How I Do It
Learn from your colleagues. ASRA Pain Medicine members share how they perform common procedures and accomplish other tasks.
- Listed by publication date, most recent on top
How I Do It: Saphenous Nerve Block
The saphenous nerve can be elusive, and the multitude of approaches to blocking it only adds to the complexity of understanding and mastering its course. The nerve can be blocked essentially anywhere from the neuraxis and lumbar plexus to where it courses distally at the medial malleolus. When in doubt on a multiple-choice test, “all of the above” is likely correct. The suprainguinal fascia iliaca block will anesthetize the saphenous nerve: true. Local anesthetic administered in the distal femoral triangle blocks the saphenous nerve: true. The adductor canal (AC) block anesthetizes the saphenous nerve: true. A medial ring block in the supracondylar region blocks the saphenous nerve: true. However, studies describing the AC block, one of the most common approaches to saphenous nerve blockade, are frequently inconsistent and sometimes use incorrect terminology. Therefore, starting with a basic anatomy review is prudent.
The saphenous nerve can be elusive.
Saphenous Nerve Anatomy
The saphenous nerve (nerve roots L3–L4) is the femoral nerve’s largest cutaneous branch and originates from its posterior branch (Figure 1). The nerve runs lateral to the superficial femoral artery (SFA) in the AC, also known as Hunter’s canal or the subssartorial canal. The nerve is initially located lateral to the artery, then it crosses the SFA anteriorly and runs medially with the SFA until emerging from the AC with the saphenous branch of the descending genicular artery (SDGA). That small arterial branch can be useful in identifying the nerve distally in the thigh. After the nerve pierces the fascia lata between the gracilis and sartorius muscles, it divides into the infrapatellar and distal saphenous branches. The infrapatellar branch innervates the anterior inferior knee capsule and the skin below the patella. The distal saphenous branch courses laterally to the great saphenous vein in the lower leg, innervating the skin of the lower leg medially and sending off a branch into the medial ankle.
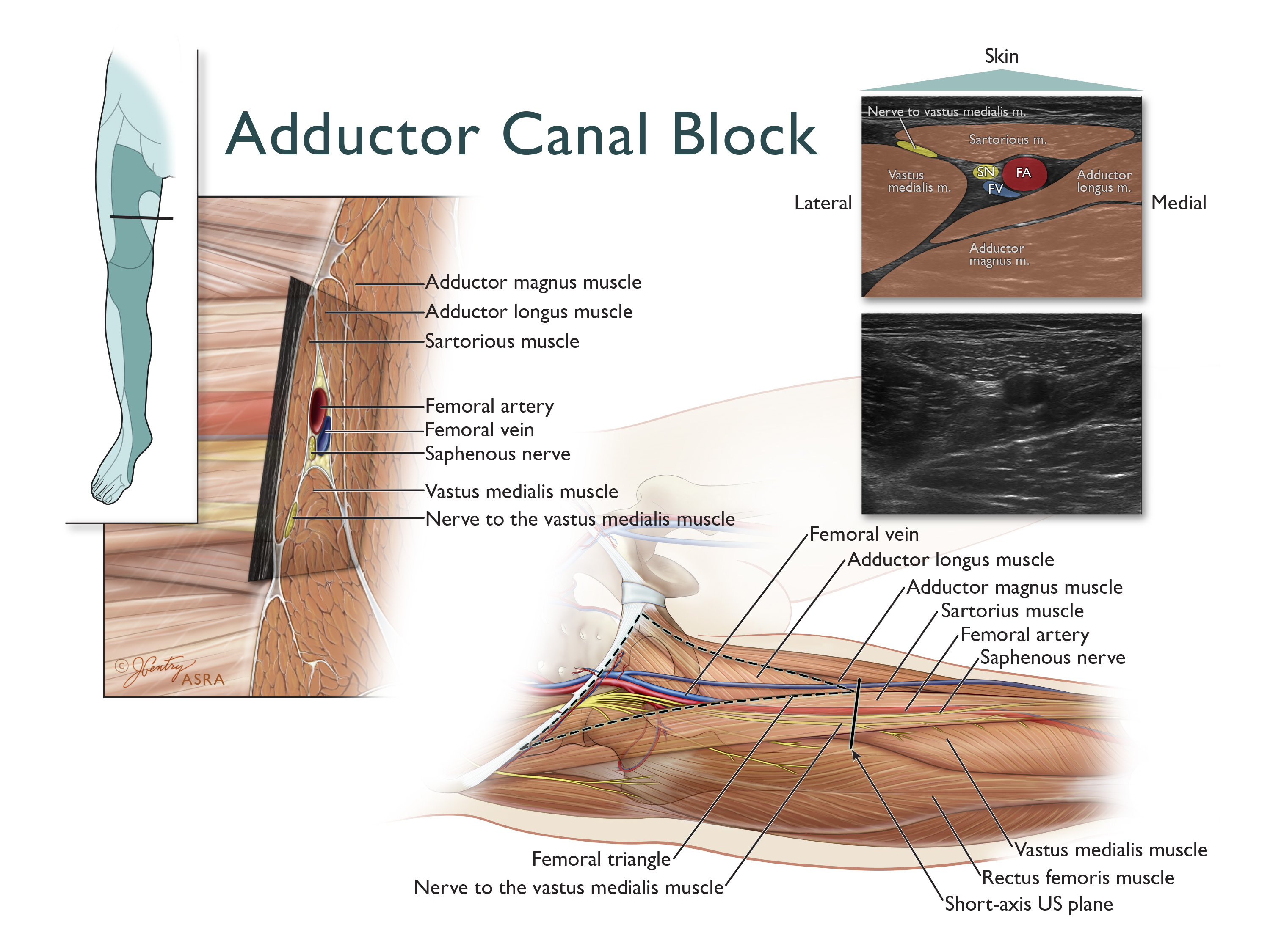
Figure 1: Femoral and saphenous nerve. Image from ASRA Image Gallery.
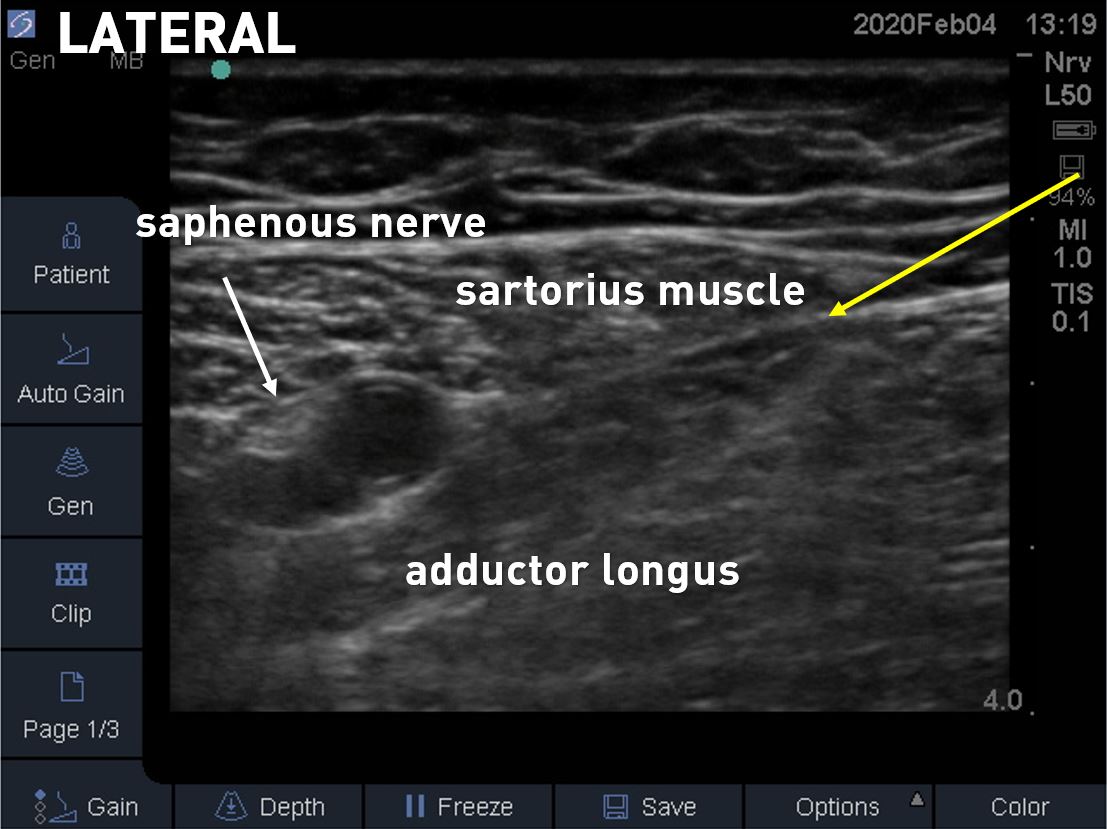
Figure 2: An ultrasound image of cross-section of the proximal adductor canal where the medial border of the sartorius intersects the medial border of the adductor longus (yellow arrow).
Adductor Canal Anatomy
John Hunter described the AC in the 18th century; it is typically defined by its surrounding structures. The canal is bordered laterally by the fascia of the vastus medialis, posteromedially by the fascia of the adductor longus and magnus, and anteriorly by the sartorius muscle (Figure 2). The true AC begins at the distal femoral triangle and ends at the adductor hiatus. The start is demarcated by the intersection of the medial border of the adductor longus with the medial border of the sartorius. The vastoadductor (or vasoadductor) membrane creates a roof for a portion of the aponeurotic tunnel; this covered portion is sometimes referred to as the “AC proper”[1] (Figure 3).
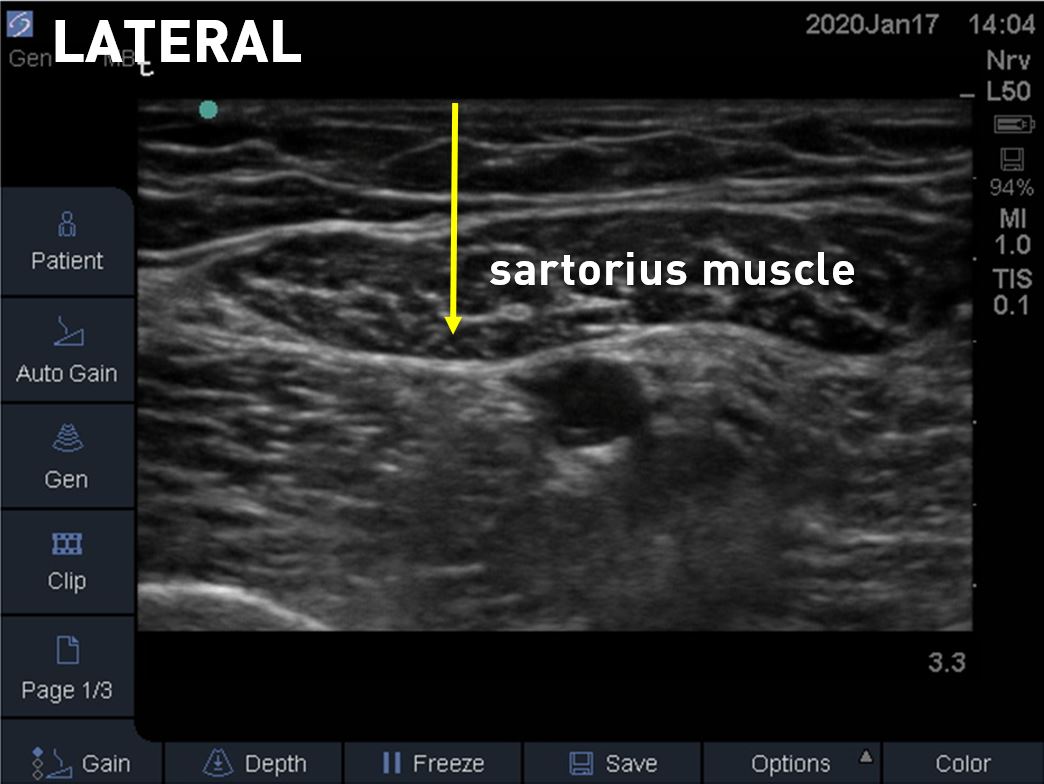
Figure 3: Ultrasound image of the adductor canal with the yellow arrow demarcating the vastoadductor membrane.
The AC’s components (Figure 4) vary anatomically, resulting in sometimes conflicting studies and sources. The saphenous nerve is consistently located in the AC and contributes to the patellar plexus and the subsartorial plexus. Although the medial femoral cutaneous nerve is noted as being in the canal in up to 61% of cadavers, other descriptions note that it is not contained within the AC.[2],[3] The anterior cutaneous branch of the obturator nerve is inconsistent in its location within the AC (21%), as is the superior medial genicular nerve.[2],[4] The genicular branch of the posterior division of the obturator nerve is more likely to be located in the distal AC.[4],[5] It is important to note that nerves located in the AC do not necessarily equate with nerves blocked by an ACB.
History of the Saphenous Nerve Block
Historically, saphenous nerve blocks were performed as cutaneous field blocks using an above-the-knee femoral paracondylar approach or below the knee using the greater saphenous vein as a landmark. In 1993, van der Wal et al demonstrated a more proximal method of blocking the saphenous nerve using a landmark-based, loss-of-resistance, transsartorial approach.[6]
The authors compared the three approaches for blocking the saphenous nerve and found the proximal transsartorial approach to be 80% successful with the more distal approaches less successful (65% for paracondylar and 40% for saphenous vein landmark).
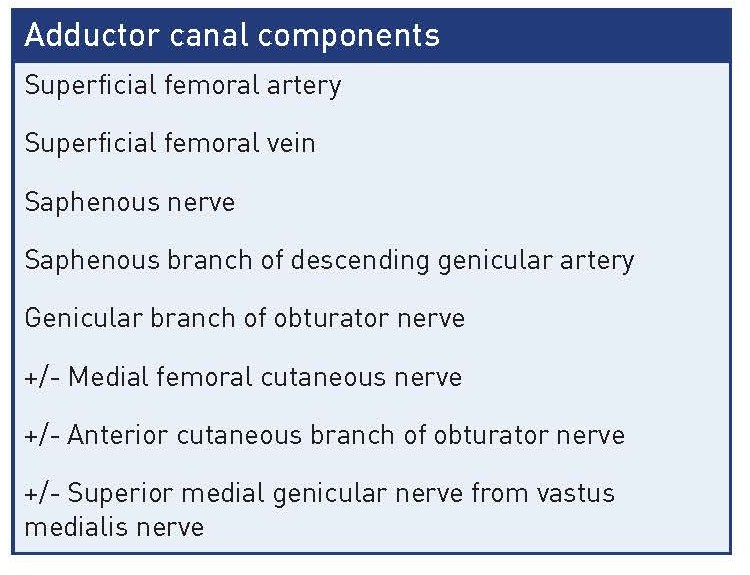
Figure 4: AC components.
In a cadaveric study, Horn and colleagues identified the saphenous nerve as it exited the adductor canal and demonstrated its consistent course with the saphenous branch of the SDGA.[7] Manickam et al then described ultrasound guidance for a saphenous nerve block more proximal in the adductor canal in a small descriptive study of patients undergoing foot and ankle surgery.[8]
In 2011, a study of continuous AC blocks for adjuvant postoperative analgesia in eight patients undergoing total knee arthroscopy was published that found the new block preserved quadriceps muscle strength and improved mobilization.[9] A study by Marian and colleagues demonstrated that an ultrasound-guided AC block approaching the saphenous nerve lateral to the SFA was more successful than the distal transsartorial saphenous nerve block approach using the SDGA as a landmark.[10]
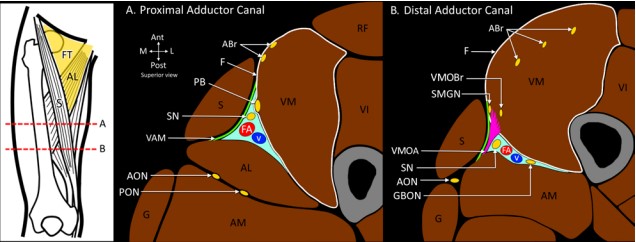
Figure 5: Schematic transverse sections through the proximal (A) and distal (B) adductor canal
A 22-person volunteer study by Wong et al helped to better define the AC and its relation to surface anatomy in healthy volunteers.[11] The authors demonstrated that the midpoint between the anterior superior iliac spine and patella is proximal to the start of the AC and is more consistently the location of the distal femoral triangle. This finding suggests that many of the studies performing AC blocks at the mid-thigh level targeting the anterolateral portion of the SFA are not actually performing AC blocks but rather distal femoral triangle blocks.
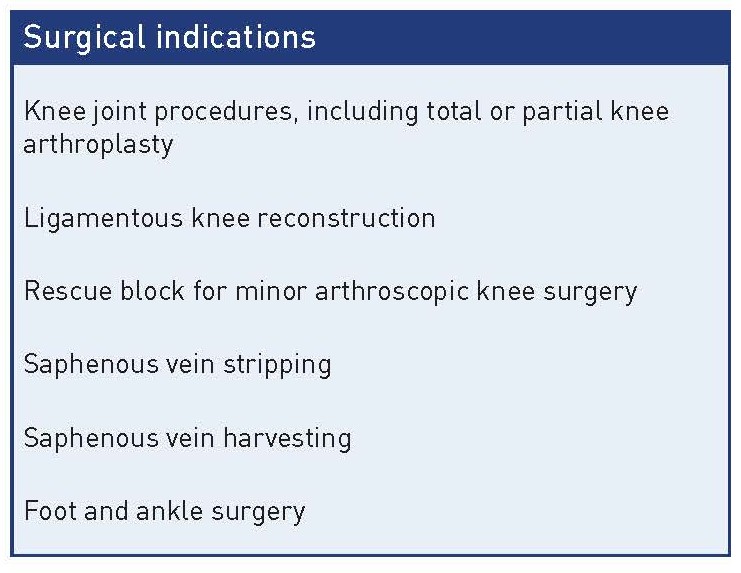 Figure 6: AC block surgical indications.
Figure 6: AC block surgical indications.
A more recent cadaver study helped differentiate distal femoral triangle blocks from proximal AC blocks and define the contents that ACs block. Using a 10 mL dye injection in a proximal AC block, the authors found spread to the saphenous nerve as well as the posteromedial branch of the nerve to vastus medialis (NVM).[12] Additionally, the superior medial genicular nerve branch from the NVM and the genicular branch of obturator nerve were stained with this small volume injected into the AC (Figure 5). This is significant because while not in the AC proper, the posteromedial branch of the NVM innervates the medial knee capsule. The authors concluded that both the distal femoral triangle block and the proximal AC may offer significant analgesia to the knee joint through blockade of the saphenous nerve, posteromedial branch of the NVM, superior medial genicular nerve, and genicular branch of obturator nerve, but the distal AC block was associated with greater motor sparing of other NVM branches.
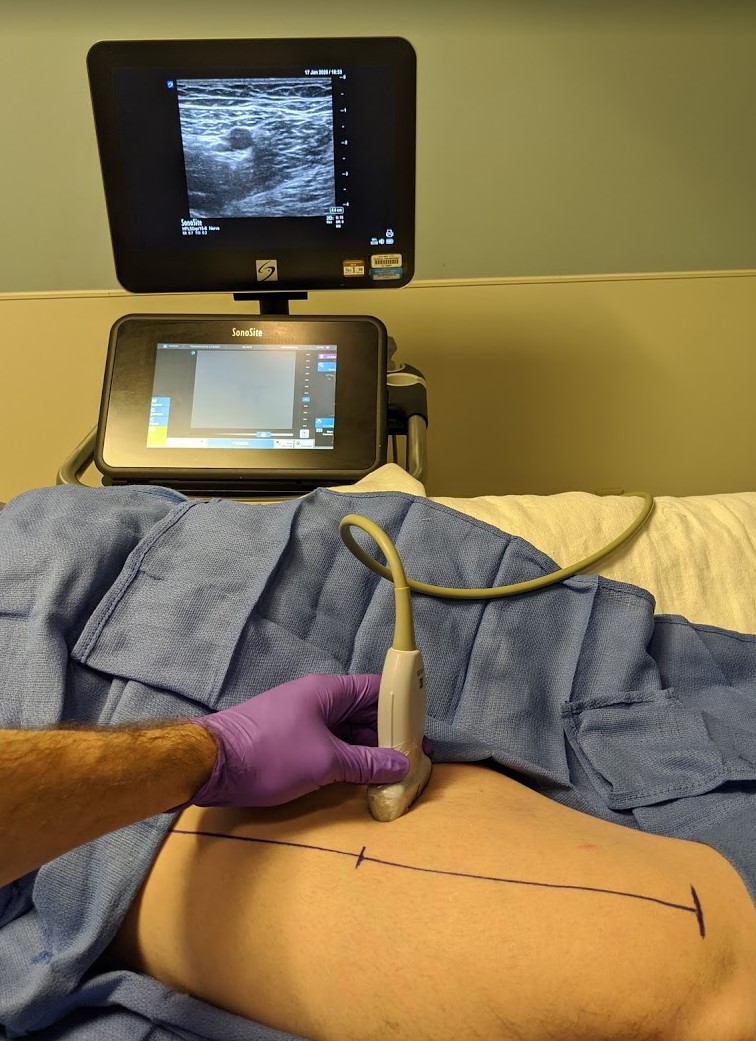
Figure 7: Mid-thigh imaging that demonstrates the distal femoral triangle.
The search to find the perfect motor-sparing analgesic block for early-ambulating total knee arthroscopy patients who are at risk for falls with or without a peripheral nerve block has instigated many studies comparing different approaches. In a meta-analysis, the AC block was shown to be noninferior to a femoral nerve block for outcomes of pain scores and opioid consumption with spared motor function. As noted, whether the blocks included in the studies were a true AC block or a distal femoral triangle block can be debated.[13] Nonetheless, both blocks offer motor-sparing advantages over a femoral nerve block with analgesia to some (of the many) nerves innervating the knee joint.
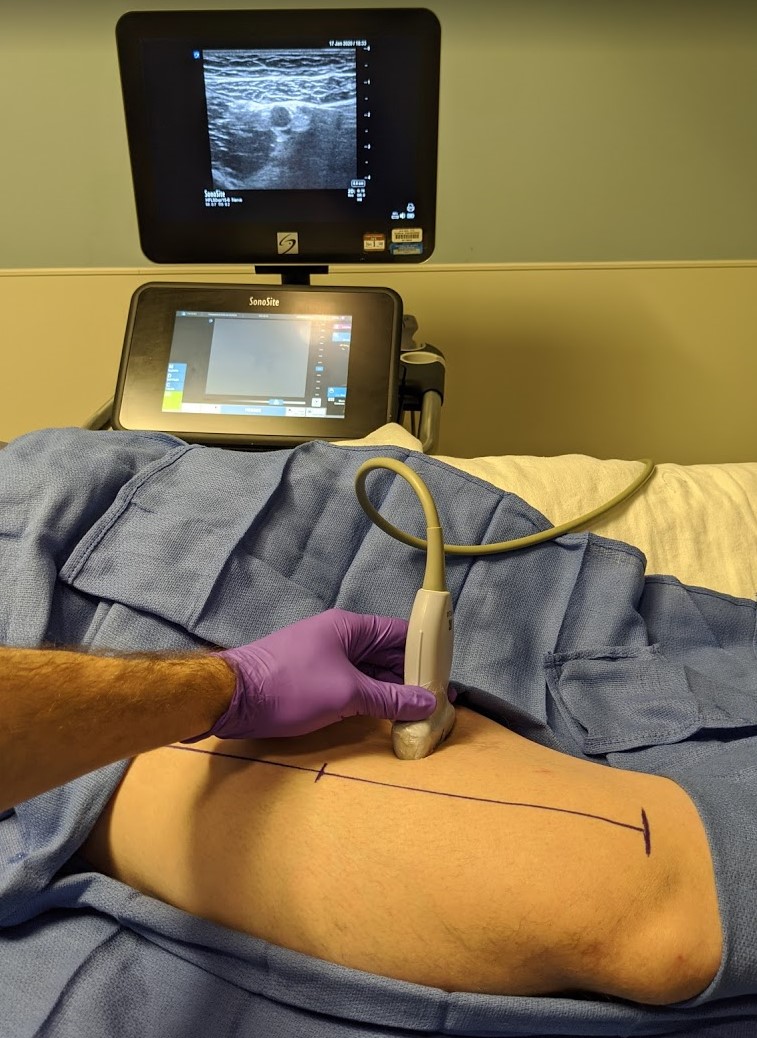
Figure 8: Ultrasound placement that demonstrates a proximal adductor canal block.
Indications
Figure 6 provides an overview of surgical indications for an AC block. For a procedure on the knee, a distal femoral triangle or proximal AC block is likely beneficial secondary to blockade of the posterior branch of NVM. For procedures below the knee, a more distal AC block may minimize the significant motor weakness that can accompany blockade of the proximal motor branches of the NVM.
Supplies
- High-frequency linear ultrasound probe
- 80 mm 22-gauge needle
- 10–15 mL of local anesthetic of choice
Positioning/Technique/Approach
Sometimes, the nerve is not visible or can be confused with the posteromedial branch of NVM. The needle approaches the nerve from a lateral to medial direction either in the fascial plane between the sartorius and vastus medialis muscle or by traversing the sartorius muscle (Figure 9). The injection must not only be subsartorial, but also in the aponeurotic plane that surrounds the nerve and vessel. If local anesthetic is injected into the AC proper, it should spread circumferentially around the artery and nerve as opposed to a more horizontal linear distribution under the sartorius muscle.Position the patient supine with the leg slightly externally rotated. Place the high-frequency ultrasound transducer over the anteromedial thigh, usually starting in the mid-thigh (Figure 7). Move the probe axially to find the superficial femoral artery, which should be located below the boat-shaped sartorius muscle. Move the probe caudally to identify the vastus medialis, adductor longus, and adductor magnus (Figure 8). The AC is defined where the medial border of vastus medialis intersects the medial border of adductor longus. The saphenous nerve should be hyperechoic and lateral to the SFA at this position.
A more distal approach can be used when the sensory block must be below the knee. Determine the true AC and follow the SDGA distally. The nerve should be located in close proximity, although it may not be visualized. Insert the needle in a lateral to medial direction, and inject 5–10 mL of local anesthetic to block the saphenous nerve.
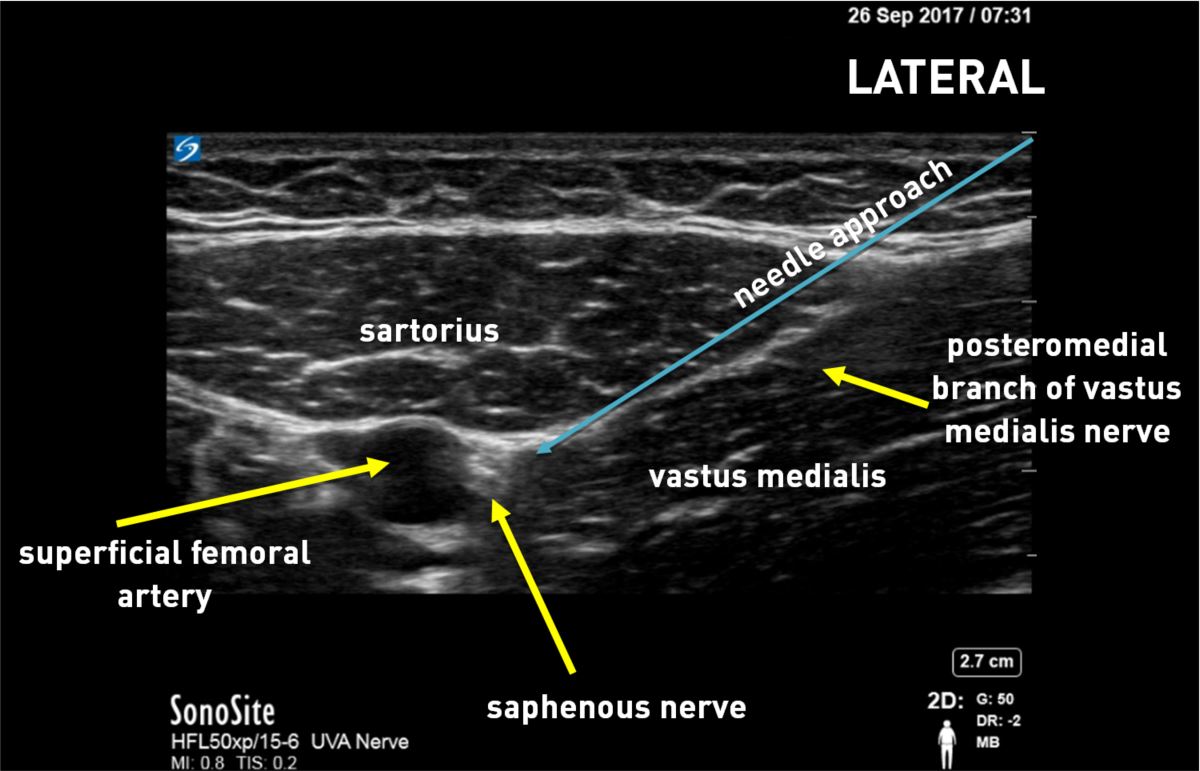
Figure 9: Ultrasound image of proximal adductor canal demonstrating the saphenous nerve.
Clinical Pearls
- The choice of a block site should involve thoughtful consideration of patient priorities, such as optimizing analgesia or avoiding motor blockade.
- Remember that a good choice for a procedure on the knee is a distal femoral triangle or proximal AC block, along with other supplemental blocks (obturator, sciatic, interspace between the popliteal artery and capsule of the posterior knee, intermediate femoral cutaneous nerve, lateral femoral cutaneous nerve) for more complete coverage of the knee.
- Low volumes of local anesthetic (10–15 mL) are sufficient to provide a successful block, although ideal dose studies are still needed.
- Larger volumes of local anesthetic may cause greater spread with the potential for increased motor block or more extensive sensory block.
- Incremental dosing and frequent aspiration are always prudent when performing an AC block because the target nerve is close to the superficial femoral artery and vein.
References
- Vora M, Nicholas T, Kassel C, Grant S. Adductor canal block for knee surgical procedures: review article. J Clin Anesth. 2016;35:295–303. https://doi.org/10.1016/j.jclinane.2016.08.021
- Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res. 1994;301:221–226. https://doi.org/10.1097/00003086-199404000-0003
- Bjorn S, Nielsen T, Moriggl B, Hoermann R, Bendtsen T. Anesthesia of the anterior femoral cutaneous nerves for total knee arthroplasty incision: randomized volunteer trial. Reg Anesth Pain Med. 2020;45(1):107–116. https://doi.org/10.1136/rapm-2019-100904
- Tran J, Peng PWH, Gofeld M, et al. Anatomical study of the innervation of posterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2019;44(2):234–238. https://doi.org/10.1136/rapm-2018-000015
- Özer H, Tekdemir I, Elhan A, Turanli S, Engebretsen L. A clinical case and anatomical study of the innervation supply of the vastus medialis muscle. Knee Surg Sports Traumatol Arthrosc. 2004;12(2):119–122. https://doi.org/10.1007/s00167-003-0382-7
- Van der Wal M, Lang SA, Yip RW. Transsartorial approach for saphenous nerve block. Can J Anaesth. 1993;40(6):542–546. https:// doi.org/10.1007/BF03009739
- Horn J, Pitsch T, Salinas F, Benninger B. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med. 2009;34(5):486–489. https://doi.org/10.1097/AAP.0b013e3181ae11af
- Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan, R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009;34(6):578– 580. https://doi.org/10.1097/aap.0b013e3181bfbf84
- Lund J, Jenstrup T, Jaeger P, Sorensen AM, Dahl JB. Continuous adductor canal-blockade for adjuvant post-operative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand. 2011;55(6):14–19. https://doi.org/10.1111/j.1399-6576.2010.02333.x
- Marian AA, Ranganath Y, Bayman EO, Senasu J, Brennan TJ. A comparison of 2 ultrasound-guided approaches to the saphenous nerve block: adductor canal versus distal transartorial: a prospective, randomized, blinded, noninferiority trial. Reg Anesth Pain Med. 2015;40(5):623–630. https://doi.org/10.1097/AAP.0000000000000277
- Wong WY, Bjorn S, Strid JM, Borglum J, Bendtsen TF. Defining the location of the adductor canal using ultrasound. Reg Anesth Pain Med. 2017;42(2):241–245. https://doi.org/10.1097/AAP.0000000000000539
- Tran J, Chan V, Peng P, Agur A. Evaluation of the proximal adductor canal block injectate spread: a cadaveric study. Reg Anesth Pain Med. 2020;45(1):124–130. https://doi.org/10.1136/rapm-2019-101091
- Wang D, Yang Y, Li Q, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. Sci Rep. 2017;7:40721. https://dx.doi. org/10.1038%2Fsrep40721
Leave a commentOrder by
Newest on top Oldest on top