Complementary Pain Treatments: Back to Acupuncture
An estimated 80% of adults in the United States will experience back pain at some point in their lives. It is consistently ranked as one of the leading causes of visits to a primary care physician1 and costs the nation over $170 billion per year.2 As pain physicians, we are no strangers to low back pain. Although we are armed to alleviate back pain with an arsenal of remedies, it is not uncommon to feel powerless when many of the conventional therapies have failed to deliver sufficient relief.
There is no shortage of complementary and alternative therapies for chronic pain. In fact, many of these treatments are now considered mainstream. Over 40% of the United States adult population uses some sort of complementary or alternative medicine (CAM).3 The American Pain Society and the American College of Physicians have outlined a clinical practice guideline using systematic reviews and randomized controlled trials to address many of these CAM therapies and found fair evidence for the effectiveness of acupuncture for the treatment of chronic low back pain.4
Acupuncture is one of the oldest practices of Chinese medicine, with documented reports of its use dating back as early as 100 BC.5 The ancient therapy of acupuncture aims to reestablish harmony within the body by relieving blockages in qi, thought to be the body’s vital energy, which travels along pathways called meridians (Figure 1). These blockages can manifest as tenderness on palpation. Studies suggest that approximately 20%–70% of these tender areas, also sometimes referred to as “trigger points,” correspond to acupuncture points.6-7
There are many theories explaining the therapeutic mechanism of acupuncture. The neurohumoral hypothesis describes analgesia from acupuncture via stimulation of A-delta afferents, which induces a cascade of endorphins, enkephalins, monoamines, and other neurotransmitters in the central nervous system.8 Other theories include increase in nitric oxide synthase activity,9 activation of other descending inhibitory pain signals,10 changes in blood flow,11 and placebo effect.
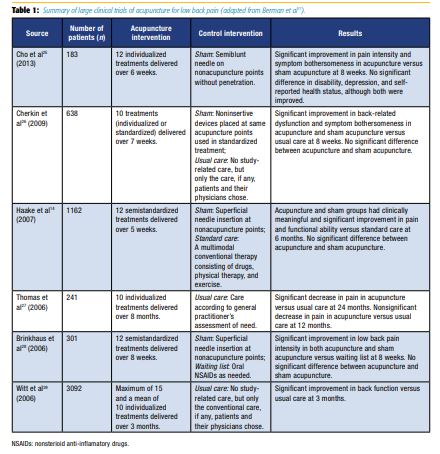
Systematic reviews and meta-analyses report conflicting results when comparing acupuncture versus sham acupuncture. A minority of the reviews concluded that there is limited evidence in acupuncture being more effective than no treatment for chronic pain. Low-quality trials were significantly associated with positive results.8 However, a more consistent theme across many of these reviews is the analgesic and functional benefit of either acupuncture or sham acupuncture when compared with conventional treatment, such as physical therapy, exercise, and medications (Table 1).12–15 One of the main challenges in designing high-quality randomized controlled trials is the use of sham acupuncture. It was once considered a placebo arm but likely has physiologic effects that result in significant analgesic benefit over true inert placebos. This was seen in animal studies that involved needling of nonacupuncture points resulting in an analgesic response.16 This suggests that many of the mechanisms by which acupuncture can reduce low back pain may be secondary to needle puncture itself, and not necessarily limited to acupoints.
Many trials show positive outcomes in patients receiving six or more treatments versus fewer than six.8 More recent studies recommend a minimum of 10–12 sessions to determine if there is therapeutic benefit. The reason may be coincidental, patients becoming more “invested” in treatments with increasing number of sessions, or possibly a cumulative effect. However, treatment should be discontinued if no benefit is seen after 10–12 sessions. With ongoing benefit, some may require maintenance treatments monthly or every few months.17
Acupuncture has undergone an evidence-based review from the Veterans Health Administration18 and is being incorporated in many Veterans Affairs (VA) Medical Centers across the country as part of the opioid safety initiative, in an attempt to decrease reliance on opioid pain medications for chronic pain. In the Atlanta VA Medical Center, veterans are regularly treated within the pain clinic by physicians with acupuncture certification, which has become a popular modality of treatment in high demand. Pain relief appears to be short-lived, but with regular weekly treatments over the course of 6–8 weeks, can decrease veterans’ need for pain medications and also improve function. These treatments must be maintained every few months after the initial 6- to 8-week period in order to provide continued benefit. It is unclear what the overall costs are to the system and whether the frequency of the visits outweighs the decreased reliance on medications and less invasive nature of this modality, but it demonstrates that acupuncture can improve pain and function with minimal risk to the patient.
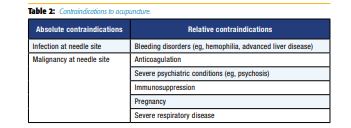
Absolute contraindications include infection or malignancy at the needle site. Relative contraindications include bleeding disorders (eg, hemophilia, advanced liver disease), patients on anticoagulant therapy, and severe psychiatric conditions (eg, psychosis). Although not a true contraindication, one should be cautious in pregnancy, owing to the possibility of inducing labor, and in severe respiratory disease owing to the possibility of pneumothorax (Table 2).19
Major adverse events due to acupuncture are extremely rare but can include pneumothoraces, infections, and acute hypertensive crises. There are five case reports that describe death after acupuncture from pneumothoraces.20 In a large study involving more than 2 million acupuncture treatment sessions, hematoma (6.1%) was the most common adverse event followed by pain at the needle site (1.7%).21
It has been suggested that a practitioner should consider referral to acupuncture for low back pain at the 4- to 6-week mark to be cost-effective.22 Approximately 90% of patients who present with acute low back pain have resolution of symptoms within 4–6 weeks with conservative therapy alone.2 Although research supports the effectiveness of acupuncture for acute low back pain,23 it may be more financially practical to use acupuncture beyond the acute phase. One study found that receiving acupuncture did not offset the use of other health care resources. Acupuncture was associated with increased primary care visits, specialist referrals, and physical therapy referrals.24
Acupuncture is a form of CAM that is relatively safe for the treatment of chronic low back pain. While studies report varying efficacy, most recent randomized controlled trials agree that there is at least modest analgesic benefit (either true or sham acupuncture) over a treatment regimen that does not use acupuncture. Acupuncture should be used in conjunction with a multimodal and multidisciplinary approach to chronic low back pain. Furthermore, it should not replace the traditional approach to chronic low back that may include a thorough clinical history and examination, necessary imaging, conventional therapies, and the exclusion of serious underlying medical conditions.
References
1. Centers for Disease Control, National Center for Health Statistics. Ambulatory health care data. Available at: http://www.cdc.gov/nchs/ahcd/. Accessed December 8, 2016.
2. Manchikanti L. Epidemiology of low back pain. Pain Physician 2000;3(2):167– 192.
3. Barrett B. Alternative, complementary, and conventional medicine: is integration upon us? J Altern Complement Med 2003;9:417–427.
4. Chou R, Huffman LH; American Pain Society; American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 2007;147(7):492–504.
5. Lu H. The Yellow Emperor’s Book of Acupuncture. Vancouver, Canada: Academy of Oriental Heritage; 1973.
6. Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain 1977;3(1):3–23.
7. Birch S. Trigger point: acupuncture point correlations revisited. J Altern Complement Med 2003;9(1):91–103.
8. Ezzo J, Berman B, Hadhazy VA, Jadad AR, Lao L, Singh BB. Is acupuncture effective for the treatment of chronic pain: a systematic review. Pain 2000;86(3):217–225.
9. Tsuchiya M, Sato EF, Inoue M, et al. Acupuncture enhances generation of nitric oxide and increases local circulation. Anesth Analg 2007;104:301–307.
10. Wu MT, Hsieh JC, Xiong J, et al. Central nervous pathway for acupuncture stimulation: localization of processing with functional MR imaging of the brain— preliminary experience. Radiology 1999;212:133–141.
11. Inoue M, Kitakoji H, Yano T, et al. Acupuncture treatment for low back pain and lower limb symptoms: the relation between acupuncture or electroacupuncture stimulation and sciatic nerve blood flow. Evid Based Complement Alternat Med 2008;5:133–143.
12. Vickers AJ, Linde K. Acupuncture for chronic pain. JAMA 2014;311(9):955–956.
13. Yuan J, Purepong N, Kerr DP, Park J, Bradbury I, McDonough S. Effectiveness of acupuncture for low back pain: a systematic review. Spine 2008;33:E887–E900.
14. Haake M, Muller HH, Schade-Brittinger C, et al. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallelgroup trial with 3 groups. Arch Intern Med 2007;167:1892–1898.
15. Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol 2006;164:487–496.
16. LeBars D, Villanueva L, Willer JC, Bouhassira D. Diffuse noxious inhibitory controls (DNIC) in animals and man. Acupunct Med 1991;9:47–56.
17. Berman BM, Langevin HM, Witt CM, Dubner R. Acupuncture for chronic low back pain. N Engl J Med 2010;363(5):454–461.
18. Hempel S, Taylor SL, Solloway MR, et al. Evidence Map of Acupuncture. Washington, DC: Department of Veterans Affairs; 2014.
19. Chung A, Bui L, Mills E. Adverse effects of acupuncture: which are clinically significant? Can Fam Physician 2003;49:985–989.
20. Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks: a review of reviews. Pain 2011;152(4):755–764.
21. Witt CM, Pach D, Brinkhaus B, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementarmed 2009;16:91–97.
22. Barrett B. Alternative, complementary, and conventional medicine: is integration upon us? J Altern Complement Med 2003;9:417–427.
23. Lee JH, Choi TY, Lee MS, Lee H, Shin BC, Lee H. Acupuncture for acute low back pain: a systematic review. Clin J Pain 2013;29(2):172–185.
24. Lewis K, Abdi S. Acupuncture for lower back pain: a review. Clin J Pain 2010;26(1):60–69.
25. Cho YJ, Song YK, Cha YY, et al. Acupuncture for chronic low back pain: a multicenter, randomized, patient-assessor blind, sham-controlled clinical trial. Spine (Phila Pa 1976). 2013;38(7):549–557.
26. Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med 2009;169(9):858–866.
27. Thomas KJ, MacPherson H, Thorpe L, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ 2006;333(7569):623.
28. Brinkhaus B, Witt CM, Jena S, et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med 2006;166(4):450–457.
29. Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol 2006;164(5):487–496.
Leave a commentOrder by
Newest on top Oldest on top