Major Changes in Medicare Physician Payments for Calendar Year (CY) 2021
In accordance with final regulations released by the Centers for Medicare and Medicaid Services (CMS) and statutory changes enacted by Congress, several major changes to Medicare physician payment have taken effect for 2021. Highlights are provided below.
- Reduction in the Medicare Physician Fee Schedule (MPFS) Conversion Factor. The MPFS conversion factor for CY 2021 is 34.8931, which reflects a 3.3 percent reduction for 2021 relative to 2020.
- Changes in documentation, coding, and payment for office and outpatient evaluation and management (E/M) services. CMS finalized significant changes for office and outpatient E/M services, effective January 2021. These include the following:
- Documentation. CMS generally adopted revisions to documentation requirements recommended by the CPT Editorial Panel for office and outpatient E/M visits. Under the new requirements, level selection and documentation requirements may be determined based on either medical decision making (MDM) alone, or time alone. History and physical are no longer determinants for selecting levels. MDM criteria have been modified to increase clarity and redefine data elements. For level selection based on time, total time requirements account for both face-to-face and non-face-to-face time personally spent by the physician or other qualified health care professional on the day of the encounter. Total time requirements are identified in updated code descriptors, as shown in Table 1 below.
- Coding. CMS largely adopted the CPT Editorial Panel’s recommendations for revised coding of office and outpatient E/M visits, including eliminating coding for Level 1 new patient visits. A full discussion of the 2021 CPT recommended changes is included on the American Medical Association (AMA) website. However, CMS adopted a modified version of the CPT prolonged service code; rather than CPT 99417 (formerly 99XXX), CMS adopted a new G-code that requires the maximum amount of time for a level 5 office/outpatient E/M visit to be exceeded by at least 15 minutes before the code can be billed when level selection is based on time (see Table 1). CMS also prohibited the use of two existing prolonged services codes, 99358 and 99359, in conjunction with office and outpatient E/M visits starting in 2021.[1]
- Payment. CMS largely adopted RUC-recommended values for the office and outpatient E/M visits. Values were based on a cross-specialty survey, reflecting increases of between 0 to 46 percent in work RVUs for the office and outpatient E/M codes. Updated work RVUs for 2021 are shown in Table 1 below.
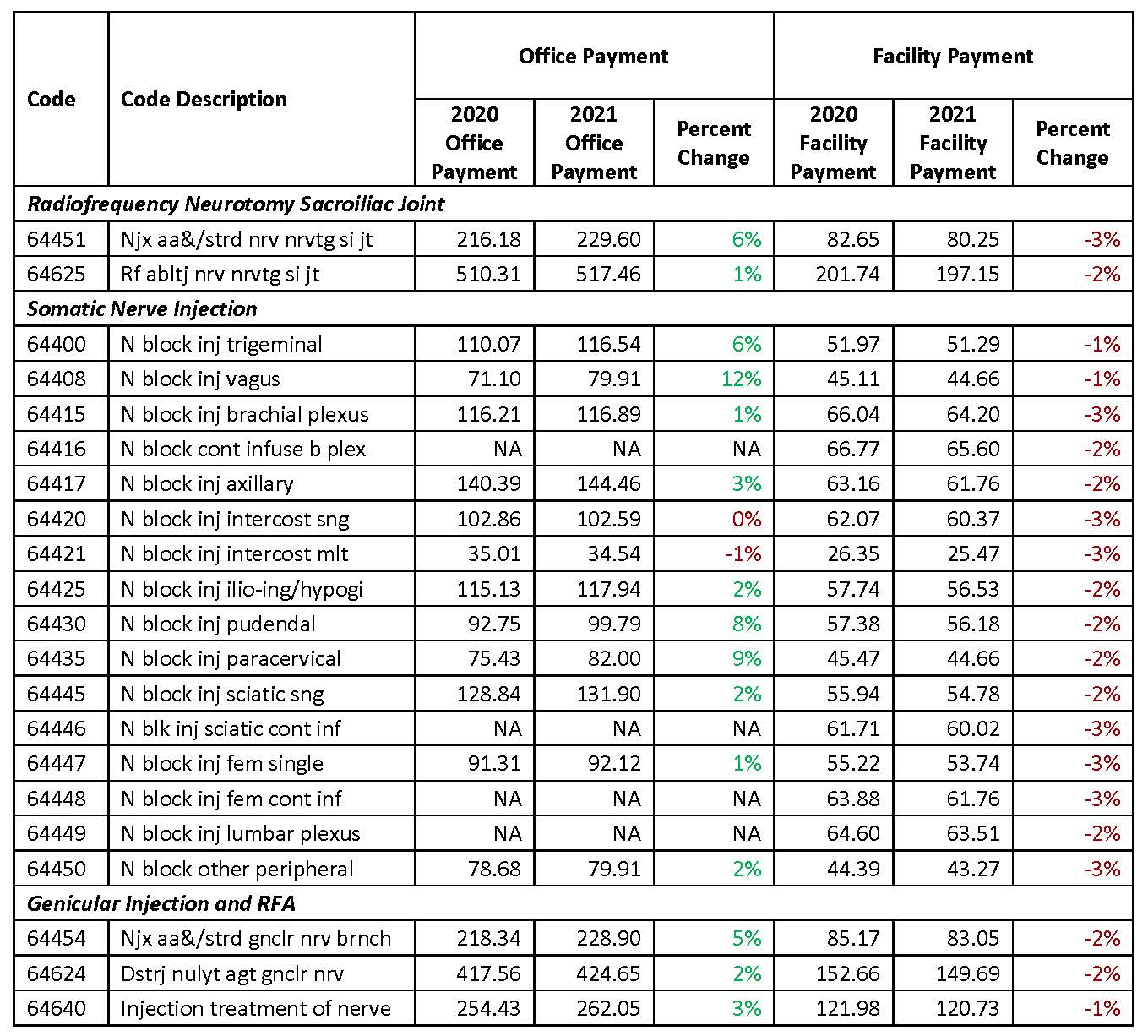
- Payment changes for common procedures. Many procedures commonly furnished by ASRA members are seeing payment changes for 2021. These include several procedures that are experiencing higher payments when furnished in the office, while at the same time they are experiencing payment reductions when furnished in the facility setting. This disparity is largely due to increases in practice expense RVUs for office settings that overcome the reductions in payment driven by the lower conversion factor; PE changes for facility-based settings, however, were relatively limited, allowing the conversion factor reduction to dominate. Table 2 identifies payment changes from 2020 to 2021 for common procedures.
- Medicare sequester reductions. In response to the coronavirus pandemic, Congress suspended the 2 percent sequestration reduction in Medicare payments from May 1, 2020 through March 31, 2021. Absent further Congressional action, Medicare payments will again experience a 2 percent reduction starting April 1, 2021.
Additional information on the office and outpatient E/M changes can be found on in this CMS Fact Sheet.
Table 1: Select Office and Outpatient E/M Codes and Updated Descriptions and Work RVUs, Effective 1/1/2021
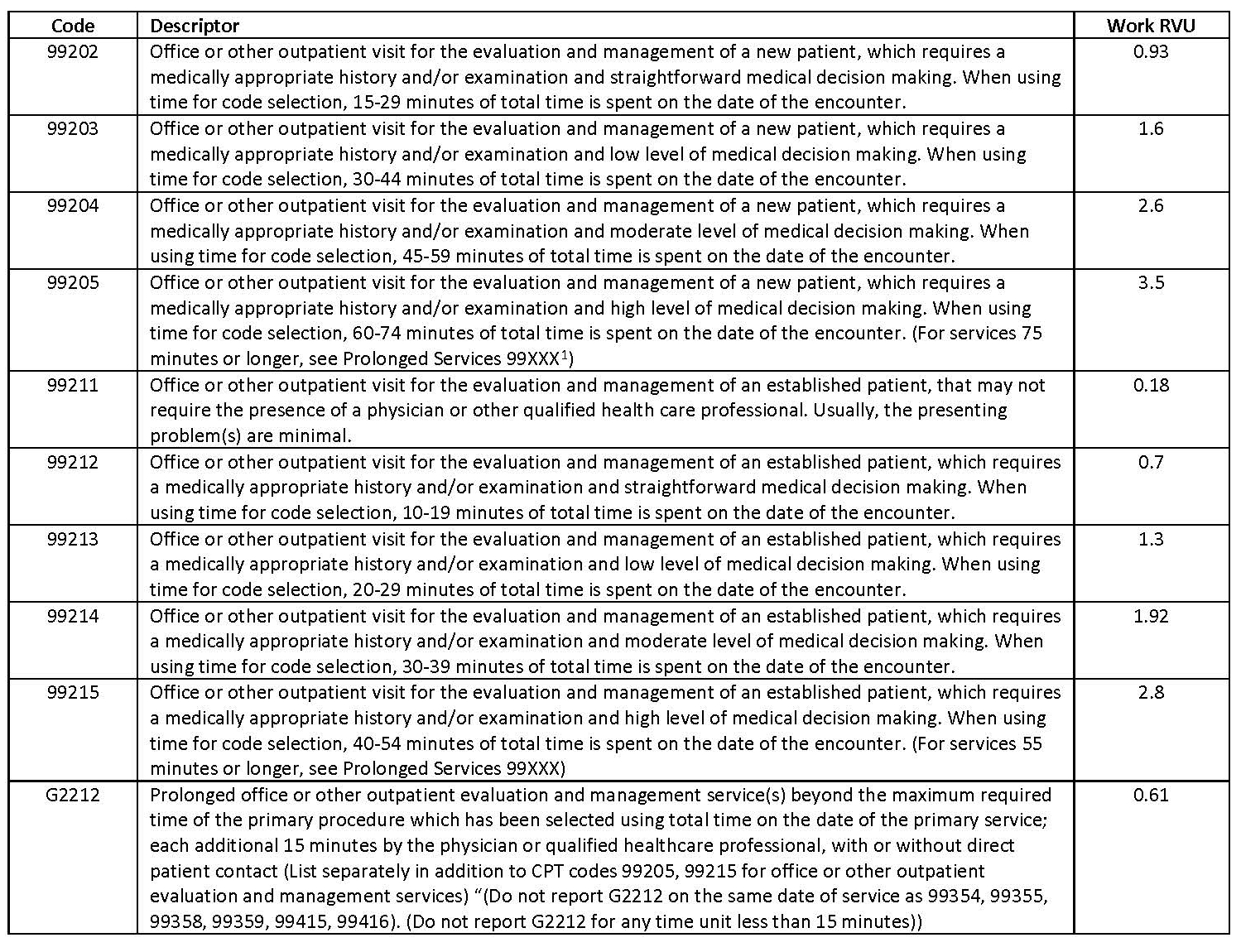
Table 2: Changes in Payment for Common Procedures
References to 99XXX in code descriptors reflect original CPT coding, as finalized in 2019. See on the AMA website here. These references do not take into account the more recent assignment by the CPT Editorial Panel of code 99417 to this service, nor CMS’ final policy to replace 99417 with G2212.
While CMS also finalized the addition of a separate add-on G-code for CY 2021 to address complexity for certain types of E/M services that reflect ongoing, longitudinal care (G2211/formerly GPC1X), the Consolidated Appropriations Act of 2021 (PL 116-260) prohibited CMS from making payment for this code prior to January 1, 2024. In the CMS Fact Sheet, CMS notes that practitioners may report this code starting in 2021, but CMS has assigned a payment indicator of “B” (Bundled) until 2024. Additional information on CMS’ expectations for use of G2211 – as released prior to the enactment of the Consolidated Appropriations Act of 2021 – can be found in the preamble of the CY 2021 MPFS final rule.
Leave a commentOrder by
Newest on top Oldest on top