How I Do It
Learn from your colleagues. ASRA Pain Medicine members share how they perform common procedures and accomplish other tasks.
- Listed by publication date, most recent on top
How I Do It: Ultrasound-Guided Combined Suprascapular and Axillary Nerve Block
This article originally appeared in ASRA News, Volume 13, Number 4, pp. 22-25(November 2013).
Author
Darcy J. Price, MBChB, FANZCA
North Shore Hospital and University of Auckland
Auckland, New Zealand
Section Editor: Steven Orebaugh, MD
Introduction
Pain following shoulder surgery can be severe and has traditionally been controlled using an interscalene nerve block (ISB).[1] This technique is associated with well-documented adverse effects, including unwelcome arm paralysis, and intolerance of hemidiaphragm paralysis.[2] ISB is also associated with more frequent long-term neurological deficits compared to other nerve blocks[3,4] and must be performed in proximity to important anatomical structures (e.g., vertebral artery). Thus an alternative to ISB may be advantageous and has been described, whereby terminal nerves supplying the shoulder joint are blocked rather than the entire brachial plexus.[5-7] Combined suprascapular and axillary nerve block (CSANB) appears to be an effective alternative to ISB for pain relief following shoulder surgery,[6,7] with the advantages of minimal side effects, reduced potential for serious complications, and less reported pain during block resolution.[6,7]
Anatomy
Five nerves innervate the shoulder joint and associated structures. The suprascapular nerve (SN) carries the most extensive supply; a lesser amount travels via the axillary nerve (AN) (Fig. 1).[8] The lateral pectoral, musculocutaneous and subscapular nerves are responsible for only minor contributions (Fig. 1).[8]
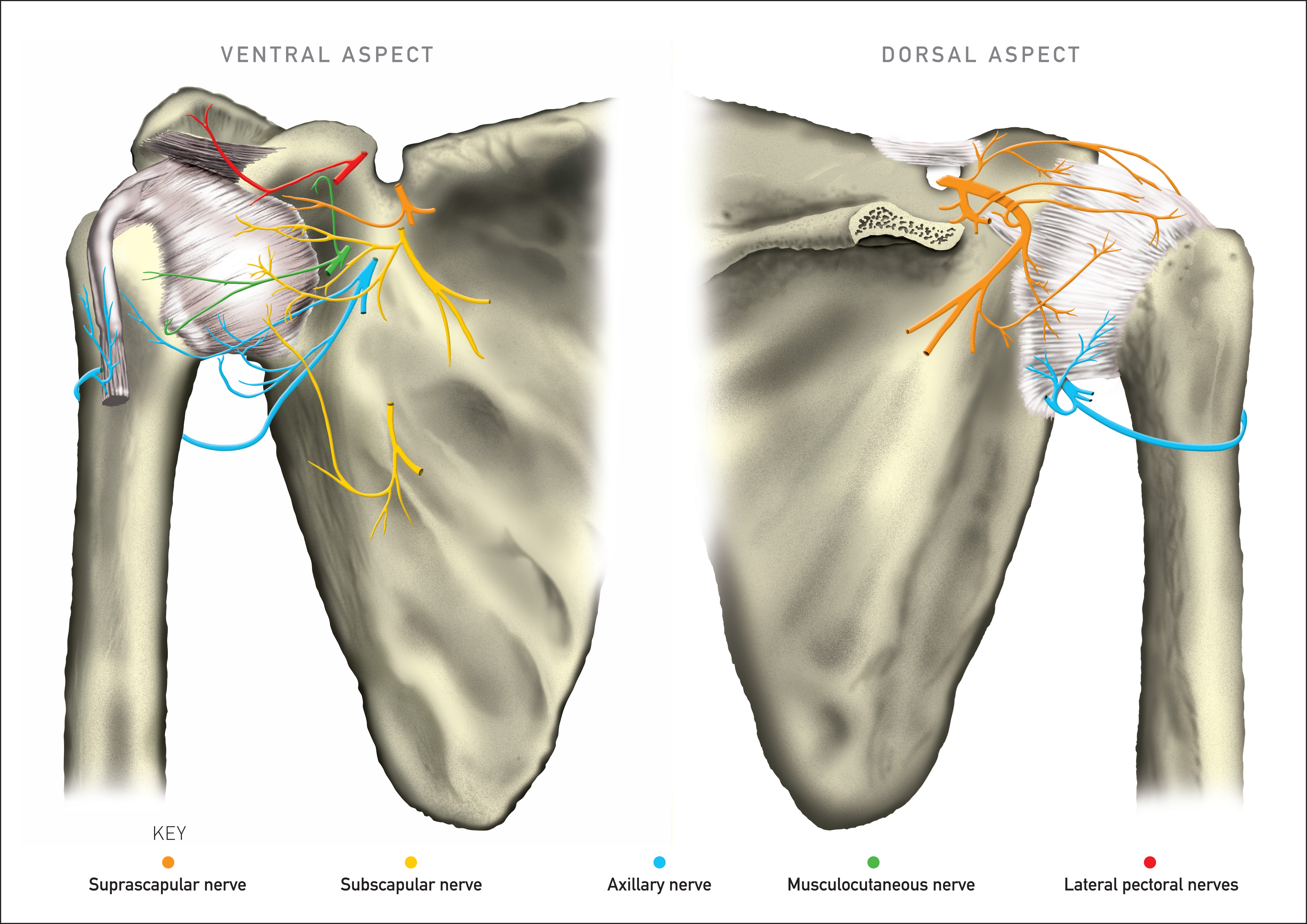 Figure 1. Innervation of the ventral and dorsal shoulder joint and capsule
Figure 1. Innervation of the ventral and dorsal shoulder joint and capsule
History
While searching for an alternative to ISB, I reasoned that a minimum requirement was blockade of the suprascapular nerve (SNB). The question to be answered was whether the addition of AN blockade (ANB) would result in better analgesia than SNB alone.[9] I initially developed a landmark-based technique (with or without nerve stimulation) using Meier’s SNB10 and my own description of ANB.[5] It has proven to be quick and reliable to perform, as both nerves are blocked where they run across bone: SN on the lateral floor of supraspinous fossa (LFSF),[10] and AN on the posterior surface of the humerus (PSH).[5]
Relevant sonoanatomy
The SN and AN are both narrow and lie deep to large muscles, which make them difficult to locate with US. To enhance my understanding of the sonoanatomy, I studied ultrasound (US) images of the SN and the AN in 50 volunteers.[9] Each nerve was imaged in three separate regions in both short axis (SAX) and long axis (LAX); the structure most reliably visualized was bone, followed by artery and then nerve.[11] In addition, a radiologist at my institution reviewed 37 routine shoulder MRIs, determining how frequently the SN lies on the LFSF, beneath supraspinatus, and the AN lies beneath deltoid on the PSH.[11] For both nerves, the result was 100%; thus, as for the “blind” landmark technique, locating bone appears to be the key to a quick and reliable US-guided approach to CSANB.[11]
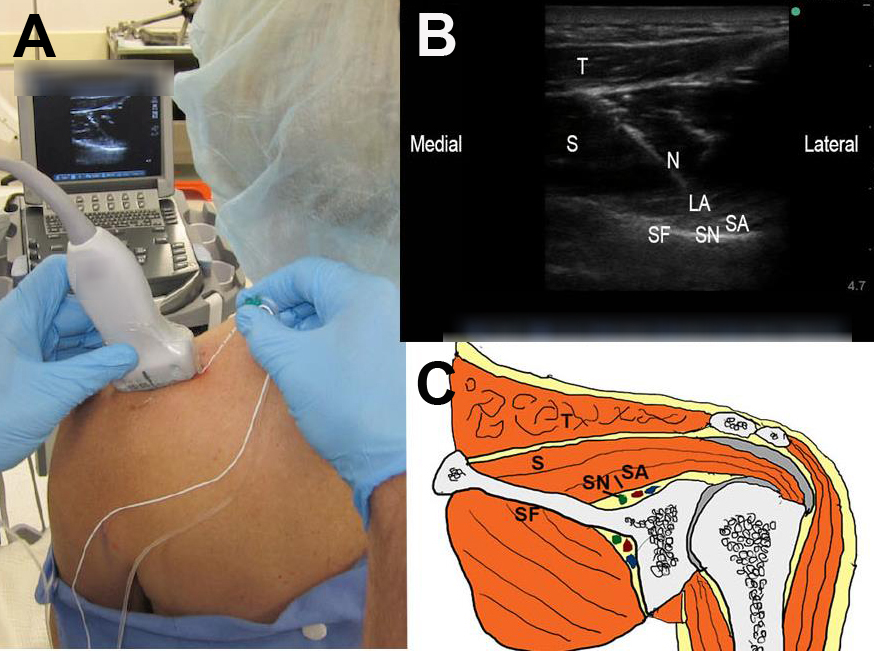
The best images of the SN and the suprascapular artery (SA) are found in the LFSF, in the LAX of the fossa (Fig. 2). This region is superior to imaging in either the suprascapular notch and or the greater scapular (spinoglenoid) notch. The best images of the AN and the circumflex artery (CA) are found on PSH in LAX of the humerus (Fig. 3). This region is superior to imaging in either the quadrilateral space (QS) or the lateral aspect of the humerus.[11]
Figure 2. Positioning (A), imaging (B), and relevant anatomy (C) for ultrasound-guided suprascapular nerve block in lateral floor and in long-axis; T = trapezius, N = needle, S = supraspinatus, SN = suprascapular nerve, LA = local, anaesthetic, SA = suprascapular artery, SF = supraspinous fossa
Suprascapular Nerve Block (SNB)
Imaging the supraspinous fossa is critical to locating the SN; you may also image the SA, as they travel together in a neurovascular bundle (NVB). If the NVB is not visible (33% of cases in the above study[11]), directing the needle onto the LFSF and injecting 10 to 15 ml of LA under supraspinatus will reliably block the SN. Technically, this is easiest to perform in the LAX of the fossa with the needle in-plane (Fig. 2A and 2B). The floor of the fossa has a characteristic “ice hockey stick” pattern in this view; the tip should be aiming at the most lateral part (Figs. 2B and 2C).
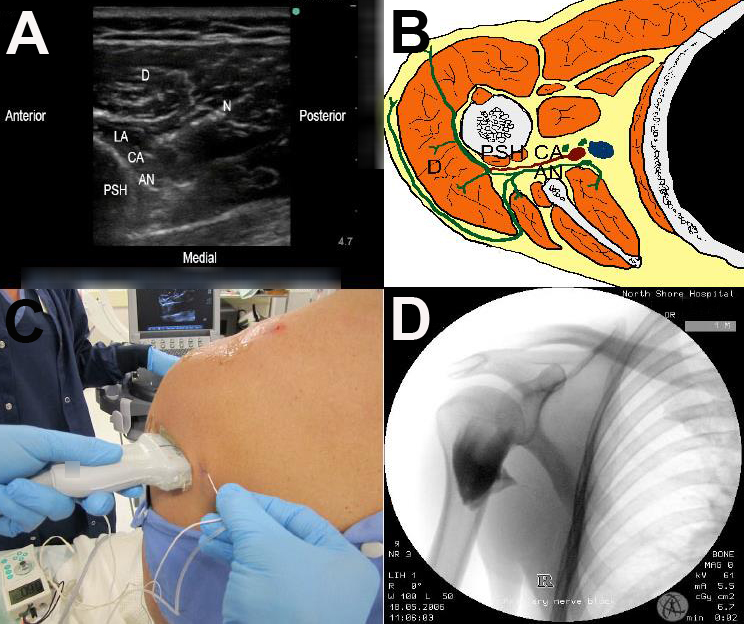
Figure 3. Imaging (A), relevant anatomy (B), positioning (C), and contrast-enhanced spread of local anesthetic (D) for ultrasound-guided axillary nerve block in short-axis; D = deltoid, N = needle, CA = circumflex artery, LA = local anaesthetic, AN = axillary nerve, PSH = posterior surface of humerus
Axillary Nerve Block (ANB)
Likewise, imaging the humerus is critical to locating the AN. Imaging the PSH may permit location of the CA, which travels with the AN in a NVB beneath posterior deltoid. If the NVB is not visible (5-10% of cases in the above study[11]), directing the needle onto the PSH, and imaging LA spread under deltoid will result in ANB. The posterior shoulder capsule (PSC) can assist in determining the correct point on the PSH to inject LA. In LAX, the PSC causes the periosteum to become fuzzy; LA is injected 1-2 cm below the PSC. It can also be seen in short axis of the humerus, by scanning superiorly until the circular periosteal image becomes blurred.
The most logical approach would appear to be in LAX of the PSH; the CA and AN appear in cross-section, and successful ANB has been described with this approach.[12] However, the PSH is difficult to keep in view, as small probe movements result in loss of a clear image. In contrast, the SAX view of the humerus is more stable, and this is my preferred technique despite the AN and CA being imaged longitudinally (Figs. 3A and 3B). Placing the probe slightly lateral reduces the distance from skin to PSH and permits needle passage in-plane from a similar insertion point as with the landmark technique (Fig. 3C).
Even if imaging the NVB is impossible, locating the shoulder capsule as detailed above will allow successful ANB if LA fills the space under deltoid on the PSH (Fig. 3B). This is reinforced by imaging contrast-enhanced LA spread with fluoroscopy during shoulder block (Fig. 3D); a potential space exists, limited laterally by entry of the AN into the deltoid, and medially by the QS. I use 5-7 ml of LA, as 10 ml or greater is associated with higher rates of spread to the posterior cord via the QS, resulting in radial nerve blockade.
Practical Tips:
- Indications: CSANB is limited to providing analgesia, rather than full surgical anesthesia, but can be effective for arthroscopic or open shoulder surgery.
- Perioperative opioid: CSANB requires additional systemic opioid analgesia, and can have varying degrees of anterior shoulder discomfort on emergence.
- Position: I do most of these blocks with the patient seated. Another option is lateral decubitus position, which may make it is easier to block the AN but harder to perform SNB.
Conclusion
CSANB is an effective alternative to ISB for analgesia following shoulder surgery and can be performed using US despite the nerves being small and relatively deep. As with the landmark-based technique, locating bone (PSH and LFSF) makes performance of these blocks quick, safe, and reliable.
References
- Borgeat A, Ekatodramis G: Anaesthesia for shoulder surgery. Best Pract Res Clin Anaesthesiol 2002; 16 (2): 211-225
- Urmey W, Gloeggler M. Pulmonary function changes during interscalene brachial plexus block: effects of decreasing local anaesthetic injection volume. Reg Anesth 1993;18: 244-249
- Borgeat A, Ekatodramis G, Kalbere F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology 2001; 95:875-880
- Sites BD, Taenzer AH, Herrick MD, Gilloon C, Antonakakis J, Richins J, Beach ML. Incidence of local anesthetic systemic toxicity and postoperative neurologic symptoms associated with 12,668 ultrasound-guided nerve blocks. An analysis from a prospective clinical registry. Reg Anesth Pain Med 2012;37: 478-482
- Price DJ. The shoulder block: a new alternative to interscalene brachial plexus blockade for the control of postoperative shoulder pain. Anaesthesia Intensive Care 2007;35:575-81
- Lee SM, Park S-E, Nam Y-S, Han, S-H, Choi S-Y, Park J-S. Analgesia effectiveness of nerve block in shoulder arthroscopy:comparison betweeninterscalene, suprascapular and axillary nerve blocks. Knee Surg Sports, Traumatol Arthrosc. 2012;20:2573-2578.
- Price D, Abeysekera A, Chaddock M. A randomised comparison of combined suprascapular and axillary (circumflex) nerve block with interscalene block for postoperative analgesia following arthroscopic shoulder surgery. Anaesth Intensive Care 2012. 40,1 183-184
- Halata Z, Bauman K. Mechanoreceptors of the shoulder joint: structure and function. In: Atlas of Functional Shoulder Anatomy Di Giacomo G, Pouliart N, Costantini A. Milan: Springer 2008; 206-208
- Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: a comparison of intraarticular analgesia, suprascapular nerve block and interscalene brachial plexus block. Anesth Analg 2004; 99:589-592
- Meier G, Buettner J. Suprascapular Nerve Block. In: Peripheral Regional Anesthesia: An Atlas of Anatomy and Techniques. Stuttgart: Thieme 2006; 48-54
- Price D, Kershaw, N, Clark B, Fletcher T. An overview of the anatomy of the suprascapular and axillary nerves using ultrasound and magnetic resonance imaging. Anaesth Intensive Care 2012 40,1:183
- Rothe C, Asghar S, Andersen HL, Christensen JK, Lange KH. Ultrasound-guided block of the axillary nerve: a volunteer study of a new method. Acta Anaesthesiol Scand. 2011 May;55(5):565-570
Leave a commentOrder by
Newest on top Oldest on top