How I Do It
Learn from your colleagues. ASRA Pain Medicine members share how they perform common procedures and accomplish other tasks.
- Listed by publication date, most recent on top
How I Do It: Managing an Obstetric Patient with Chronic Pain
Cite as: Zakowski M. How I do it: managing an obstetric patient with chronic pain. ASRA News. 2021;46. https://doi.org/10.52211/asra050121.034
A patient with chronic pain or history of opioid use can present with several anesthetic challenges; an obstetric patient is even more challenging. In 2017, 17% of Americans filled at least one opioid prescription.1 In the same year, maternal opioid use more than doubled to 8.2 per 1000 across the United States, with some states reporting numbers as high as 47 per 1000.2
It is important to distinguish between a patient with chronic pain without opioid tolerance, who will need increased analgesics, and a patient who is opioid-tolerant or on medication-assisted treatment, who will benefit more from regional blocks than additional opioid therapy.
Chronic pain is common during pregnancy. Approximately 38% of pregnant women report chronic pain or pain before pregnancy, whereas 55% have new-onset pain during pregnancy.3 In one study, pregnancy-related pelvic girdle pain and low back pain occurred in 45% and 25% of women, respectively.4 Chronic pain occurs across the full spectrum of socioeconomic classes, and many women are reluctant to take medications during pregnancy out of concern for fetal and/or neonatal effects.
Pregnant women with chronic pain should undergo a history review and physical examination that also screens for pain and substance use.5 The California Maternal Quality Care Collaborative recommends that standardized screening tools for substance use disorder should be used in all pregnant women to improve maternal and neonatal outcomes.6 Referral to a high-risk obstetric anesthesia clinic prior to delivery also allows physicians to design an individual anesthetic plan for labor analgesia, cesarean delivery, and the postpartum period for patients who need specialized pain management.
Chronic pain during pregnancy commonly involves pelvic girdle pain, back pain, and headaches. Diagnosing and understanding the underlying biomechanical issues (eg, herniated disc) are helpful. The source of chronic pain will likely increase the total anesthetic requirements for labor analgesia and the postpartum period. In particular, the concentration of the local anesthetic or opioid within the epidural solution may need to be increased. Many parturients with chronic pain will likely be on a combination of non-opioid and opioid-based analgesics. Some may be on medication-assisted treatment (MAT) for chronic opioid use disorder (OUD); it is generally recommended that these medications be continued through labor and delivery.6
Opioid tolerance develops very quickly by rapid desensitization of the mu-opioid receptor.7 In a randomized, double-blinded study, the administration of intrathecal (IT) fentanyl at the time of cesarean delivery increased postoperative morphine patient-controlled analgesia (PCA) consumption by 63%8 and increased pain scores post-cesarean section.9 These studies also confirmed what we observed in our clinical practice during the early 1990s, wherein patients who received 25 µg of IT fentanyl for labor analgesia developed tolerance after repeated doses via a microspinal IT catheter. Several years later, acute tolerance to IT fentanyl has been reported in the literature.10, 11 The use of IT fentanyl as an adjunct for acute pain may therefore be a mixed blessing.
Labor Analgesia
Neuraxial labor analgesia provides the highest quality, most reliable pain relief. The use of combined spinal epidural or dural puncture epidural (DPE) for a parturient with chronic pain is recommended. DPE allows partial distribution and increased absorption of epidural medications into the cerebrospinal fluid and spinal cord. Higher concentrations of local anesthetic within the epidural solution may be needed to treat patients who have acute labor pains and chronic back or pelvic girdle pains. The addition of neuraxial adjuncts can also be helpful. Examples of neuraxial adjunct medications include alpha adrenergic agonists, such as clonidine and dexmedetomidine, and epinephrine.
Moreover, it is important to understand the cause and location of the labor pain. For example, if the patient describes the pain as being above the anterior pelvis, this can indicate uterine pain. Lower back pain can be indicative of lumbo-sacral-plexus pressure from the fetal head or back pain stress. Lower pelvic pain can represent fetal head engagement, pelvic girdle pain, or sciatica. Understanding the source of the pain also helps determine the definitive management. In these scenarios, consider increasing the volume of the infused epidural solution or the concentration of the local anesthetic or opioid within the solution. Adding adjuncts such as clonidine, an alpha-adrenergic agonist with a recommended epidural dose of 1.2 µg/mL or IT dose of 50 µg, has been found to be beneficial.12 Epidural dexmedetomidine 0.5 µg/mL has also been used as an adjunct to ropivacaine infusion; it provides superior analgesia but with greater sedation compared with sufentanil.13 Including epinephrine in the epidural infusion may also provide analgesia via alpha-adrenergic agonism.14, 15
Systemic Supplementation/Augmentation
When neuraxial analgesia remains insufficient, consider adding inhaled nitrous oxide, remifentanil PCA, or a low-dose dexmedetomidine intravenous infusion.12 For intra-operative cesarean section discomfort and anxiety, low-dose propofol infusion (i.e., 25–50 µg/kg/min, 20–40 mg load) can be considered, with cautious monitoring and titration to keep the patient audibly conversing.
Cesarean Delivery
The intraoperative dosing requirements for local anesthetics for spinal dosing remains unchanged in patients with chronic pain or OUD. If the patient continues to complain of insufficient analgesia, consider discussing with the obstetrician if exteriorizing the uterus during closure can be avoided to help reduce pain and discomfort.16 Neuraxial opioid dosing may need to be increased and the use of additional adjuncts, such as 50–100 µg of IT clonidine, should be considered.12 Patients with chronic pain and opioid-tolerance may require an increase in the dose of neuraxial morphine. Using the epidural catheter to infuse a local anesthetic/opioid or give a repeat dose of epidural morphine for post-operative pain management is an option.17 Methadone may also be used for postoperative pain management in such patients.
General Anesthesia
If the patient requires general anesthesia due to emergent complications, has underlying coagulopathies, or refuses neuraxial anesthesia, regional blocks can be considered. Transversus abdominis plane (TAP) and quadratus lumborum blocks can provide some analgesic coverage of the abdominal wall. Some studies have shown that TAP blocks do not provide additional relief when used in addition to the triad of neuraxial morphine, acetaminophen, and non-steroidal anti-inflammatory drugs.16,18 The Society of Obstetric Anesthesia and Perinatology protocol for Enhanced Recovery after Cesarean Delivery provides recommendations for multimodal analgesic options.16
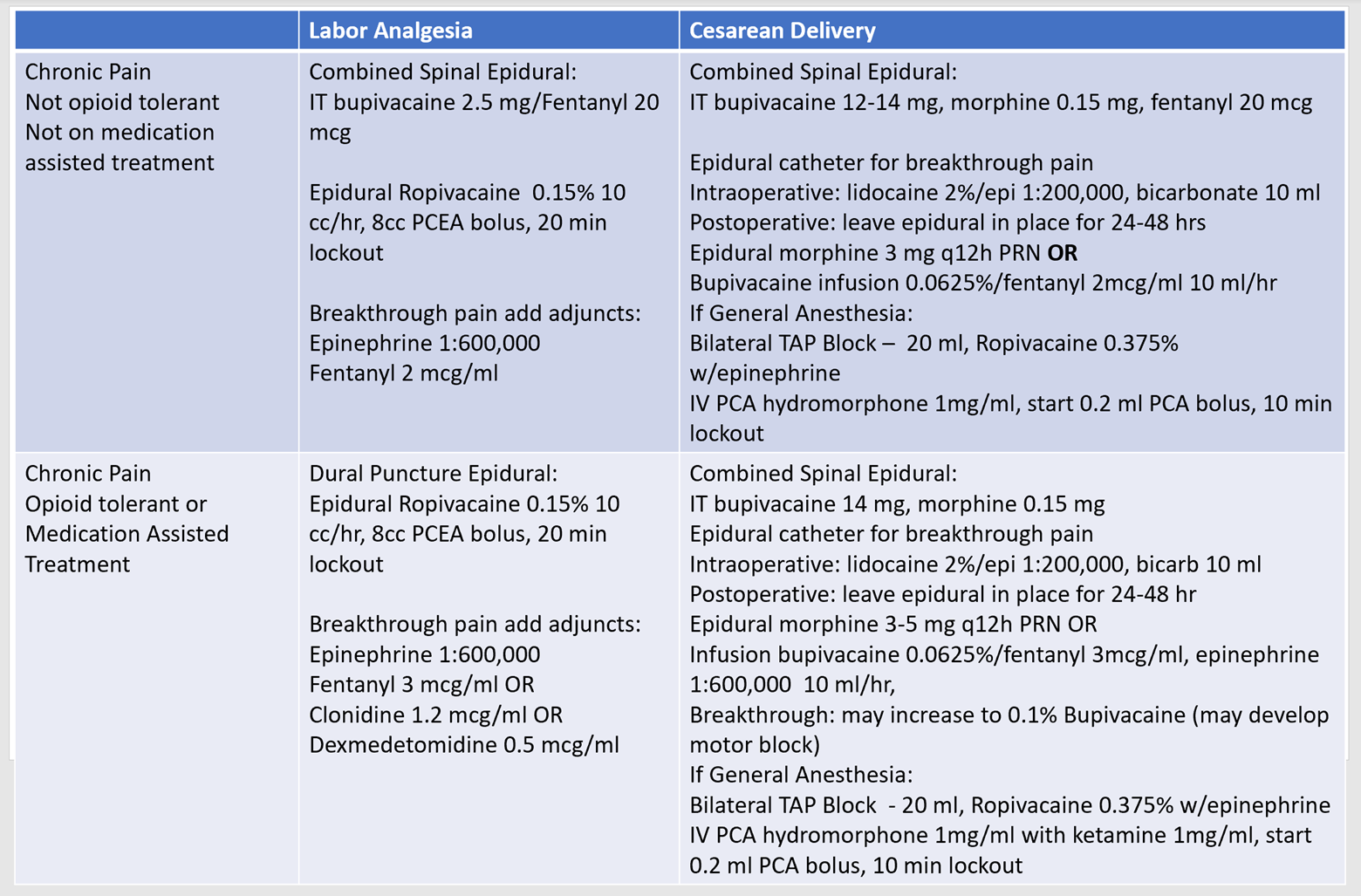
An individualized analgesic plan19 should be implemented for pregnant patients with chronic pain. It is important to distinguish between a patient with chronic pain without opioid tolerance, who will need increased analgesics, and a patient who is opioid-tolerant or on MAT, who will benefit more from regional blocks than additional opioid therapy. Baseline MAT therapy should also be continued in these patients. It has also been suggested that splitting the daily dose of methadone or buprenorphine into a twice or three-times-daily dosing schedule can improve pain control.12 A stepwise approach in managing pain for patients with chronic pain with and without opioid tolerance is illustrated in Table 1.
Table 1: Stepwise approach for labor analgesia and cesarean delivery in patients with chronic pain

Mark Zakowski, MD, FASA, is a professor of anesthesiology and program director for the obstetric anesthesiology fellowship at Cedars-Sinai Medical Center in Los Angeles, CA.
References
- Prescribing practices: changes in opioid prescribing practices. Centers for Disease Control. https://www.cdc.gov/drugoverdose/data/prescribing/prescribing-practices.html. Published August 13, 2019. Accessed April 1, 2021.
- Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA. J2021;325(2):146–155. https://doi.org/10.1001/jama.2020.24991.
- Munro A, George RB, Chorney J, Snelgrove-Clarke E, Rosen NO. Prevalence and predictors of chronic pain in pregnancy and postpartum. J Obstet Gynaecol Can. 2017;39(9):734–741. https://doi.org/10.1016/j.jogc.2017.01.026.
- Wu WH, Meijer OG, Uegaki K, et al. Pregnancy-related pelvic girdle pain (PPP), I: terminology, clinical presentation, and prevalence. Eur Spine J. 2004;13(7):575–89. https://doi.org/10.1007/s00586-003-0615-y.
- Committee opinion no. 722: marijuana use during pregnancy and lactation. Obstet Gynecol. 2017;130(4):e205–e209. https://doi.org/10.1097/AOG.0000000000002354.
- Mother & baby substance exposure toolkit. California Maternal Quality Care Collaborative. https://www.cmqcc.org/resources-toolkits/toolkits/mother-baby-substance-exposure-initiative-toolkit. Published 2020. Accessed December 1, 2020.
- Ok HG, Kim SY, Lee SJ, Kim TK, Huh BK, Kim KH. Can oliceridine (TRV130), an ideal novel micro receptor G protein pathway selective (micro-GPS) modulator, provide analgesia without opioid-related adverse reactions? Korean J Pain. 2018;31(2):73–79. https://doi.org/10.3344/kjp.2018.31.2.73.
- Cooper DW, Lindsay SL, Ryall DM, Kokri MS, Eldabe SS, Lear GA. Does intrathecal fentanyl produce acute cross-tolerance to i.v. morphine? Br J Anaesth. 1997;78(3):311–3. https://doi.org/10.1093/bja/78.3.311.
- Carvalho B, Drover DR, Ginosar Y, Cohen SE, Riley ET. Intrathecal fentanyl added to bupivacaine and morphine for cesarean delivery may induce a subtle acute opioid tolerance. Int J Obstet Anesth. 2012;21(1):29–34. https://doi.org/10.1016/j.ijoa.2011.09.002.
- Abboud TK, Zhu J, Sharp R, LaGrange C, Rosa C, Kassells B. The efficacy of intrathecal injection of sufentanil using a microspinal catheter for labor analgesia. Acta Anaesthesiol Scand. 1996;40(2):210–215. https://doi.org/10.1111/j.1399-6576.1996.tb04421.x.
- Kalaydjian A, Farah F, Cheng Y, Acquadro MA, Gerges FJ. Opioid induced hyperalgesia with intrathecal infusion of high-dose fentanyl. Pain Pract. 2019;19(2):222–223. https://doi.org/10.1111/papr.12726.
- Landau R. Post-cesarean delivery pain. Management of the opioid-dependent patient before, during and after cesarean delivery. Int J Obstet Anesth. 2019;39:105–116. https://doi.org/10.1016/j.ijoa.2019.01.011.
- Zhang T, Yu Y, Zhang W, Zhu J. Comparison of dexmedetomidine and sufentanil as adjuvants to local anesthetic for epidural labor analgesia: a randomized controlled trial. Drug Des Devel Ther. 2019;13:1171–1175. https://doi.org/10.2147/DDDT.S197431.
- Curatolo M, Petersen-Felix S, Arendt-Nielsen L, Zbinden AM. Epidural epinephrine and clonidine: segmental analgesia and effects on different pain modalities. Anesthesiology. 1997;87(4):785–794. https://doi.org/10.1097/00000542-199710000-00011.
- Niemi G, Breivik H. Epinephrine markedly improves thoracic epidural analgesia produced by a small-dose infusion of ropivacaine, fentanyl, and epinephrine after major thoracic or abdominal surgery: a randomized, double-blinded crossover study with and without epinephrine. Anesth Analg. 2002;94(6):1598–1605, table of contents. https://doi.org/10.1097/00000539-200206000-00044.
- Bollag L, Lim G, Sultan P, et al. Society for Obstetric Anesthesia and Perinatology: consensus statement and recommendations for enhanced recovery after cesarean. Anesth Analg. 2020;132(5):1362–1377. https://doi.org/10.1213/ANE.0000000000005257.
- Zakowski MI, Ramanathan S, Turndorf H. A two-dose epidural morphine regimen for cesarean section patients: therapeutic efficacy. Acta Anaesthesiol Scand. 1992;36(7):698–701. https://doi.org/10.1111/j.1399-6576.1992.tb03547.x.
- Patel K, Zakowski M. Enhanced recovery after cesarean: current and emerging trends. Curr Anesthesiol Rep. 2021:1–9. https://doi.org/10.1007/s40140-021-00442-9.
- Carvalho B, Habib AS. Personalized analgesic management for cesarean delivery. Int J Obstet Anesth. 2019;40:91–100. https://doi.org/10.1016/j.ijoa.2019.02.124.
Leave a commentOrder by
Newest on top Oldest on top