Minority Underrepresentation Is Growing in Medicine: Where Are We Today, and Where Will We Be Tomorrow?
Cite as: Estime SR, Reed A. Minority underrepresentation is growing in medicine: where are we today, and where will we be tomorrow? ASRA News 2021;46. https://doi.org/10.52211/asra080121.057.
Introduction
Improving how we treat chronic pain requires a physician workforce that is prepared to address the inequities in our healthcare system. This includes a workforce that reflects the diversity of patients they serve and a workforce that understands the factors that drive disparity in chronic pain. Health inequities have persisted long before the COVID-19 pandemic but are now on prominent display. The worsened outcomes with COVID-19 among the poor and minorities are similar in many ways to those suffering disproportionally from chronic pain in these same communities. Chronic pain is a disease not just a symptom of an injury or illness. This will require recruiting increasing the diversity in our workforce and recruiting those who are invested in the issues driving inequities in healthcare.
Is The Workforce Representative of Society?
The short answer is no.
The Association of American Medical Colleges (AAMC) maintains a comprehensive database on the physician workforce and its pipeline. They have also helped define what underrepresentation means for the medical community. Underrepresented minorities (URMs), which has since been updated to “underrepresented in medicine” (UiM), is a term used to describe underrepresented racial and ethnic groups in medicine. This has traditionally included Blacks/African Americans, Latinos, American Indians, Alaska Natives, Native Hawaiians, and other Pacific Islanders; however the AAMC acknowledges that defining these groups evolves with time and may depend on the population in question. Thus, schools, residencies and hospitals may define underrepresentation based on the demographics they serve rather than national demographics at large.
With that being said, it is helpful to understand the demographics of our workforce and the existing disparities within the United States. Based on the U.S. Census Bureau, people of Black and Latinx race make up 32% of the U.S. population. However just 11% of all physicians are of Black and Latinx race, including 10% of anesthesiologists and 12% of pain medicine doctors. (Figure 1) The disparity grows when considering full time academic physicians who are Black and Latinx as they make up just 6% of the workforce. (Figure 2)1
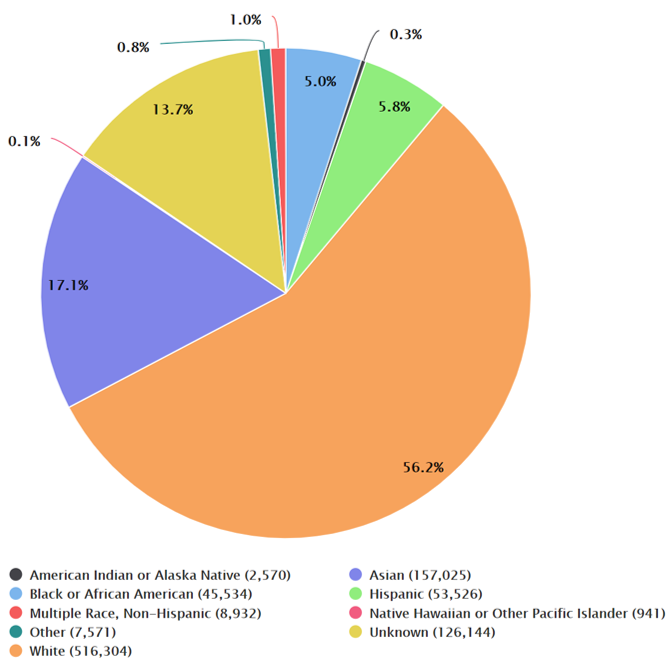
Figure 1: Percentage of Active Physicians by Race/Ethnicity as of July 1, 2019 (adapted from AAMC)
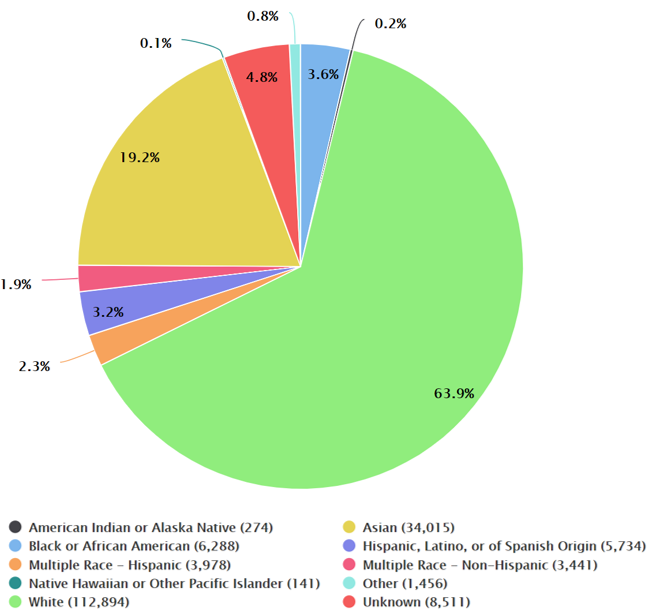
Figure 2: Full-time U.S. Medical School Faculty by Race/Ethnicity as of Dec. 31, 2018 (adapted from AAMC)
The lack of underrepresented physicians is not likely to go away anytime soon. While minorities are expected to comprise more than half of the U.S. population by 2045, underrepresented physicians are expected to remain a small fraction of physicians.2 To understand why, it is helpful to consider the current physician pipeline. Based on 2018-2019 academic year data aggregated by the AAMC, just 15% of those applying to medical school were Black or Latinx. The numbers are more dire for those that matriculate into medical school (13%) and go on to graduate (11.5%). (Figure 3)
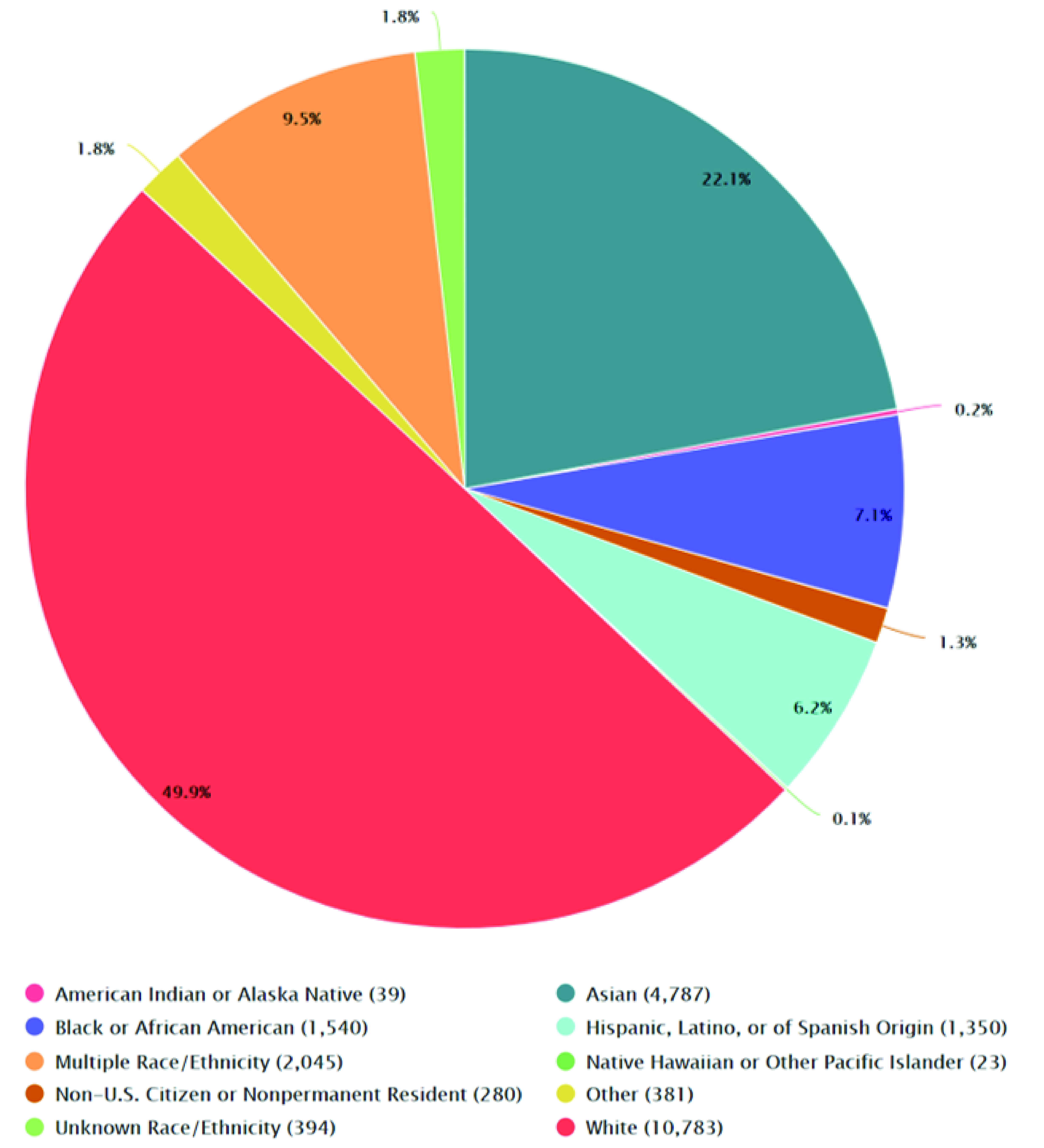
Figure 3: U.S. Medical School Matriculants by Race/Ethnicity, academic year 2018-19 (adapted from AAMC)
Several factors are partly responsible for this deteriorating—indeed broken—pipeline. Those underrepresented in medicine disproportionally incur higher premedical educational debts, have fewer accessible mentors, experience racism either overt or subtle, and suffer from the abolishment of policies like affirmative action that hinder the growth of future pipelines.
Why Does a Diverse Workforce Matter?
Medical students from underrepresented backgrounds are more likely to work in underserved areas with vulnerable populations – an effect that is independent of the student’s socioeconomic status. This can translate to better healthcare outcomes as a more diverse workforce improves patient satisfaction and health care delivery and increases financial performance.3,4 Racially diverse hospital systems have been shown to reduce major complications including death among minority patients, owing in part to higher cultural proficiencies among clinicians.5 Clinicians who understand their patients’ lived experiences, core values, and the circumstances that influence their health decisions allow for better care. For instance, studies have shown when Black patients are cared for by Black physicians, patients are more likely to opt in for testing, including diabetes screenings and cholesterol monitoring. There is a certain comfort level and trust that occurs when core values are shared.6 There is no more jarring example of this than a recent study that found the mortality rate of Black babies was reduced by about half when they were delivered by Black physicians.7
Understanding and empathy among clinicians is particularly important in pain management. Studies have shown that the treatment of pain vary among race, ethnicity, native language, and socioeconomic status.8 For instance, Black patients often receive less pain medication compared to their white counterparts.9 A workforce committed to providing clinical care, research, and education to address these gaps in care are needed now more than ever.
How Do We Craft the Workforce We Need?
Patients benefit when they are cared for by a diverse workforce, which is why initiatives that enhance the recruitment and development of underrepresented physicians are important. Commitment and investment are needed at both the institutional and local levels. At the institutional level, financial investments allow for resources and infrastructure development that can attract and develop talent. For example, Columbia University invested more than $100 million in a five-year program to increase the diversity of its faculty. This has helped bolster recruitment and has set a top-down tone that prioritizes workforce diversity.
An Effective Workforce Must Understand Determinants of Health
An effective workforce is more than just its diverse clinicians. It must be one that is better prepared to meet the complex needs of its patients. In an increasingly value-based healthcare environment, considering all the factors that influence health and exacerbate chronic pain is vital. The Social Determinants of Health framework is a model that considers many facets of one’s life including where one lives, works, plays and socializes. These often influence health to a greater degree than simply treating a complaint. Recruiting a workforce committed to solving chronic pain cannot be simply treating an injury with a procedure or through medication management. It must be done by partnering with entities that influence the multifaceted aspects of our patients lives that are pivotal to how they experience pain, seek treatment, and manage their conditions over the long term. This includes linking the pain experience with key outcomes beyond pain scores including the ability to return to work and school, the ability to engage support systems, and access to psychologic counseling among other treatment modalities. These need to be the attributes we look for in our students, trainees, and future colleagues as we continue to evolve our treatment of chronic pain that incorporates outcomes that truly matter for us, our patients and society.
Data collection within an organization can highlight gaps in an organization’s performance—information that can be used to develop specific plans to address inequities locally and institutionally. After surveying leadership within the American Society of Anesthesiologists (ASA), Toledo et al. identified deep gender and minority disparities at the leadership ranks that helped shed light and formed the basis for how ASA currently considers its leadership board.10,11 ASRA dedicated 2020 to recognizing the impact and achievements of women in regional anesthesia and pain medicine. The organization eliminated male-only panels at national meetings, acknowledged women for outstanding contributions to regional anesthesia and pain medicine, and worked to ensure women had key roles on national committees.12 While these efforts are truly commendable, we still have a way to go.
Having the right leadership within an organization pays dividends, particularly when it comes to hiring and recruitment. Among pain medicine fellowship programs, female program directors are more likely to attract and train female pain fellows.13 Constructing the right workforce takes an intentional commitment to diversity at the top to set the tone for the rest of the organization so that local leaders are empowered, understand the values of the organization, and can have the resources to ultimately attract the desired workforce.

Stephen R. Estime, MD, is an assistant professor of Anesthesiology at University of Chicago Medicine in Chicago, IL.

Ashley Reed, MD, is a pain medicine fellow, at University of Chicago Medicine in Chicago, IL.
References
- U.S. Census Bureau Data. U.S. Census Bureau. Published June 29, 2020. Accessed June 29, 2020. https://data.census.gov/cedsci/profile?q=United%20States&g=0100000US.
- Vespa J, Medina L, Armstrong D. Demographic turning points for the United States: population projections for 2020 to 2060. Published February 2020. Accessed June 29, 2020. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf.
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997–1004. https://doi.org/10.1001/archinte.159.9.997.
- Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc. 2019;111(4):383–92. https://doi.org/10.1016/j.jnma.2019.01.006.
- Okafor PN, Stobaugh DJ, van Ryn M, et al. African Americans have better outcomes for five common gastrointestinal diagnoses in hospitals with more racially diverse patients. Am J Gastroenterol. 2016;111(5):649–657. https://doi.org/10.1038/ajg.2016.64.
- Alsan M, Garrick O, Graziani G. Does diversity matter for health? experimental evidence from Oakland. Am Econ Rev. 2019;109(12):4071–111. https://doi.org/10.1257/aer.20181446.
- Greenwood BN, Hardeman RR, Huang L, Sojourner, A. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci U S A. 2020;117(35):21194-200. https://doi.org/10.1073/pnas.1913405117.
- Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med Malden Mass. 2012;13(2):150–174. https://doi.org/10.1111/j.1526-4637.2011.01310.x.
- Meghani SH, Polomano RC, Tait RC, et al. Advancing a national agenda to eliminate disparities in pain care: directions for health policy, education, practice, and research. Pain Med. 2012;13(1):5–28. https://doi.org/10.1111/j.1526-4637.2011.01289.x.
- Wong CA, Stock MC. The status of women in academic anesthesiology: a progress report. Anesth Analg. 2008;107(1):178–184. https://doi.org/10.1213/ane.0b013e318172fb5f.
- Toledo P, Duce L, Adams J, et al. Diversity in the American Society of Anesthesiologists leadership. Anesth Analg. 2017;124(5):1611–1616. https://doi.org/10.1213/ANE.0000000000001837.
- Viscusi E. President’s message: inclusivity, diversity, and ASRA’s celebration of the year of women in ASRA. ASRA News. Published November 2019. Accessed June 29, 2020. https://www.asra.com/asra-news/article/211/president-message-inclusivity-diversity
- Hagedorn JM, Moeschler S, Goree J, et al. Diversity and inclusion in pain medicine. Reg Anesth Pain Med. 2020;45(10):839. https://doi.org/10.1136/rapm-2020-101284.
Leave a commentOrder by
Newest on top Oldest on top