How I Do It
Learn from your colleagues. ASRA Pain Medicine members share how they perform common procedures and accomplish other tasks.
- Listed by publication date, most recent on top
How I Do It: Ultrasound-Guided Injection for the Shoulder (Part 2)
This article originally appeared in the ASRA News,Volume 13, Issue 2, pp 9-12 (May 2013).
Author
Philip Peng MBBS, FRCPC, Founder (Pain Medicine)
Department of Anesthesia and Pain Management
University Health Network and Mount Sinai Hospital
University of Toronto, Toronto, Canada
Section Editor: David Provenzano, MD
This article summarizes the anatomy, sonoanatomy, efficacy, accuracy, and the injection techniques for the glenohumeral joint (GHJ) and subacromial subdeltoid bursa (SASDB). Patient selection for those injections is also reviewed. A detailed review can be found in two recent articles.[1,2]
Glenohumeral Joint
Anatomy and Sonoanatomy
The GHJ is a ball-and-socket joint composed of a round humeral head and a relatively small, flat pear-shaped glenoid fossa. The glenoid cavity is deepened by the presence of a fibrocartiginous rim, the glenoid labrum (Figure 1). The joint capsule is attached medially to the margin of the glenoid cavity extending to the base of the coracoid process and laterally to the anatomical neck of the humerus (Figure 1).[3,4] The synovial membrane lines the capsule on its deep surface and overlies the long head of biceps (LHB) tendon. From there, three recesses are formed: the biceps tendon sheath anteriorly, the subscapularis recess medially, and the axillary pouch inferiorly (Figure 2).[3] The presence of the LHB recess allows a potential portal for GHJ entry.[1,3]
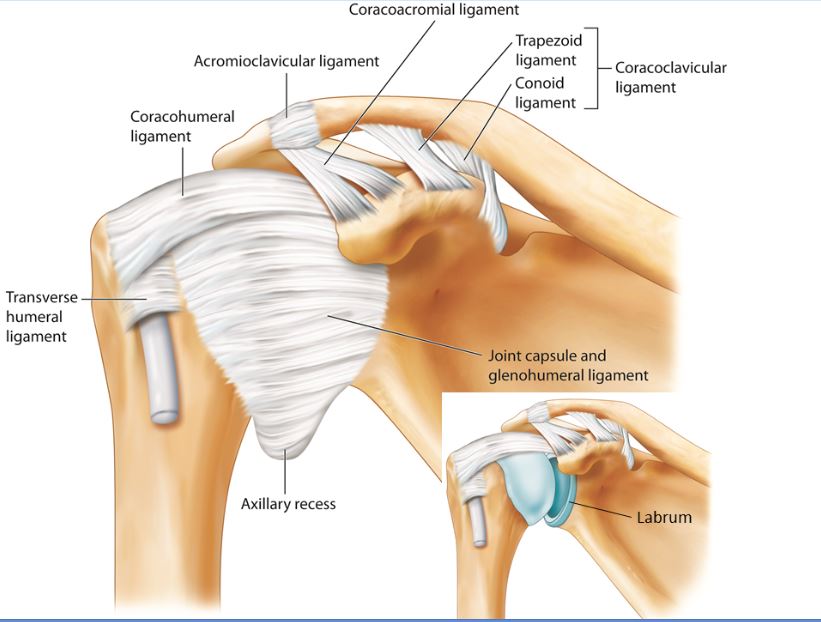
Figure 1: Glenohumeral joint showing various ligaments and the joint capsule. The anterior capsule is reinforced by the superior, middle and inferior glenohumeral ligament. The insert shows the articular surface, glenoid process, and labrum. Reprint with permission from usra.ca.
The GHJ can be accessed anteriorly, posteriorly, and from the rotator cuff interval.[1] The techniques for the anterior and posterior approaches will be described. For the posterior approach, the patient is placed in either the sitting or lateral decubitus position with the ipsilateral hand placed on the contralateral shoulder. A linear probe of frequency 6-13 MHz is usually used unless the patient is of very high body mass index or strong muscular build. The ultrasound probe is placed just caudal to the acromion over the infraspinatus tendon (Figure 3). The key structures to identify are humeral head, labrum, infraspinatus tendon, and joint capsule. For the anterior rotator cuff interval approach, the patient is placed in supine position and a high frequency linear probe 6-13 MHz is used. The first scan is similar to the scanning of the long head of the biceps (LHB) tendon at the bicipital groove. Following this scan, the LHB is traced in the cephalad and medial direction until it is seen in between the supraspinatus and subscapularis muscle underneath the coraco-humeral ligament (Video 1).
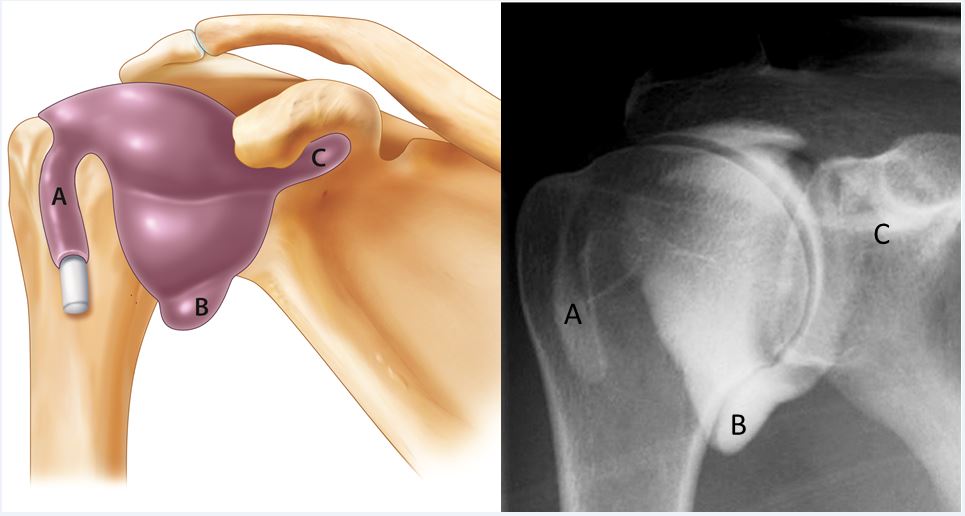
Figure 2: The drawing of three main recesses of the joint (left): A=the biceps tendon sheath; B=the axillary pouch; C=the subscapular recess; and the corresponding radiographic (arthrogram) appearance (right). Reprint with permission from usra.ca.
Injection Techniques
The target for the posterior approach is between the free edge of labrum and the cartilage of humeral head underneath the capsule (Video 2).[1,2] Once the target is obtained, a 22 gauge 3.5-inch spinal needle is inserted from lateral to medial direction with in-plane technique. The injectate is 4 mL of local anesthetic with steroid (e.g., 2% lidocaine and 40 mg methylprednisolone acetate). If one encounters resistance during injection with the posterior approach, two maneuvers can be used to adjust the needle: turn the bevel 90 degrees or withdraw the needle slightly. Correct placement of injectate in the posterior approach will result in the spread of medication beneath the joint capsule.
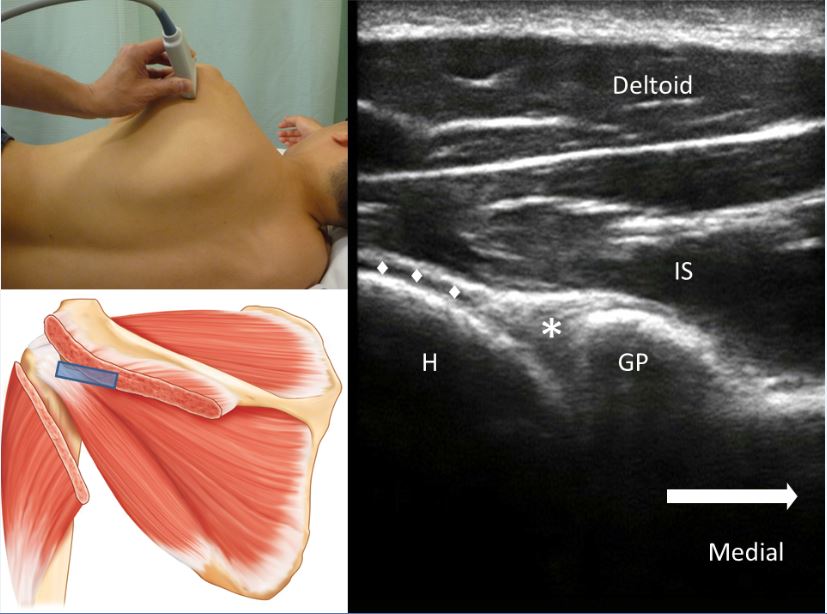
Figure 3: Ultrasound image of the posterior glenohumeral joint. The glenoid process and humeral head both appear as hyperechoic structures with anechoic shadow. The insert on the top shows the position of the patient and the ultrasound probe while one below shows the probe position and the structures underneath; IS=-infraspinatus muscle; H=humeral head; GP=glenoid process; *=glenoid labrum; •=the articular cartilage of the humeral head. Reprint with permission from usra.ca.
Video 1: Video showing the scan of the rotator cuff interval. Created by Dr. Phillip Peng and reproduced with permission from usra.ca.
Video 2: Video showing the needle insertion for the glenohumeral joint injection. Created by Dr. Phillip Peng and reproduced with permission from usra.ca.
The target for the rotator cuff interval approach is the space on either side of the LHB deep to the coracohumeral ligament (Figure 4). Once the target image is obtained, a 25 gauge 1.5-inch needle is inserted either out-of-plane (caudal to cephalad direction) or in-plane (lateral to medial direction). The injectate is local anesthetic with steroid as previously described.[1,2]
Literature Review
The main indications for GHJ injection are adhesive capsulitis and glenohumeral arthrosis. The efficacy for adhesive capsulitis had been reviewed.[5] Compared with control and physiotherapy, the review showed that multiple injections were beneficial until 16 weeks from the date of the first injection. In terms of multiple injections, this review supported that up to 3 injections were beneficial, but there was limited evidence that 4 to 6 injections were beneficial. The role of GHJ injection as part of the conservative therapies for adhesive capsulitis needs to be emphasized. Intra-articular steroid injection has been shown to produce significant reduction in pain and disability after treatment when combined with exercise versus exercise alone.[5]
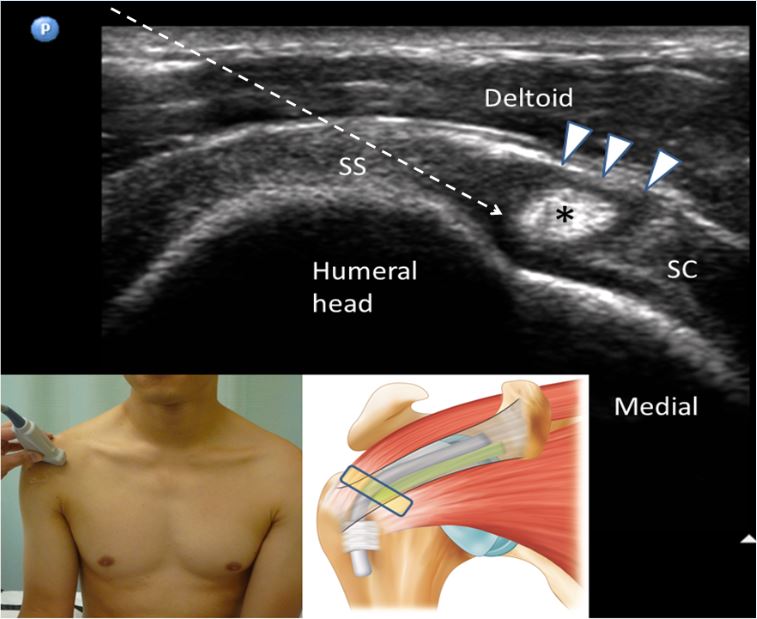
Figure 4: Ultrasound image of the rotator cuff interval and the needle insertion trajectory. The insert shows the position of the probe and corresponding anatomical structures underneath. The LHB tendon (*) is always hyperechoic at this level and sandwiched between the supraspinatus tendon (SS) laterally and subscapularis tendon (SC) medially. The coracohumeral ligament (arrow heads) forms the roof of the interval. The needle (indicated by the dashed arrow) is inserted from lateral to medial into the rotator cuff interval. Reprint with permission from usra.ca.
Video 3: Dynamic scan of the supraspinatus tendon in the long axis. Arrows indicate the subacromial subdeltoid bursa. Created by Dr. Phillip Peng and reproduced with permission from usra.ca.
Video 4: Video showing the dynamic scan of the supraspinatus tendon in the long axis and then to short axis. Created by Dr. Phillip Peng and reproduced with permission from usra.ca.
Video 5: Video showing the injection of the subacromial subdeltoid bursa. Created by Dr. Phillip Peng and reproduced with permission from usra.ca.
The role of GHJ injection in the management of arthrosis is unclear. There are no studies specifically addressing the efficacy in GHJ arthrosis. A recent practice guideline from the American Academy of Orthopedic Surgery found no evidence to support or refute the use of intra-articular corticosteroid injection for the treatment of GHJ arthrosis.[7] There is some evidence to support the use of viscosupplement in GHJ osteoarthritis, an off-label use for viscosupplement, based on an industry-sponsored study.[8]
The overall success rates of the landmark-based technique range from 27% to 100%.1 In contrast, the success rates of the ultrasound-guided studies are consistently higher. A recent review examining the accuracy of GHJ injection demonstrated that the pooled success rates of the landmark-based and image-guided were 79% and 95% respectively.[9] Of note, an interesting comparison study was conducted examining the ultrasound-guided approach and landmark-based (conventional) approach in various joint interventions. The ultrasound-guided injections were all performed by a rheumatology trainee (9 months into a rheumatology program with 8 sessions of MSK ultrasound training), and the conventional approach was all performed by 9 rheumatology consultants with a median of 9 years of experience.[10] The accuracy rates for shoulder injections were 63% and 40% for the ultrasound and conventional groups, respectively. Despite the contrast in experience, the trainee achieved better accuracy, which was associated with better pain relief at the sixth week.
Subacromial Subdeltoid Bursa
Anatomy and Sonnanatomy
There are four rotator cuff muscles: subscapularis (SSC), supraspinatus (SS), infraspinatus (IS) and teres minor (TMi) muscles. The rotator cuff is a tight layer of tendons around the GHJ on the anterior (SSC), superior (SS), and posterior (IS and TMi) aspects of the shoulder.[1,3,11] It plays an important role to stabilize the humeral head in the shallow glenoid fossa during movement of the arm. The subacromial subdeltoid bursa (SASDB), the largest bursa in the body, is located inferior to the acromion, the coraco-acromial ligament (CAL), and the deltoid muscle. It overlies the superior aspect of the SS tendon.[3,11] It also extends anteriorly to cover the bicipital groove and medially to the coracoid process (subcoracoid bursa). The lateral border may reach approximately 3 cm below the greater tuberosity.[3] The main role of the SASDB is to minimize attrition of the cuff against the coracoacromial arch (acromion and CAL) and deltoid muscle during movements of the arm.
To reveal the SASDB, the patient is placed either supine or sitting in the reclining position with the back supported. The patient is advised to put the hand in modified Crass position (gesture of “put the money back in the back pocket”). The ultrasound probe used is high frequency 6-13 MHz linear, and the SASDB can be viewed in either long- or short-axis (Videos 3 and 4).
Injection Technique
The target is the bursa outlined by the peribursal fat. A 25 gauge 1.5-inch needle or 22 gauge 3.5-inch spinal needle is inserted in-plane. If the needle tip is in the bursa, a small volume (0.5 mL) of injectate will be seen spreading across the bursa plane (Video 5). Once the position of the needle is satisfactory, 4 mL of local anesthetic with steroid (0.25% bupivacaine and 40 mg methylprednisolone acetate) can be injected.
The indication for SASBD injection is subacromial impingement syndrome, which covers a constellation of conditions: partial- and full-thickness rotator cuff tear and rotator cuff tendinopathy.[12] The common presentations of patients with rotator cuff disease are pain and stiffness. Pain is the predominant symptom, often most troubling at night and with overhead activities. The rotator cuff tear can be articular-sided, bursal-sided, or intratendinous, and the incidence increases with age. The tear can be partial- or full-thickness, but partial tendon lesions are often much more painful than full-thickness tears.[13] Literature Review
Physical examination reveals pain with active range of motion between 60 and 100 degrees of abduction (painful arc), as well as loss of active range of motion but relatively-preserved passive range of motion. Both are suggestive of a rotator cuff pathology. Provocative tests for rotator cuff pathology are Hawkins’ impingement test, Neer’s test, and “empty can” supraspinatus test.[2]
The efficacy of SASDB injections for rotator cuff disease has been the subject of multiple reviews.[1] One of the more recent systematic review included 9 randomized controlled trials specifically appraising the use of subacromial steroid injections in rotator cuff disease.[14] The authors concluded that subacromial steroid injection was not efficacious in the treatment of rotator cuff disease. It is important to note that the injection techniques included in those 9 studies were all ‘‘blind’’ injection, with the exception of 1 study in which injections were performed with X-ray guidance. Previous investigation has suggested that the X-ray-guided technique is not reliable or dependable.[15]
In a practical clinical setting, subacromial injection is usually performed in a multimodal approach with physiotherapy or a rehabilitation protocol. A recent large, pragmatic, randomized controlled trial[16] showed that the subacromial steroid injection decreased pain and improved functional outcome at 1 and 6 weeks, but there was no difference compared with exercise alone at 3 and 6 months. The absence of long-term efficacy is not uncommon for interventions of common MSK problems. In examining results from recent high-quality randomized controlled trials for common MSK disorders, Foster et al found no or very small differences in the effectiveness of different approaches when based on long-term outcomes (6-12 months).[17] This has been exemplified by the various shoulder injection techniques described in the previous sections.
The SASDB is a very small target, and precise injection should be performed with image guidance. With the exception of one study (which showed 100% success rate[18]), the literature demonstrates success rates for landmark-based approaches ranging from 29% to 70% in clinical studies and 70% to 91% in cadaver studies.[1] The success rates were similar irrespective of different approaches (posterior, anterolateral, and lateral) for the blind injection and experience and confidence of the practitioners. In studies in which the blind procedures were performed by very experienced orthopedic surgeons and shoulder specialists, the confidence correlation (the accuracy rate when the practitioners were very confident that they were accurate) ranged from 42% to 66%.[19.20]
Among those commonly-used imaging modalities, Mathews and Glousman[15] found that X-ray was an unreliable method in confirming the location of contrast in the subacromial space. Ultrasound-guided injection was validated with MRI in one study, and the accuracy was 100%. The use of the ultrasound-imaging technique in the diagnosis of rotator cuff disease has been extensively investigated, and the reliability is comparable with that of MRI.[21-23]
Conclusion
Application of ultrasound for shoulder injection is increasingly popular. Ultrasonography allows accurate localization of the various target structures for shoulder injections and real-time guidance of needle insertion. An in-depth understanding of the anatomy and sonoanatomy is of paramount importance in performing these ultrasound-guided injections.
References
- Peng PWH, Cheng P. Ultrasound-guided interventional procedures in pain Medicine: A review of anatomy, sonoanatomy and procedures. Part III: Shoulder. Reg Anesth Pain Med 2011; 36: 592-605
- Peng PWH. Ultrasound-guided shoulder injection. In: Philip WH Peng (ed). Ultrasound for Pain Medicine Intervention: A Practical Guide. Vol. 4: Musculoskeletal structures. Philip Peng Education Series-iBook series. (Release March 2013)
- Bianchi S, Martinoli C. Shoulder. In: Bianchi S, Martinoli C. Ultrasound of the Musculoskeletal System. Berlin, Germany: Springer-Verlag Berlin Heidelberg, 2007
- Iannotti JP, Gabriel JP, Schneck SL, et al. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am 1992; 74:491-500
- Shah N, Lewis M. Shoulder adhesive capsulitis: systematic review of randomised trials using multiple corticosteroid injections. Br J Gen Pract. 2007;57:662-667.
- Carette S, Moffet H, Tardif J, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo controlled trial. Arthritis Rheum. 2003; 48:829-838.
- Izquierdo R, Voloshin I, Edwards S, et al. AAOS clinical practice guideline summary-treatment of glenohumeral osteoarthritis. J Am Acad Orthop Surg. 2010; 18:375-382.
- Blaine T, Moskowitz R, Udell J, et al. Treatment of persistent shoulder pain with sodium hyaluronate: a randomized, controlled trial. A multicenter study. J Bone Joint Surg Am. 2008; 90:970-979.
- Daley EL, Bajaj S, Bisson LJ, Cole BJ. Improving injection accuracy of the elbow, knee, and shoulder. Does injection site and imaging make a difference? A systematic review. Am J Sports Med 2011; 39: 656-662
- Cunnington J, Marshall N, Hide G, et al. A randomized, double-blind, controlled study of ultrasound-guided corticosteroid injection into?the joint of patients with inflammatory arthritis. Arthritis Rheum. 2010;62:1862-1869
- DeFranco MJ, Cole BJ. Current perspectives on rotator cuff anatomy. 2009; 25:305-320
- Gruson KI, Ruchelsman DE, Zuckerman JD. Subacromial corticosteroid injections. J Shoulder Elbow Surg 2008;17:118S-130S
- Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman’s classic. J Shoulder Elbow Surg. 2000; 9:163-168
- Koester MC, Dunn WR, Kuhn JE, Spindler KP. The efficacy of subacromial. corticosteroid injection in the treatment of rotator cuff disease: a systematic review. J Am Acad Orthop Surg. 2007;15:3-11.
- Mathews PV, Glousman RE. Accuracy of subacromial injection: anterolateral. versus posterior approach. J Shoulder Elbow Surg. 2005; 14:145-148.
- Crawshaw DP, Helliwell PS, Hensor EMA, Hay EM, Aldous SJ, Conaghan PG. Exercise therapy after corticosteroid injection?for moderate to severe shoulder. pain: large pragmatic randomised trial. BMJ. 2010;340:c3037
- Foster NE, Dziedzic KS, van der Windt DA, Fritz JM, Hay EM. Research priorities for non-pharmacological therapies for common musculoskeletal problems: nationally and internationally agreed recommendations. BMC Musculoskelet Disord. 2009;10:3.
- Rutten MJ, Maresch BJ, Jager GJ, de Waal Malefijt MC. Injection of the subacromial-subdeltoid bursa: blind or ultrasound-guided? Acta Orthop. 2007;78:254-257
- Henkus HE, Cobben LP, Coerkamp EG, Nelissen RG, van Arkel ER. The accuracy of subacromial injections: a prospective randomized magnetic resonance. imaging study. Arthroscopy. 2006; 22:277-282.
- Park JY, Siti HT, KS O, Chung KT, Lee JY, Oh JH. Blind subacromial injection. from the anterolateral approach: the ballooning sign.?J Shoulder Elbow Surg. 2010;19:1070-1075.
- Rutten MCJM, Maresch BJ, Jager GJ, Blickman JG, van Holsbeeck MT. Ultrasound of the rotator cuff with MRI and anatomic correlation. Eur J Radiol. 2007; 82:427-436.
- Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. 2005; 87:1305-1311.
- Milosavljevic J, Elvin A, Rahme H. Ultrasonography of the rotator cuff: a comparison with arthroscopy in one hundred- and-ninety consecutive cases. Acta Radiol. 2005;46:858-865.
Leave a commentOrder by
Newest on top Oldest on top