How I Do It
Learn from your colleagues. ASRA Pain Medicine members share how they perform common procedures and accomplish other tasks.
- Listed by publication date, most recent on top
How I Do It: Ultrasound-Guided Sciatic Nerve Block at the Popliteal Fossa
Cite as: Pai P, Jinadu S. How I do it: ultrasound-guided sciatic nerve block at the popliteal fossa. ASRA Pain Medicine News 2022;47. https://doi.org/10.52211/asra020122.003.
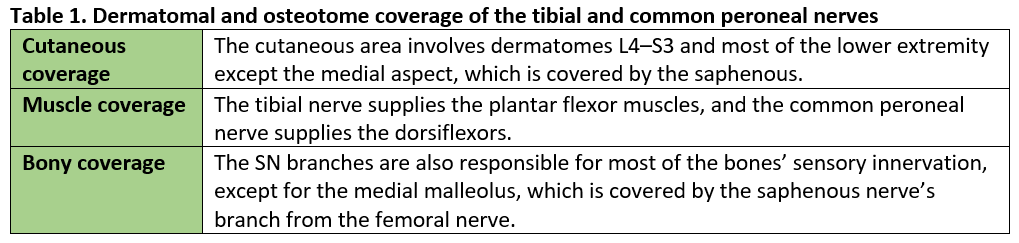
The sciatic nerve (SN) block at the popliteal fossa is useful for lower-extremity surgeries of the lower leg, ankle, and foot. The SN runs in the posterior thigh and bifurcates at the level of the popliteal fossa into the tibial nerve (TN) and common peroneal nerve (CPN), and the block targets the SN branches at the popliteal fossa. In addition to single-shot SN blocks, continuous blocks can be invaluable tools for surgeries where long-term analgesia is desired. The procedure presented in this article was first described by Singelyn et al, who in 1997 used a landmark technique with the aid of a peripheral neurostimulator.1
Anatomy
The sciatic nerve originates from the L4–S3 anterior rami of the sacral plexus and travels posteriorly through the thigh, where it bifurcates at the popliteal fossa to give rise to the TN medially and CPN laterally (see Figures 1 and 2).2 The exact level of bifurcation varies with patient anatomy, but placing the needle between 5 and 7 cm above the popliteal fossa is associated with a 95.22% success rate for SNB.3 The TN and CPN are encased in their individual epineuriums, both surrounded by a multilayered paraneural sheath,4 and the presence of the Compton-Cruveilhier septum creates two potential paraneural compartments in the sciatic nerve trunk (Figure 3).5 The fascial anatomy may have implications on the block’s onset, success, and safety.
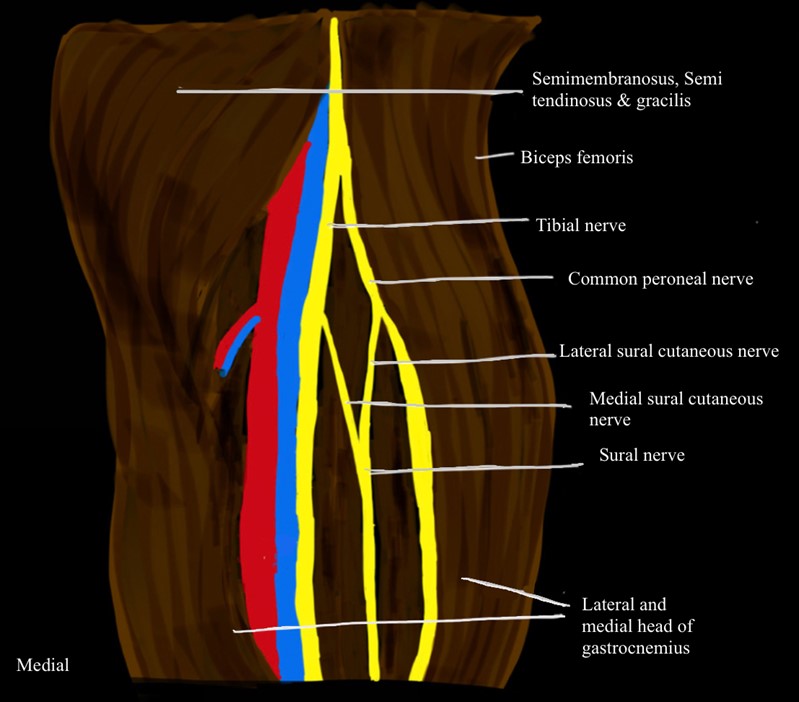
Figure 1. Schematic diagram illustrating sciatic nerve splitting into tibial nerve and common peroneal nerve with popliteal artery (red) and vein (blue) shown in the right popliteal fossa
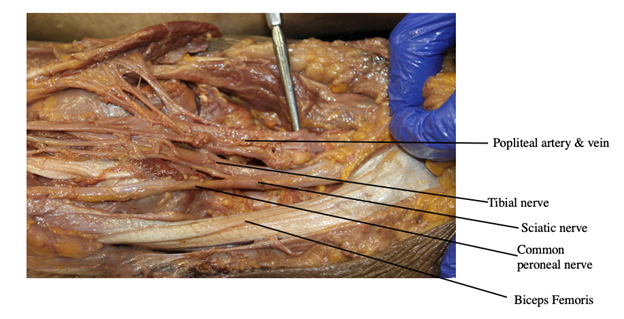
Figure 2. Cadaveric image showing the sciatic nerve at the bifurcation into common peroneal nerve laterally, tibial nerve medially, popliteal artery and vein in the right popliteal fossa, and biceps femoris
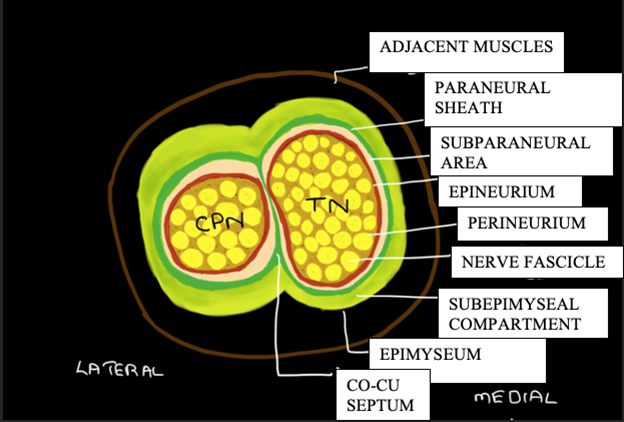
Figure 3. Schematic diagram illustrating the internal architecture of the sciatic nerve trunk splitting into tibial nerve (TN) and common peroneal nerve (CPN) within the fascial compartment in the midthigh, encompassed by the paraneural sheath where it merges with the Compton-Cruveilhier (Co-Cu) septum
Single-Shot Block
Although it can be approached with the patient in the supine, lateral, or prone position, we favor performing a single-shot block (SSB) in the supine position to minimize patient discomfort, especially for a patient with fractures in external fixators. For that approach, the patient is placed in the supine position and the legs elevated with folded blankets or an adjustable table.
Ultrasound guidance has been shown to improve the quality of SNB compared to a single-injection nerve-stimulator–guided block.6–9 Although our focus is description of the ultrasound-guided block, a nerve stimulator can be a helpful adjunct in patients with difficult sonographic anatomy and we will briefly discuss related findings.
Prepare the skin with chlorhexidine. Position the transducer in a transverse orientation at the popliteal fossa. At this level, identify the popliteal artery and confirm with color flow or power doppler. In patients with larger body mass index, increase the depth if needed to visualize the pulsating artery. Once the artery is visualized, locate the hyperechoic nerves superficially. At this level, it can be unclear if the TN and CPN have separated or still coalesced. Trace the sciatic nerve proximally to visualize where the TN and CPN eventually come together to form the sciatic nerve and separate distally, with the CPN travelling laterally and the TN staying medially. The optimal image is the configuration of the nerves just as they begin to separate, giving a peanut or figure 8 shape. Studies have shown that blocking the nerves in the fossa separately resulted in faster onset than a prebifurcation sciatic block (see Figure 4).10–12
Note the nerve’s distance from the skin on the ultrasound screen. Introduce the needle lateral to the probe in an in-plane approach, at the noted distance away from the probe. Needle entry should be above the biceps femoris tendon to prevent excessive patient discomfort. Direct the needle toward the perineural sheath and enter with the aim to deposit local anesthetic and observe its spread around the TN and CPN (see Figure 5).13 In our practice, we routinely use 20 mL of 0.5% or 0.25% ropivacaine or bupivacaine, which ensures the block’s success without toxicity in the average adult patient. Prior to injecting the local anesthetic, confirm negative aspiration. While injecting, it is important to watch for swelling of individual nerves, paresthesia, or high opening pressures, which may indicate intraneural injection. If that occurs, immediately stop the injection, withdraw the needle, and assess for nerve injury.
If using a neurostimulator, observe a plantar flexion response for the TN and dorsiflexion or eversion response for the CPN. Inject the local anesthetic at a current less than 0.5mA. If a current less than 0.2 mA elicits a motor response, reposition the needle. A plantar flexion of the foot is a better prediction of complete sensory blockade than dorsiflexion.14
Catheter Placement
We place the patient in the prone position, prep the skin, and apply a sterile drape (see Figure 6), then we identify the appropriate sonoanatomy as described before. Mohan et al. demonstrated superior analgesia when placing the catheter 5 cm proximal to the sciatic nerve bifurcation compared to at the bifurcation.15
For catheter placements, we prefer an out-of-plane approach in which we advance the needle through the paraneural sheath, outside the epineurium, in the middle of the two neural elements. This allows for adequate local anesthetic spread. Once the Tuohy needle is in a satisfactory position, we pass the catheter through the needle, remove the needle, and confirm proper positioning with saline or air. Take care to ensure negative aspiration. The block is often supplemented with general anesthesia or monitored anesthesia care depending on the type of surgery, incision location, and use of a tourniquet. Supplemental blocks such as an adductor canal block or femoral nerve block can ensure complete coverage of incision sites.
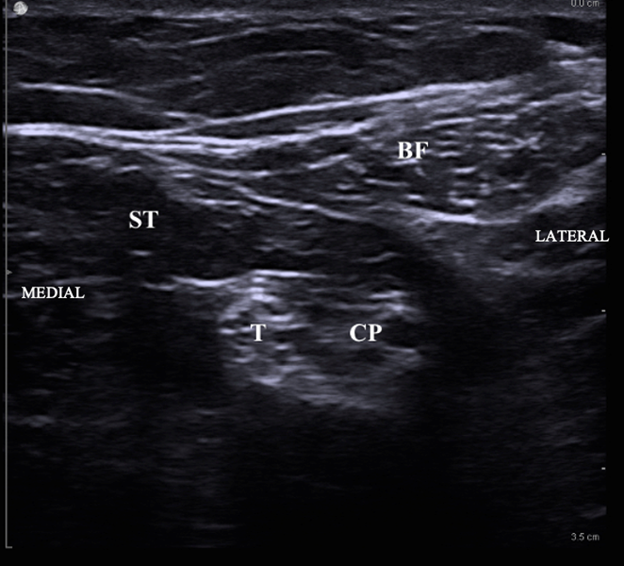
Figure 4. Ultrasound image of tibial nerve (T) and common peroneal nerve (CP) with good local spread seen circumferentially around the nerves
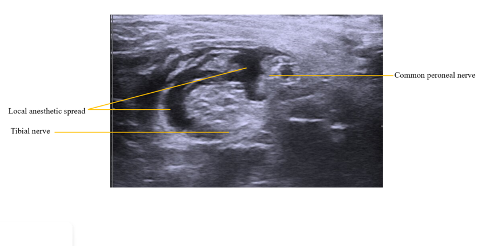
Figure 5. Local anesthetic seen circumferentially around tibial and common peroneal nerve with the surrounding muscular structure biceps femoris and semitendinosus

Figure 6. Patient in prone position for the placement of a sciatic nerve block at the popliteal fossa
Common Questions About SSBs
What is the ideal volume of local anesthetic? Jeong et al showed that the minimum effective volume (MEV) of 0.5% ropivacaine for single-injection, ultrasound-guided SNBs to be 6 mL and 16 mL for ED50 and ED95, respectively,16 which was confirmed in a study that showed that the MEV of local anesthetic was less than 7 mL.17 Chen et al showed a significant correlation between the MEV and cross-sectional area of the sciatic nerve and found the MEV of 1.5% lidocaine to be 7–15 mL.18 We routinely use 20 mL of 0.5% or 0.25% ropivacaine or bupivacaine, which ensures the block’s success without toxicity in the average adult patient.
What is the optimal location for the injection? Studies have shown that a subparaneural injection has more advantages than an extraparaneural injecton.19–21 Capelleri et al stated that a subepineural (intraneural) injection resulted in significantly faster onset time than a paraneural injection without any reported clinical neurologic complications;22 however, use of ultrasound to perform a subparaneural injection while avoiding a subepineurial injection may better prevent neurologic damage.23 Furthermore, Perlas et al confirmed that SNB through the common paraneural sheath is a simple, safe, and effective block that respects the integrity of the epineurium and intraneural structures.24 When comparing circumferential and noncircumferential injections, the time to achieve a sensory block is earlier with circumferential injections but the time to achieve a motor block is the same for both methods.25
Adjuvants
Patients undergoing foot and ankle surgery are offered a popliteal catheter depending on their preference and type of surgery. Some practitioners choose to add perineural dexamethasone to the local anesthetic in patients who refuse a catheter or lack proper social support to use a home pump. Adjuvants such as buprenorphine, nalbuphine, clonidine, dexmedetomidine, and magnesium, although promising for prolonging SSBs, are not routinely used at our institution.26–29
Complications
The main adverse events with a SNB in the popliteal fossa are bleeding, infection, local anesthetic toxicity, pain at needle site, and neuropathic complications. Park et al found a 2.7% incidence of transient neurologic complications from SNB.30 In another study of 855 patients, the authors reported a 10.1% incidence of short-term neuropathic complications after SNB and a 4.3% incidence of long-term complications31. Other studies have shown close to 0% complication rate.32
Conclusion
The popliteal nerve block is a useful analgesic modality for patients undergoing lower-extremity surgery. With the use of an ultrasound and an understanding of anatomy, appropriate local anesthetic choice, and proper technique, it can be done safely to provide reliable pain control.
The authors would like to thank Drs. Ali Shariat, Usama Siddiqui, and Janet Hong for their assistance with the images for the article.

Poonam Pai B.H., MD, MS, is an assistant professor and associate program director of the regional anesthesia and acute pain medicine fellowship program in the Icahn School of Medicine at Mount Sinai West and Morningside Hospitals in New York, NY.

Samiat Jinadu, MD, is an assistant professor in anesthesia and perioperative medicine at Oregon Health and Science University in Portland.
References
- Singelyn FJ, Aye F, Gouverneur JM. Continuous popliteal sciatic nerve block: an original technique to provide postoperative analgesia after foot surgery. Anesth Analg. 1997;84(2):383–6. https://doi.org/10.1097/00000539-199702000-00027
- Hansen E, Eshelman MR, Cracchiolo A 3rd. Popliteal fossa neural blockade as the sole anesthetic technique for outpatient foot and ankle surgery. Foot Ankle Int. 2000;21(1):38–44. https://doi.org/10.1177/107110070002100107
- Barbosa FT, Barbosa TR, da Cunha RM, Rodrigues AK, Ramos FW, de Sousa-Rodrigues CF. Anatomical basis for sciatic nerve block at the knee level. Braz J Anesthesiol. 2015;65(3):177–9. https://doi.org/10.1016/j.bjane.2014.03.010
- Andersen HL, Andersen SL, Tranum-Jensen J. Injection inside the paraneural sheath of the sciatic nerve: direct comparison among ultrasound imaging, macroscopic anatomy, and histologic analysis. Reg Anesth Pain Med. 2012;37(4):410–4. https://doi.org/10.1097/aap.0b013e31825145f3
- Karmakar MK, Reina MA, Sivakumar RK, Areeruk P, Pakpirom J, Sala-Blanch X. Ultrasound-guided subparaneural popliteal sciatic nerve block: there is more to it than meets the eyes. Reg Anesth Pain Med. 2021;46(3):268–75. https://doi.org/10.1136/rapm-2020-101709
- Perlas A, Brull R, Chan VW, McCartney CJ, Nuica A, Abbas S. Ultrasound guidance improves the success of sciatic nerve block at the popliteal fossa. Reg Anesth Pain Med. 2008;33(3):259–65. https://doi.org/10.1016/j.rapm.2007.10.010
- Sala-Blanch X, de Riva N, Carrera A, López AM, Prats A, Hadzic A. Ultrasound-guided popliteal sciatic block with a single injection at the sciatic division results in faster block onset than the classical nerve stimulator technique. Anesth Analg. 2012;114(5):1121–7. https://doi.org/10.1213/ANE.0b013e318248e1b3
- Danelli G, Fanelli A, Ghisi D, et al. Ultrasound vs nerve stimulation multiple injection technique for posterior popliteal sciatic nerve block. Anaesthesia. 2009;64(6):638–42. https://doi.org/10.1111/j.1365-2044.2009.05915.x
- van Geffen GJ, van den Broek E, Braak GJ, Giele JL, Gielen MJ, Scheffer GJ. A prospective randomised controlled trial of ultrasound guided versus nerve stimulation guided distal sciatic nerve block at the popliteal fossa. Anaesth Intensive Care. 2009;37(1):32–7. https://doi.org/10.1177/0310057X0903700115
- Buys MJ, Arndt CD, Vagh F, Hoard A, Gerstein N. Ultrasound-guided sciatic nerve block in the popliteal fossa using a lateral approach: onset time comparing separate tibial and common peroneal nerve injections versus injecting proximal to the bifurcation. Anesth Analg. 2010;110(2):635–7. https://doi.org/10.1213/ane.0b013e3181c88f27
- Eldegwy MH, Ibrahim SM, Hanora S, Elkarta E, Elsily AS. Ultrasound-guided sciatic popliteal nerve block: a comparison of separate tibial and common peroneal nerve injections versus injecting proximal to the bifurcation. Middle East J Anaesthesiol. 2015;23(2):171–6. https://pubmed.ncbi.nlm.nih.gov/26442393
- Prasad A, Perlas A, Ramlogan R, Brull R, Chan V. Ultrasound-guided popliteal block distal to sciatic nerve bifurcation shortens onset time: a prospective randomized double-blind study. Reg Anesth Pain Med. 2010;35(3):267–71. https://doi.org/10.1097/aap.0b013e3181df2527
- Brull R, Macfarlane AJ, Parrington SJ, Koshkin A, Chan VW. Is circumferential injection advantageous for ultrasound-guided popliteal sciatic nerve block? A proof-of-concept study. Reg Anesth Pain Med. 2011;36(3):266–70. https://doi.org/10.1097/aap.0b013e318217a6a1
- Taboada Muñiz M, álvarez J, Cortés J, Rodrguez J, Atanassoff PG. Lateral approach to the sciatic nerve block in the popliteal fossa: correlation between evoked motor response and sensory block. Reg Anesth Pain Med. 2003;28(5):450–5. https://doi.org/10.1016/j.rapm.2003.08.007
- Monahan AM, Madison SJ, Loland VJ, et al. Continuous popliteal sciatic blocks: does varying perineural catheter location relative to the sciatic bifurcation influence block effects? A dual-center, randomized, subject-masked, controlled clinical trial. Anesth Analg. 2016;122(5):1689–95. https://doi.org/10.1213/ane.0000000000001211
- Jeong JS, Shim JC, Jeong MA, Lee BC, Sung IH. Minimum effective anaesthetic volume of 0.5% ropivacaine for ultrasound-guided popliteal sciatic nerve block in patients undergoing foot and ankle surgery: determination of ED50 and ED95. Anaesth Intensive Care. 2015;43(1):92–7. https://doi.org/10.1177/0310057x1504300114
- Sala-Blanch X, Franco J, Bergé R, Marín R, López AM, Agustí M. 3D ultrasound estimation of the effective volume for popliteal block at the level of division. Rev Esp Anestesiol Reanim. 2017;64(3):125–30. https://doi.org/10.1016/j.redar.2016.08.004
- Chen X, Ling D, Cao J, et al. Factors associated with minimum effective volume of lidocaine 1.5% for sciatic nerve blocks. Clin J Pain. 2020;36(4):296–301. https://doi.org/10.1097/ajp.0000000000000799
- Luo J, Cai G, Ling D, et al. Mean effective volume of local anesthetics by nerve conduction technique. Ann Transl Med. 2020;8(5):174. https://doi.org/10.21037/atm.2020.01.96
- Lopez AM, Sala-Blanch X, Castillo R, Hadzic A. Ultrasound guided injection inside the common sheath of the sciatic nerve at division level has a higher success rate than an injection outside the sheath. Rev Esp Anestesiol Reanim. 2014;61(6):304–10. https://doi.org/10.1016/j.redar.2013.11.018
- Choquet O, Noble GB, Abbal B, Morau D, Pharm SB, Capdevila X. Subparaneural versus circumferential extraneural injection at the bifurcation level in ultrasound-guided popliteal sciatic nerve blocks. A prospective, randomized, double-blind study. Reg Anesth Pain Med. 2014; 39:306–11. https://doi.org/10.1097/aap.0000000000000095
- Cappelleri G, Cedrati VL, Fedele LL, et al. Effects of the intraneural and subparaneural ultrasound-guided popliteal sciatic nerve block: a prospective, randomized, double-blind clinical and electrophysiological comparison. Reg Anesth Pain Med. 2016;41(4):430–7. https://doi.org/10.1097/AAP.0000000000000413
- Lai YH, Rosenblatt MA. Ultrasound-guided popliteal intraneural approach: comment. Anesthesiology. 2019;130(6):1083. https://doi.org/10.1097/ALN.0000000000002717
- Perlas A, Wong P, Abdallah F, Hazrati LN, Tse C, Chan V. Ultrasound-guided popliteal block through a common paraneural sheath versus conventional injection: a prospective, randomized, double-blind study. Reg Anesth Pain Med. 2013;38:218–25. https://doi.org/10.1097/aap.0b013e31828db12f
- Brull R, Macfarlane AJ, Parrington SJ, Koshkin A, Chan VW. Is circumferential injection advantageous for ultrasound-guided popliteal sciatic nerve block? A proof-of-concept study. Reg Anesth Pain Med. 2011;36(3):266–70. https://doi.org/10.1097/aap.0b013e318217a6a1
- Vermeylen K, De Puydt J, Engelen S, et al. A double-blind randomized controlled trial comparing dexamethasone and clonidine as adjuvants to a ropivacaine sciatic popliteal block for foot surgery. Local Reg Anesth. 2016;9:17–24. https://doi.org/10.2147/lra.s96073
- Prajwal V, Preethi N, Usha N, Balakrishna N, Akash M. Effect of nalbuphine as adjuvant to bupivacaine for ultrasound-guided popliteal nerve block: a prospective randomised comparative clinical study. Indian J Anaesth. 2020;7(3):664–70. https://doi.org/10.21088/ijaa.2349.8471.7320.2
- Ahuja V, Thapa D, Chander A, Gombar S, Gupta R, Gupta S. Role of dexmedetomidine as adjuvant in postoperative sciatic popliteal and adductor canal analgesia in trauma patients: a randomized controlled trial. Korean J Pain. 2020;33(2):166–75. https://dx.doi.org/10.3344%2Fkjp.2020.33.2.166
- Noori N, Anand K, Pfeffer G, Thordarson D. Dexamethasone addition to popliteal nerve blocks: effects on duration of analgesia and incidence of postoperative nerve complication. Foot Ankle Spec. 2021;14(1):39–45. https://doi.org/10.1177/1938640019897224
- Park YU, Cho JH, Lee DH, Choi WS, Lee HD, Kim KS. Complications after multiple-site peripheral nerve blocks for foot and ankle surgery compared with popliteal sciatic nerve block alone. Foot Ankle Int. 2018;39(6):731–5. https://doi.org/10.1177/1071100717753954
- Lauf JA, Huggins P, Long J, et al. Regional nerve block complication analysis following peripheral nerve block during foot and ankle surgical procedures. Cureus. 2020;12(7):e9434. https://doi.org/10.7759/cureus.9434
- Provenzano DA, Viscusi ER, Adams Jr SB, Kerner MD, Torjman MC, Abidi NA. Safety and efficacy of the popliteal fossa nerve block when utilized for foot and ankle surgery. Foot Ankle Int. 2002; 23:394–9. https://doi.org/10.1177/107110070202300504
Leave a commentOrder by
Newest on top Oldest on top