An Introduction to Medicare Chronic Pain Management Codes for 2023
Dec 23, 2022, 00:00 AM
by
ASRA Pain Medicine
As part of our commitment to keep you informed on important payment and Medicare information, ASRA Pain Medicine's partner Heart Health has developed this explainer on the Calendar Year (CY) 2023 Medicare Physician Fee Schedule (MPFS) Final Rule.
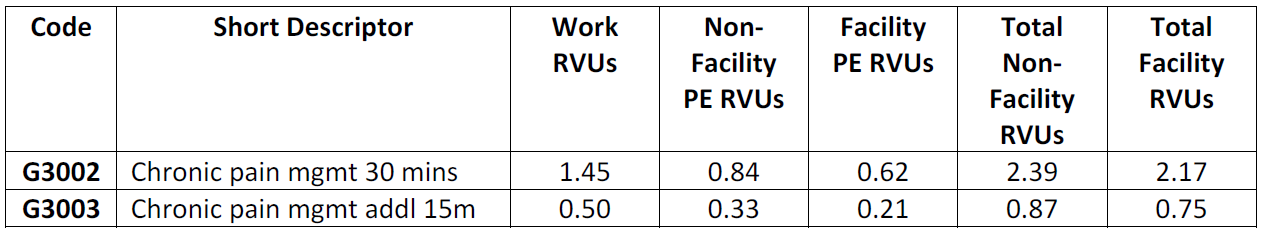
The Centers for Medicare and Medicaid Services (CMS) has finalized coverage and payment of new chronic pain management (CPM) bundled payment codes, effective January 1, 2023. Coverage of these services reflects CMS’s interest in improving the care experience for individuals with chronic pain and more appropriately reflecting the time and resources involved in furnishing comprehensive CPM services.
- G3002: Chronic pain management and treatment, monthly bundle including, diagnosis; assessment and monitoring; administration of a validated pain rating scale or tool; the development, implementation, revision, and/or maintenance of a person-centered care plan that includes strengths, goals, clinical needs, and desired outcomes; overall treatment management; facilitation and coordination of any necessary behavioral health treatment; medication management; pain and health literacy counseling; any necessary chronic pain related crisis care; and ongoing communication and care coordination between relevant practitioners furnishing care, e.g. physical therapy and occupational therapy, complementary and integrative approaches, and community-based care, as appropriate. Required initial face-to-face visit at least 30 minutes provided by a physician or other qualified health professional; first 30 minutes personally provided by physician or other qualified health care professional, per calendar month. (When using G3002, 30 minutes must be met or exceeded.)
- G3003: Each additional 15 minutes of chronic pain management and treatment by a physician or other qualified health care professional, per calendar month. (List separately in addition to code for G3002. When using G3003, 15 minutes must be met or exceeded.)
Billing for these codes must be consistent with the service as specified in the code descriptors. CMS also finalized the following additional guidelines and requirements for billing the codes:
- The initial visit must be conducted in person, face-to-face, by a physician or other qualified health care professional (QHP), for at least 30 minutes, with both the physician or QHP and the patient in a clinical setting. After the initial visit, the in-person components included in the codes may be furnished via telehealth, as applicable and clinically appropriate. And certain elements of the proposed bundle, such as care planning or care coordination with other health professionals, would not necessarily require face-to-face care.
- Services may not be furnished by auxiliary personnel incident to a physician’s (or other QHP’s) professional services.
- Verbal beneficiary consent must be provided at the initiating visit and must be documented in the beneficiary’s medical record. Beneficiaries should be educated regarding what the CPM services are, how often they may generally expect to receive the services, and what cost sharing may apply in their particular situation.
- CPM services may be billed on the same date as evaluation and management (E/M) services, or in the same month as remote physiologic monitoring (RPM) services, remote therapeutic monitoring (RTM) services, and care management services such as chronic care management (CCM), transitional care management (TCM), or behavioral health integration (BHI) services, if all the requirements to report each service are met. However, time spent furnishing CPM services cannot represent time spent for any other furnished and billed service.
- G3002 may be billed by an unlimited number of physicians or other qualified health care professionals for a beneficiary for a month, as medically necessary. G3003 may be billed as many times as applicable for a given beneficiary and month, as medically necessary, after G3002 has been billed. However, CMS will be monitoring utilization.
- CPM services are limited to office or other outpatient or domiciliary settings.