sole determining factor. Scholarly productivity is an important factor to demonstrate dedication to the specialty.
Horn: The best gauge we have for an applicant’s work ethic and commitment to the specialty comes from references from their residency training, so applicants should focus on excelling while in training.
Issa: I watch for passion, a sense of teamwork, and leadership skills to lead all aspects of pain medicine to the next level, both nationally and globally.
What Are the Important Concepts That Aspiring Pain Management Fellows Should Understand?
Sack and Sayed: A fundamental starting block is understanding the pathophysiology, pharmacology, and anatomy involved in pain. Applicants also should have insight into how physiologic and psychological comorbidities influence chronic pain. Then, trainees can progress to advanced strategies for recognizing and treating complex pain. Excellent procedure skills prior to fellowship are not critical, but adaptability, teachability, and a strong desire to learn are.
Sobey: Fellows should understand some foundational aspects of pain medicine, such as etiology and evidence-based treatment of the most common musculoskeletal and neurologic pain conditions. Knowledge of controlled substances, risks and consequences of chronic prescribing, and enacted or proposed policy mitigation strategies is also important. Many fellows have an eye-opening experience when they see how opioid treatments for pain overlap with dependency and addiction, and they must understand how to minimize risks while properly treating a patient’s debilitating pain.
Issa: Among the many concepts already cited, fellows should understand appropriate differential diagnosis and the pain physician's toolbox: medication management, therapy interventions, complementary treatments, and, most importantly, that chronic pain always comes along with an affective component.
Brogan: Aspiring fellows must understand and embrace the complexity of chronic pain and the need for interdisciplinary management involving other specialties, therapists, and the patient and family.
Horn: Understanding the therapies, interventions, and implantable devices that can help treat chronic pain is important; however, we must remember that those interventions are not a cure for pain and the most beneficial services we can provide our patients are compassion, empathy, and time. Dealing with pain on a long-term basis is often debilitating and extremely taxing for patients, so it is integral that physicians make sure that patients feel that they are heard and seen, their experience are listened to, and that they are receiving the best care possible. There is no simple algorithm to follow, and each person deserves an individualized and tailored plan based on their condition, financial ability, and social support.
What Changes Do You Foresee in Chronic Pain Fellowship Training?
Issa: Fellowships will continue to advance with training in further innovative minimally invasive surgical pain management and procedures to replace more judicial use of opioids for treatment of chronic non-cancer pain. We will foster this by continuing to further expand our sites, so fellows can get more comprehensive and surgical pain management training.
Horn: As a large academic center, we are fortunate to be involved in several clinical trials, which gives trainees and faculty the opportunity to learn about the latest therapies that may become standard options in the future. Also, we are focused on providing multidisciplinary care and encouraging self-management, including physical and behavioral rehabilitative techniques, in addition to pharmacologic and interventional options.
Sobey: Pain medicine is an incredibly broad, developing, and rapidly changing field. Consolidating specialty knowledge into one year of learning becomes more difficult each year. Pain faculty need to stay up to date with their own education in novel treatments that might not have been validated or even existed during their training. Fellowship programs also need to offer enough patients entailing the broad array of pain issues for fellows to not only learn from the literature, but have hands-on experience with innovative treatments.
Sack and Sayed: We shape the future of the specialty when we expose fellows to advanced pain procedures and multidisciplinary pain treatments. As the specialty advances, it offers fellows opportunities to participate in cutting-edge research and be directly involved in hands-on innovative chronic pain treatments. Those rapid advancements require us to adapt quickly to innovative options, and the future may include an advanced pain medicine integrated track in training or pain medicine becoming its own residency.
Brogan: As our interventional techniques rapidly evolve and methods become more sophisticated, we may require different training paradigms, such as a categorical pain residency program system with an abbreviated core residency. Alternatively, albeit less popular, a two-year fellowship could offer more rigorous clinical education, business management training, and a research component.
What Challenges Are Important for Aspiring Fellows to Anticipate When Transitioning From Residency to Fellowship to Practice?
Brogan: Fellowship demands an entirely different set of skills, including effective, productive, and longitudinal patient care.
Sack: An understanding of patient-relationship and continuity of care is one of the most important challenges and a vital aspect of fellowship that often is overlooked during residency training, especially those with a background in anesthesiology. Maintaining excellent patient rapport during pain fellowship is fundamental along the process of addressing complex symptoms and differential diagnosis, while maximizing interventional outcomes, tracking multiple follow-up visits, and building your practice referral.
Horn: Take advantage of your fellowship to soak up knowledge and skills, learn efficiency, and develop your own style. Following fellowship, stay proactive with continuous education. When searching for a job, financial incentives are important, but do not let them be the only guide to your decision. The type of work you will do, personalities in the practice, geography, and other job attributes may be equally, if not more, important than your salary.
Sobey: The most obvious change is the level of ownership of a patient, such as knowing what to do in certain scenarios, determining a diagnosis, performing a procedure, or conveying information to the patient or family. Along that transition, fellows are exposed to the financial aspects of the specialty and gain skills in practice management, billing, and communicating with insurance companies, which are essential to understand prior to real-world practice management and vital to keep the lights on in the clinic.
Issa: The most important challenge is understanding the changes in role and level of independence that come with each transition, including residents’ teaching and supervising responsibilities, which progressively grow from fellowship to an independent practice. When transitioning into the real world, fellows should understand that most of the learning curve comes in the first year after a fellowship and that it is okay to go slow as they improve their confidence and skills in a team environment.
Sayed: The first year out of fellowship is critical. Consider it fellowship number two, because you learn just as much as in your actual fellowship. Pain medicine is rapidly evolving, and adaptability is key. And stay in active contact with your fellowship mentors, who can offer life-long mentorship and collaboration after your official training ends.
What Are Your Words of Wisdom for Aspiring Pain Fellows?
Issa: Pain medicine is one of the fastest-growing fields in medicine. Most programs have more applicants than available positions, and the pool of applicants grows every year. Demonstrating an early interest and work on pain-related projects will show that fellows will go “an extra mile” to faculty, and their LORs will demonstrate true passion, interest, and teamwork. It fuels an energy in letter writers that can be felt when trying to select the top of the list from hundreds of letters.
Sobey: One year is a very short amount of time to acquire all the information needed to have a successful career. I recommend trying to absorb and be involved in as much as possible. By engaging completely in clinical care, staying up to date on knowledge acquisition, and not taking the opportunity of the fellowship experience for granted, fellows can leave their training feeling confident in their abilities to care for a challenging patient population. Take advantage of all that the faculty have to offer as well as educational opportunities available by pain societies like ASRA Pain Medicine. Go to work each day with the goal of making a difference in patients’ lives.
Horn: It is never too soon to start reading and building your knowledge base; establish that habit because you will never stop learning. Lean into the challenge, do your best to excel, and provide your patients with the kind of care you would want for yourself or your most beloved family member. Spend time in the pain center, not only in the procedure suite, but also in the clinic. Make sure that you enjoy the physical, psychological, pharmacologic, and interventional aspects of the specialty.
Brogan: Be the best resident you can be, even if you think you will not eventually practice your core specialty. Your effort will be reflected in your LORs. Being “checked out” in your core specialty reflects poorly on your integrity and work ethic. Express an early interest in the field, and try to do elective rotations as soon as possible so you can verify that the specialty is a good fit for you. Make sure you obtain LORs from pain physicians. Participate in pain society meetings, seek out a mentor in pain medicine, and engage in scholarly activities. If you are interested in a particular program and you do not get invited to interview, consider reaching out to the program and expressing your genuine interest.
Sack: Demonstrating a sincere interest in chronic pain medicine with accomplishments throughout residency training, such as scholarly activities and presentations with novel ideas that show commitment to the specialty, is important. An incredible trait to pain medicine physicians is the ability to work well with others and exhibit excellent rapport with coworkers, staff, and patients.
Conclusion
Genuine interest and early commitment to pain medicine, built on a progressive pattern of scholarly activities, leadership opportunities in society committees, and forthright LORs, are key factors for fellowship applicants to succeed. Networking with and seeking mentorship from pain leaders are also essential to recognizing whether the specialty is an appropriate fit for an applicant. Ask questions and take time to understand the issues facing the specialty and the business aspects of medicine. This will help a pain medicine physician develop the essential traits to deal with future perspectives and real-life situations and to intelligibly comprehend the specialty’s rapidly evolving landscape.

Vinicius Tieppo Francio, MD, MS, is a resident physician at the University of Kansas Medical Center in Kansas City.
References
- NRMP Results and Data Fellowship Appointment, February 2021. Available at https://www.nrmp.org/wp-content/uploads/2021/08/SMS_Result_and_Data_2021.pdf. Accessed January 20, 2022.
- Kohan L, Moeschler S, Spektor B, et al. Maintaining high-quality multidisciplinary pain medicine fellowship programs: part I: innovations in pain fellows’ education, research, applicant selection process, wellness, and ACGME implementation during the COVID-19 pandemic. Pain Med. 2020;21(8):1708–17. https://doi.org/10.1093/pm/pnaa168
- Kohan L, Sobey C, Wahezi S, et al. Maintaining high-quality multidisciplinary pain medicine fellowship programs: part II: Innovations in clinical care workflow, clinical supervision, job satisfaction, and postgraduation mentorship for pain fellows during the COVID-19 pandemic. Pain Med. 2020;21(8):1718–28. https://doi.org/10.1093/pm/pnaa176
- Belgrade M, Belgrade A. Why do physicians choose pain as a specialty? Pain Med. 2020;21(11):2743–7. https://doi.org/10.1093/pm/pnaa283
Leave a commentOrder by
Newest on top Oldest on top