The Ups and Downs of Innovation: Lessons from a Chronic Pain Management Clinical Decision Support Project
Cite as: Cassidy K, Kao C-K. The ups and downs of innovation: lessons from a chronic pain management clinical decision support project. ASRA Pain Medicine News 2022;47. https://doi.org/10.52211/asra050122.024
Patients need to be understood as key participants in their own health care, and none more so than those living with chronic illness and pain. The trend toward shared decision making (SDM) has been game-changing for the relationship between providers and patients, and recent developments in technology have enabled new ways to support those conversations. The electronic health record (EHR) serves as a preexisting resource, and it will be crucial to establish a framework to capture patient-reported outcomes (PROs) via EHR-based surveys systemically. This data will be the frontier of SDM conversations in the future.
The lessons from the past two years will have a lasting impact ... in fostering both new technologies and bold ideas: to center the relationship between patients and their providers and to empower them to make decisions together to serve the patient’s health and goals.
In October 2019, UChicago Medicine (UCM)’s Center for Healthcare Delivery Science and Innovation embarked on a two-year, multi-institutional project to move the conversation forward around managing chronic pain. Supported by a $4 million contract from the Agency for Healthcare Research and Quality, the team was comprised of faculty and staff at UCM, Research Triangle Institute (RTI) International, Vanderbilt University Medical Center (VUMC), Alphora LLC (a database consulting group), a patient advocate, and expert informatics consultants. The goal of the project was to create, implement, and test SDM tools that could be publicly available and employed by different health systems with relative ease.
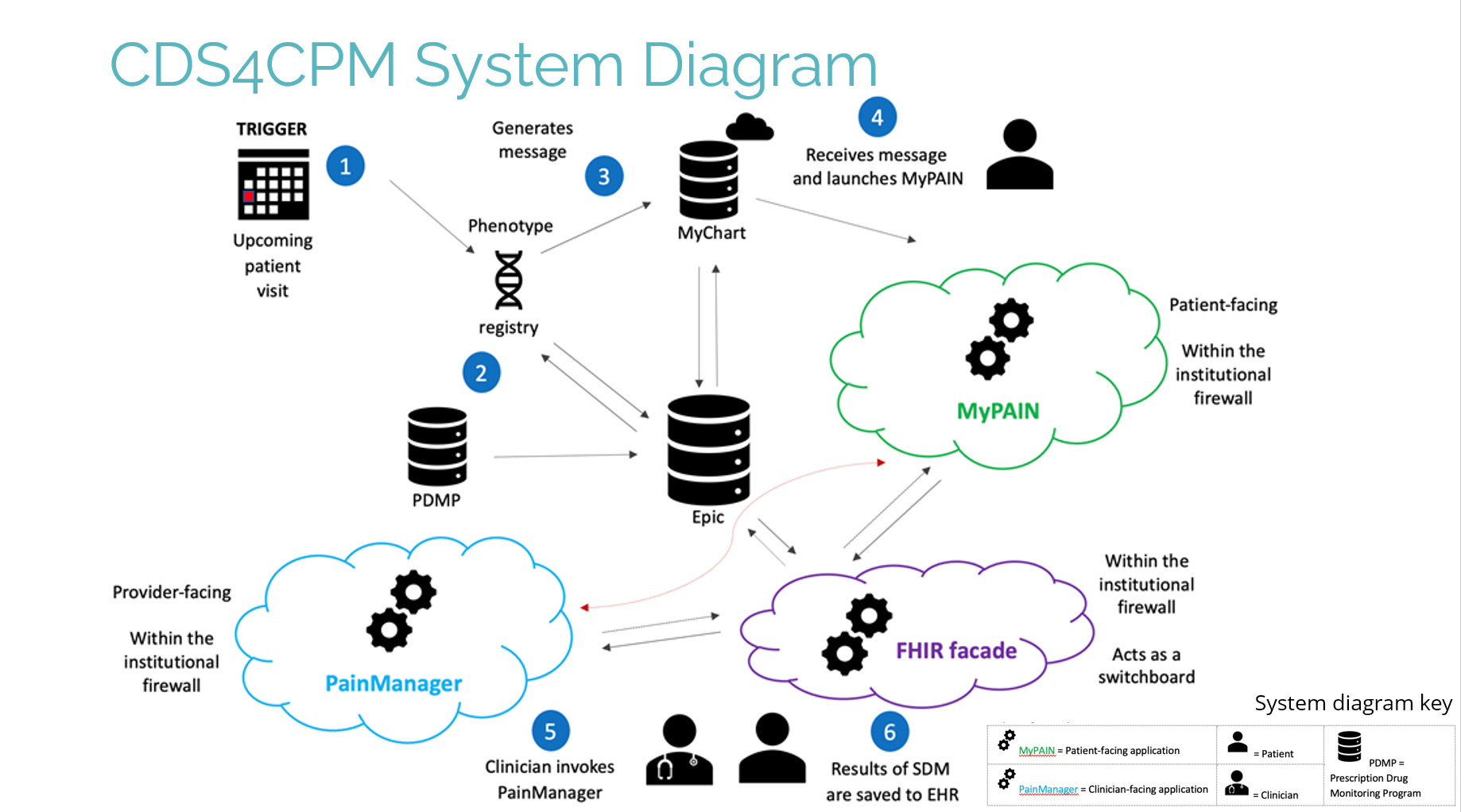
Working in collaboration between the health systems and the developer, Alphora, the team successfully designed and developed two apps to support SDM between patients and providers. The first, developed specifically for this project, was MyPAIN, a survey app sent to patients prior to their appointments via their MyChart appointment reminders. The second, adapted from an existing tool, was PainManager, a dashboard app accessed from within the EHR that shows the results of the MyPAIN survey, along with other relevant patient information (Figure 1).
Figure 1. System Diagram
UCM launched a two-month pilot of the two apps from March to May 2021 with 15 providers in four clinics, including both primary care and a specialty pain clinic. The VUMC pilot included 10 providers across three clinics.
The MyPAIN app worked well; it successfully captured patient-reported data and sent it to the EHR database. Without any aggressive promotion, about 15%-20% of patients clicked on the invitation link in the MyChart reminder message and completed the MyPAIN survey. The pilot implemented the MyPAIN link only in the patient’s appointment reminder; however, the team recognizes the need to create a parallel workflow to capture the PROs in the clinic if patients do not complete the MyPAIN survey, especially those with digital literacy issues.
As an Illinois-based institution, UCM planned to include data from the Illinois Prescription Monitoring Program (PMP) database in the PainManager dashboard. However, UCM encountered challenges to integrating the unreconciled state PMP database into the app; the database was digitized, but sharing was restricted by the state. As a result, PMP data was not incorporated into the dashboard.
Across the span of several months, members of each institution’s teams spent countless hours every week on video calls to solidify the design and troubleshoot unknown errors in implementation. The COVID-19 pandemic slowed down the project as well, as the health system focused on addressing the immediate crisis. Despite delaying the pilot to implement fixes to PainManager, the tool continued to experience operational issues, including long load times and crashes, which made it difficult to use in clinic settings. The team ultimately created an alternative report within the EHR so that providers could view MyPAIN survey data in an easier way. The ongoing IT maintenance and enhancement of a third-party app will be a challenge in the long run.
From a technology perspective, although UCM had prior experience in successfully deploying Fast Healthcare Interoperability Resources (FHIR)-based tools for clinical workflows, the particular back-end technology used to implement PainManager and MyPain was relatively new - a "FHIR façade" that allows for access to data from legacy systems via the FHIR standard. Although this project’s pilot period did not demonstrate feasibility for sustaining PainManager, John Moses, IT Research Lead at UCM, noted, “I view this as a valuable learning experience on the best ways to design and implement portable technologies and repeatable processes within the health care space. The lessons learned will be applied to future initiatives both within and beyond UCM.” In addition, a forthcoming publication from RTI will provide more details on implementing these particular tools and add to the national conversation around the patient voice in chronic pain management.
Innovation naturally involves trying new ideas and practices, and some don’t work out exactly as planned. The path has proven to be difficult in the current environment, where interoperability and sustainability remain a challenge, but we have gained valuable insights from this project about the problems and opportunities in the space, which will inform our future strategy to design, develop, and adopt similar technology. The lessons from the past two years will have a lasting impact for UChicago Medicine and the national efforts in fostering both new technologies and bold ideas: to center the relationship between patients and their providers and to empower them to make decisions together to serve the patient’s health and goals.

Kimisha Cassidy, MS, is a project manager in the Center for Healthcare Delivery Science and Innovation at UChicago Medicine in Chicago, IL.
Leave a commentOrder by
Newest on top Oldest on top