How I Do It
Learn from your colleagues. ASRA Pain Medicine members share how they perform common procedures and accomplish other tasks.
- Listed by publication date, most recent on top
How I Do It: Discontinuation of Opioid Prescription
Cite as: Potru S, Nelson A. How I do it: discontinuation of opioid prescription. ASRA Pain Medicine News 2023;48. https://doi.org/10.52211/asra110123.005.
Introduction
Any clinician who prescribes opioids on an outpatient basis is familiar with the dreaded opioid discontinuation discussion. Although primary prevention in the perioperative space (ie, decreasing exposure to opioids) is important, the secondary prevention and tertiary prevention that is provided in outpatient primary care and pain management clinics is also paramount in monitoring patients for signs and symptoms of opioid use disorder (OUD) and discontinuing opioids if/when necessary. Although recreational opioid use has higher prevalence in younger populations, OUD is on the rise among the elderly patient population.1 Of note, stigma is still present when discussing OUD or substance use disorders (SUD), and clinicians should refrain from using the term “addiction,” even if the patient uses this language.2
Scenario 1: Patient Meets Criteria for SUD
Step 1: Determining presence of SUD
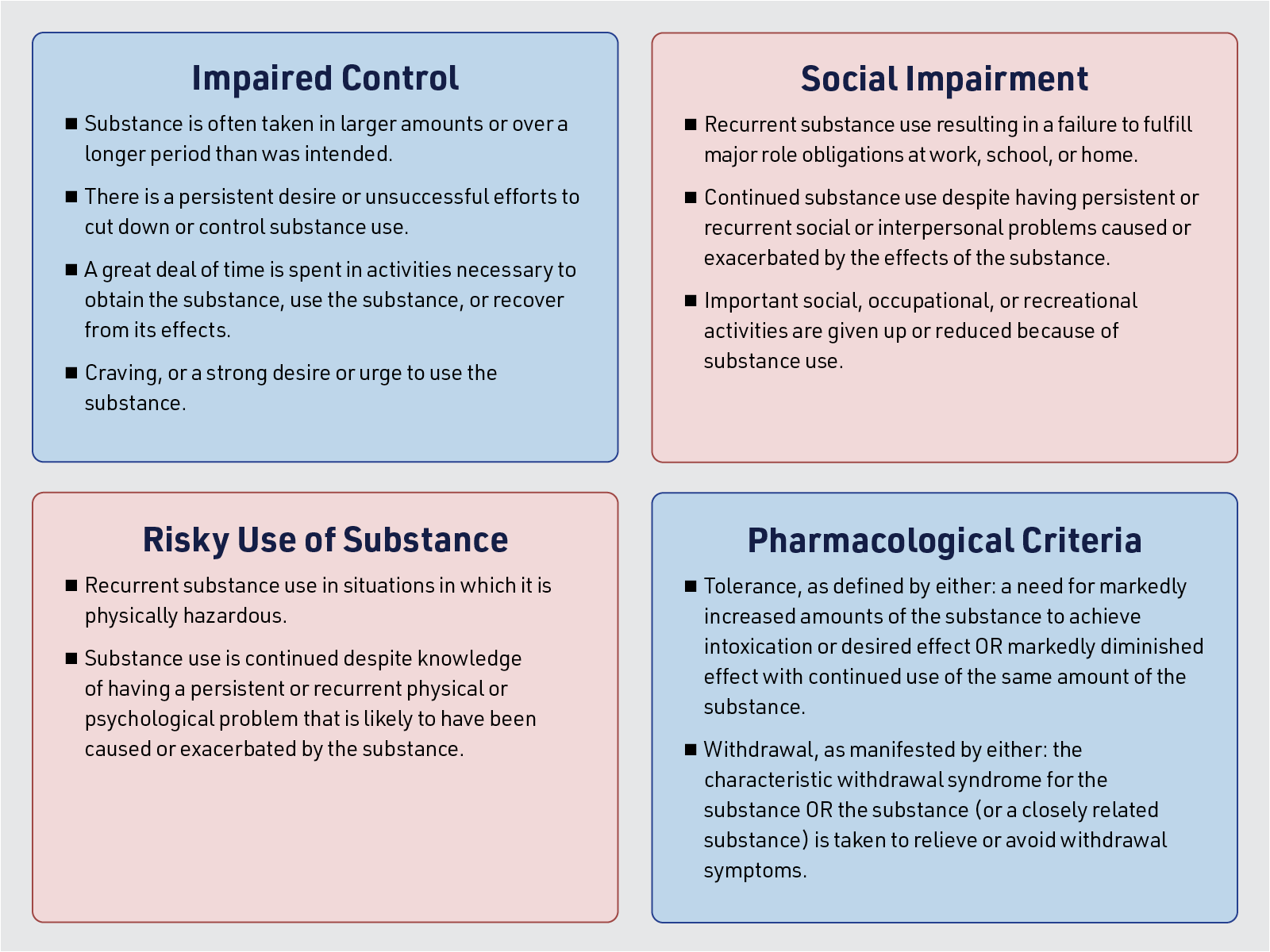
If there are concerns for OUD, such as medication overuse, repeatedly requesting early refills, and/or an inconsistent urine drug screen (UDS) (Table 1), one can consider scheduling a longer-than-usual appointment with the patient and going through the DSM-V criteria with a repeat point of care UDS. It is important to remember that OUD is a clinical diagnosis, and therefore it behooves the clinician to carefully parse the way the patient uses medication (or doesn’t use it) to determine if the criteria are met. When discussing the use of other illicit substances, prepare your verbiage to best ensure your language does not alienate the patient.3
One reasonable approach is to configure the SUD evaluation within the confines of a pain evaluation; for example, ask about pain and medication use at a specific time of day (eg, needing more medication early in the morning and why this might be the case) or ask “is the pain so severe that you run out of medications daily or early each month?” The clinician should also be aware of red flag statements, such as “taking the medicine relaxes me and lets me sleep” as indicative of potential non-medical use although there is likely some component of this effect with most patients who use opioids.
We sometimes even present patients with the DSM-V criteria so that they are aware of how the diagnosis is being made to potentially reduce questioning or resistance.
Step 2: Disclosing to the patient and discussing referral to a SUD clinician
The conversation should begin by framing everything in the context of safety, indicating that the primary goal is to treat patients’ pain while ensuring their well-being. For example, one could say, “We want to treat your pain, but we need to do so safely in a way that doesn’t harm you.” It may be helpful to address specific concerns, such as saying, “I’m concerned about [your medication/the fact that you’re running out early every month].” Sometimes, we even present patients with the DSM-V criteria so that they are aware of how the diagnosis is being made to potentially reduce questioning or resistance.
Regardless of how the diagnosis is presented, however, one should expect some resistance and pushback from the patient. In such situations, it is crucial for clinicians to remain calm, empathetic, and firm in their discussions. Reiterate the primary goal of treating the patient's pain safely and effectively. If clinicians have addiction expertise and qualify to begin treatment (with either medical or psychosocial treatment), they should proceed immediately as the patient will have some confidence and has already established rapport.4
If you do not have experience or board certification in addiction medicine (most pain physicians do not), one should approach the situation by indicating that the pain clinician will “partner” with the addictionologist; it is critical to emphasize that patients will not be abandoned, and their pain complaints will not be ignored. One statement we employ is, “We still want to help you with the pain and have many options we can use. Opioids are just one way that we treat pain, and the evidence for using them long-term is generally negative anyway. Here are some choices we can potentially try.” Many clinicians choose to discharge patients in these circumstances; however, discharging this patient from your practice may risk the patient obtaining medications from non-medical sources (with dangerous additives such as fentanyl and xylazine), suicide attempts, or overdose on other substances (eg, alcohol). It is essential to prioritize patient safety and well-being by continuing to treat the pain as best as you can safely to reduce likelihood of these events while patients are seeking care for their OUD.
Scenario 2: Opioid takeover from a colleague or insurance change, but opioids not indicated
One particularly challenging situation is that in which patients who have been prescribed opioids (often high-dose opioids) for a significant amount of time by a previous clinician (whether they stopped seeing this clinician due to retirement or change in insurance) for a condition or in a situation where the new treating clinician finds this to be inappropriate or not truly indicated. To initiate the conversation clearly and professionally, a key phrase to use is “In my professional medical opinion, opioids are not indicated for your pain.”
The link between mental health and chronic pain is increasingly well-defined; most opioids prescribed in the United States as of 2017 were to individuals with mood disorders (eg, depression, anxiety, and post-traumatic stress disorder),5 and failure to recognize this, among other more systemic challenges in the American healthcare system, often led to significant overprescribing.
In our experience, the best way to approach this is a straightforward discussion of the impact of opioids on function. If the opioids are only marginally reducing pain scores from (for example) 8/10 to 7/10 and not improving function, one could use this information to advise the patient that the medications simply are not helping enough to justify risk of chronic use. One example of phrasing might be, “In my professional medical opinion, the benefits of continuing this medication regimen do not outweigh the risks, and in fact I think it might be the opposite; I cannot in good conscience continue to prescribe something that I frankly feel is dangerous and could result in a bad outcome.”
If the patient then asks what other options are available, one could consider conversion to a buprenorphine product (The X-waiver no longer exists, and all formulations of buprenorphine can be used by any clinician for a pain indication). Utilizing a milligram-dose buprenorphine product would effectively assist with alleviating cravings and withdrawal symptoms and could potentially provide some analgesic effects in conjunction with whatever other medications/modalities are chosen by the clinician.
If a taper is required, one could establish an opioid agreement with a clear end date that can be beneficial to ensure patients understand that 1) they will not be abandoned during the process and 2) there is a well-defined timeline to discontinue these medications and/or explore safer options. It is also incumbent on the clinician to at least reference said agreements at future appointments during discussion of taper and treatment of pain.
Scenario 3: Patient not adherent to opioid agreement but does not meet criteria for SUD
To initiate the conversation, it is essential to have a factual discussion and data-driven objective lab values, such as the opioid risk tool.6 If patients have been taking more medication than prescribed or received an opioid prescription from an outside provider, it is recommended to bring a physical copy of their signed opioid agreement (caveat: your clinic should maintain this on file) into the room during the conversation. The clinician is then able to indicate on the signed agreement where the patient’s behavior is expressly prohibited. In the event of a urine drug screen that returns absent of opioids, ensure that you have established and documented the last time the patient took the medication. Ideally you will ask the patient the last time of medication administration prior to disclosing that you will be checking a urine drug screen. (Table 1)
| Issue | How to Interpret | Conversation Points |
| Other intoxicant present | Certain results can be false+ (fentanyl); others are likely a true+ (cocaine). Clarify likelihood with laboratory staff prior to conversation with patient. |
|
| No expected opioid metabolites present | Clinicians must establish the last use of medication prior to laboratory sample. Most metabolites are present for 2-3 days in urine. |
|
| Dilute sample | Patient was overhydrated prior to providing sample, or water was added to sample for intentional dilution. |
|
A patient reporting suicidal ideation cannot be ignored, even if you suspect this may be a gesture or not genuine.
Special Scenario: Concern for self-harm
A patient reporting suicidal ideation cannot be ignored, even if you suspect this may be a gesture or not genuine. The clinician must always seriously consider that such reports are truly suicidal and respond accordingly. Explaining the gravity of reporting intent to self-harm and possible outcomes can help distinguish if the patient is truly suicidal. Reiterate what you heard the patient say, eg, “What I just heard you say is that you intend to kill yourself if you do not receive this medication. We take your safety very seriously. You understand that if you intend to kill yourself and have an active plan to do so, I am obligated by law to call for a psychiatric evaluation to determine if you need hospitalization.”
It can be helpful to use and document the Columbia-Suicide Severity Rating Scale with the patient still in the room, which will stratify patients into low, moderate, and high risk for suicidal behavior. As an evidence-based screening tool, this tool will help guide your next steps in management.7 During the assessment, it is crucial to determine if patients have a specific plan to commit suicide. Document their response, using quotation marks if it is a direct quotation from the patient. If the patient does not have a plan but expresses suicidal thoughts, make referrals to pain psychology and psychiatry as appropriate. If the patient has a plan to commit suicide, call your county’s mobile crisis team for evaluation of patient capacity. If the 24/7 county mobile crisis team determines patients are an immediate danger to themselves, then they may place a psychiatric hold for inpatient psychiatric care. If patients do not meet criteria for immediate intervention or if they leave against medical advice, then local law enforcement can go to patients’ homes to perform wellness checks. Always explain to patients the reasoning for every action you take and indicate that their safety is the greatest priority.
Conclusion
Conversations about discontinuation of opioids can be fraught, and even seasoned prescribers may approach these discussions with dread. However, it behooves us as a medical community to prioritize opioid safety while still approaching the patient with empathy.
For more information, please join us on December 9th for the Perioperative and Outpatient Management of Patients with Substance Use Disorders Symposium, a one-day virtual event designed for all members of the health care team. Hosted by the Opioid Safety and Substance Use Disorder Special Interest Group (SIG), this symposium intends to bridge the knowledge gap that many health professionals face in treating patients with SUD in the perioperative period or the chronic pain clinic. This symposium meets the requirements for the Medication Access and Training Expansion (MATE) Act and offers 10.5 CME credits.


References
- Weber A, Lynch A, Miskle B, et al. Older adult substance use treatment first-time admissions between 2008 and 2018. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry 2022;30(10):1055–63. https://doi.org/10.1016/j.jagp.2022.03.003
- Ashford RD, Brown AM, Curtis B. “Abusing Addiction”: our language still isn’t good enough. Alcohol Treat Q2019;37(2):257–72. https://doi.org/10.1080/07347324.2018.1513777
- Ashford RD, Brown AM, McDaniel J, et al. Biased labels: an experimental study of language and stigma among individuals in recovery and health professionals. Subst Use Misuse 2019;54(8):1376–84. https://doi.org/10.1080/10826084.2019.1581221
- Pivovarova E, Stein MD. In their own words: language preferences of individuals who use heroin. Addict Abingdon Engl 2019;114(10):1785–90. https://doi.org/10.1111/add.14699
- Davis MA, Lin LA, Liu H, et al. Prescription opioid use among adults with mental health disorders in the United States. J Am Board Fam Med 2017;30(4):407-17. https://doi.org/10.3122/jabfm.2017.04.170112
- Cheatle MD, Compton PA, Dhingra L, et al. Development of the revised opioid risk tool to predict opioid use disorder in patients with chronic nonmalignant pain. J Pain 2019;20(7):842–51. https://doi.org/10.1016/j.jpain.2019.01.011
- Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry2011;168(12):1266–77. https://doi.org/10.1176/appi.ajp.2011.10111704
