How I Do It: PEricapsular Nerve Group (PENG) Block
Cite as: Kolli S, Nimma SR, Kukreja P, et al. How I do it: pericapsular nerve group (PENG) block. ASRA Pain Medicine News 2023;48. https://doi.org/10.52211/asra080123.007.
Introduction
PEricapsular Nerve Group (PENG) block is a fascial plane block where local anesthetic is injected in the fascial plane between the psoas tendon and the ilium, aiming to block the articular branches of the femoral, obturator, and accessory obturator nerves that provide sensory innervation to the anterior capsule. Total hip arthroplasty is the second most common joint replacement surgery.1 Hip fracture is common in the elderly population, and pain control is often challenging. The innervation to the hip joint is complex, and providing analgesia with any single technique is challenging. Therefore, having a thorough understanding of the anatomy of the hip joint capsule is critical for a more targeted intervention. Girón-Arango2 and her colleagues were first to describe the PENG block for peri-operative analgesia for hip fractures based on a comprehensive study of the anterior hip innervation published by Short et al.3
Anatomy of the Hip Joint Capsule
The hip joint is a ball and socket type of synovial joint with articulation between the head of the femur and acetabulum of the hip bone. The joint capsule of the hip attaches to the acetabular labrum and the transverse acetabular ligament proximally. A strong fibrous capsule and ligaments accommodate and support a wide range of movement. The blood supply to the hip joint is supplied by branches of the femoral artery, including the medial circumflex femoral and lateral circumflex femoral arteries.
The nerve supply of the hip joint is complex and comes from multiple articular branches. The anterior hip capsule is innervated by the articular branches from the femoral, obturator, and accessory obturator nerves, while the posterior capsule is innervated by branches from the sacral plexus.3 In general, most of the nociceptive fibers are highly concentrated in the anterior and superolateral capsule, and the posterior hip innervation is mainly comprised of mechanoreceptors.4 The articular branches of the femoral and accessory obturator nerves can be found between the anterior inferior iliac spine (AIIS) and the iliopubic eminence (IPE) (Figure 1 and Figure 2). The articular branches of the obturator nerve can be blocked separately at the inferior aspect of the inferomedial acetabulum or by a pericapsular spread from high volume injectate administered between the AIIS and IPE.
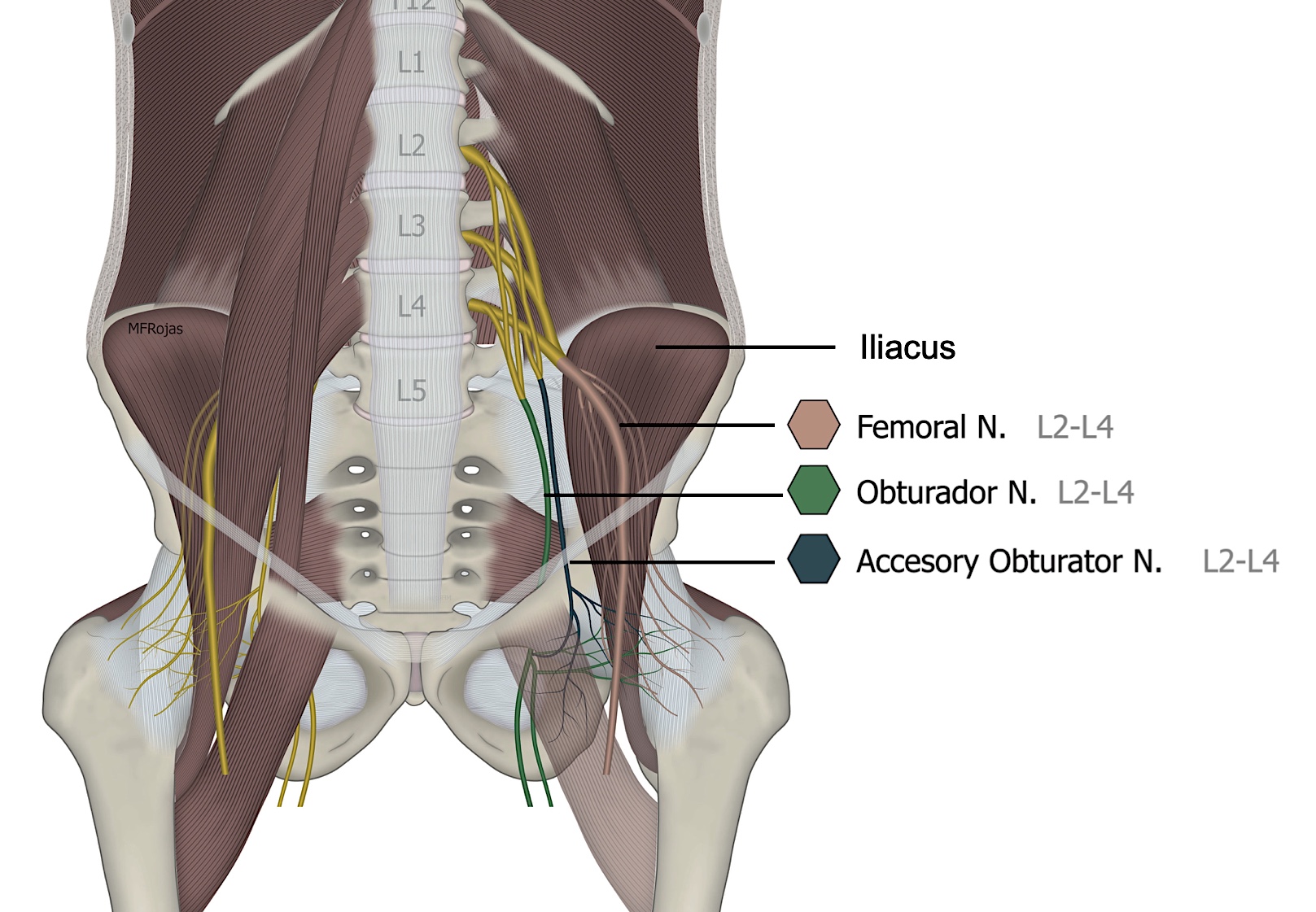
Reproduced with permission from Dr. Maria Fernanda Rojas
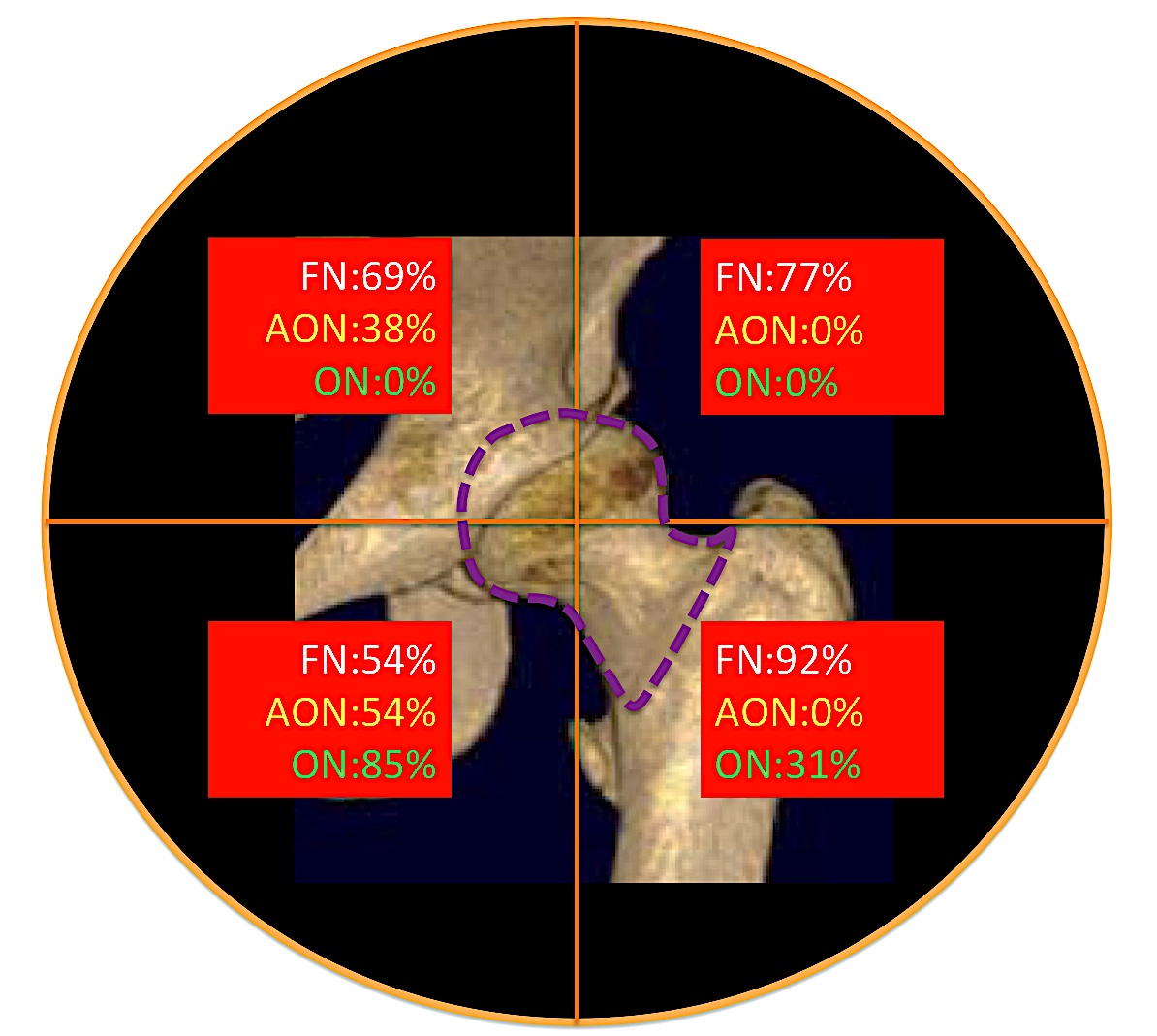
Reproduced with permission from Philip Peng Educational Series
Anatomy of the PENG Block
Anatomic structures pertinent for performing the PENG block include anterior superior iliac spine (ASIS), AIIS, pubis, and inguinal ligament. Two major muscles also help serve as identifying landmarks when performing this block under ultrasound guidance. The psoas major muscle starts at the lumbar vertebrae and inserts into the lesser trochanter of the femur. The iliacus originates at the wing of the ilium and attaches to the lesser trochanter. Both muscles function as major hip flexors and are commonly referred to as iliopsoas. The initial goal of the ultrasound guided PENG block is to obtain an ultrasound image aligning the AIIS and IPE (Figure 3). An optimal ultrasound scan should include the following structures: AIIS, IPE (bony prominence just medial to the psoas tendon), iliopsoas muscle and psoas tendon, and femoral neurovascular bundle.
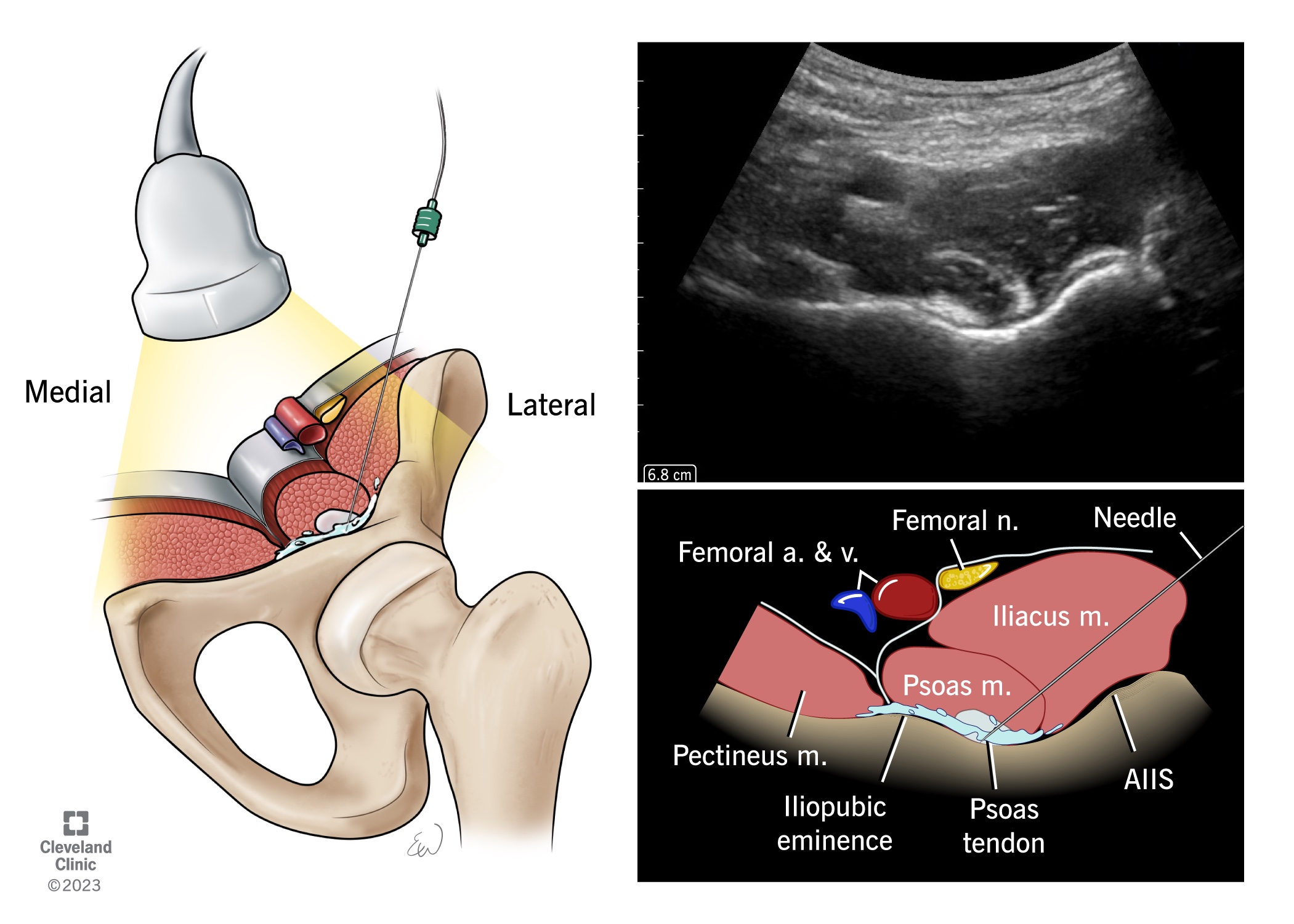
Figure 3. Left panel shows an illustration of the anatomical structures for the PENG block with left hemipelvis and proximal femur. The right panel shows the classic ultrasound image for the PENG block with illustration of the structures.
Reproduced with permission from Cleveland Clinic Centre for Medical Art & Photography
Supplies
- Low frequency curvilinear ultrasound probe (2-5 MHz)
- 80-100 mm, 20-22-gauge needle
- Sterile skin prep, sterile glove, mask, hat
- 15-20 mL of local anesthetic of choice
Approach, Technique, and Positioning
The PENG block is performed with the patient in the supine position. One can start the scanning by placing the probe at the ASIS in a transverse orientation and moving the ultrasound probe inferiorly to visualize the AIIS as per the original description by Giron et al.2 Once the AIIS is seen, the probe is pivoted towards the pubic symphysis to reveal the IPE. To ensure the optimal positioning of the probe over the two landmarks (AIIS and IPE), the depth of the AIIS is kept constant during the probe pivoting (Figure 4). The block is often performed as an in-plane technique directing the needle from lateral to medial. The needle tip should ultimately be guided to the fascial plane between the psoas tendon and ilium. Following negative aspiration, approximately 15-20 mL of local anesthetic of choice is injected, observing for fluid spread in this plane and displacement of the psoas muscle tendon.
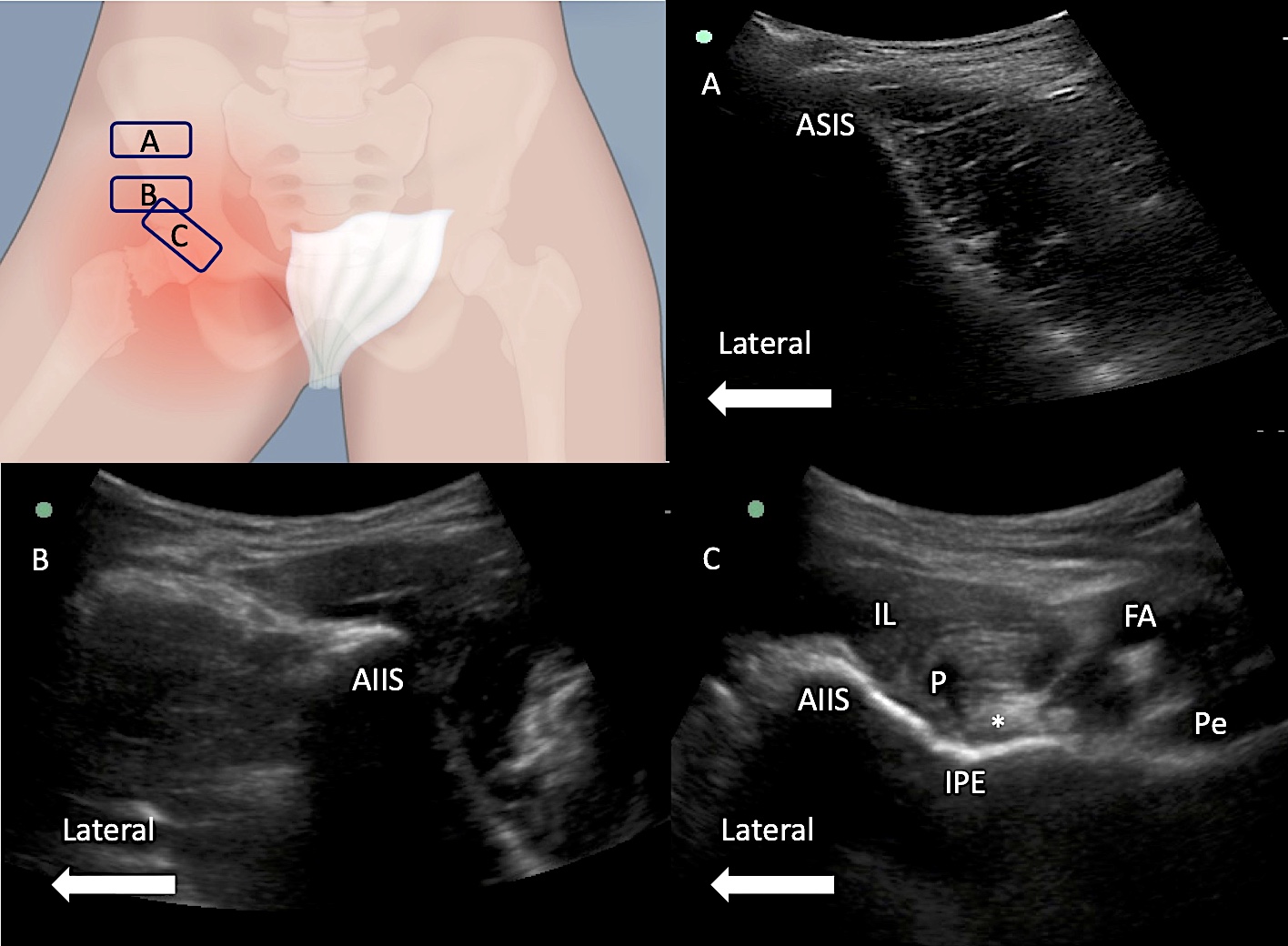
IL = iliacus, FA = femoral artery, P = Psoas, *= psoas tendo, Pe = pectineus.
Reproduced with permission from Philip Peng Educational Series
The needle tip should ultimately be guided to the fascial plane between the psoas tendon and ilium.
Two other possibilities can occur during injection: intramuscular spread or inability to inject due to high pressure. Rotating the needle will enhance the needle piercing through the muscle. Inability to inject is due to the needle being embedded in the iliofemoral ligament, and this can be solved by rotating the bevel 180 degrees or withdrawing the needle slightly. Deposition of local anesthetic in this plane will anesthetize the articular branches supplying the anterior hip capsule.
Other authors have described alternative approaches and scanning techniques, including bottom-up, visualizing the antero-superior joint line, and sliding up. The goal of any approach or technique used is to identify and target the fascial plane between the psoas tendon and ilium. Local anesthetic is then deposited in that fascial plane.
Discussion
Femoral nerve blocks, lumbar plexus blocks, and lumbar epidurals have been used in patients scheduled for hip fractures or total hip arthroplasties.5 However, a major disadvantage of these approaches is motor weakness, rendering patients unable to actively participate in physical therapy. Compared with the placebo, the PENG block showed superiority in post-operative analgesia effects and the level of opioid consumption in patients receiving both primary and revision total hip arthroplasty.6,7 Compared with femoral nerve block, the PENG block also showed superior post-operative analgesia effect and shorter discharge time in patients with hip fractures.8,9 Compared with infra-inguinal fascia iliaca block, the PENG block provided superior analgesia effects and decreased opioid consumption in patients after surgery for hip fractures.10 Compared with supra-inguinal fascia iliaca block, the PENG showed similar analgesia effects but lower incidence of motor blockade.11,12
As illustrated above, the PENG block aims to block articular nerve branches innervating the anterior hip capsule. This block therefore targets the anterior sensory branches and spares the motor branches and posterior proprioceptive fibers. Another major advantage of the PENG block is that it can be performed with the patient in a supine position, and significant reduction in dynamic hip pain can typically be achieved within 30 minutes of block placement. The motor-sparing effect enables patients to ambulate early, actively participate in physical therapy, and reduce opioid consumption.
The main indication for the PENG block is for post-operative analgesia following hip arthroplasty. There is evidence to support its use for acute traumatic pain after hip fracture. Other potential indications for the PENG block include chronic hip pain. Although the PENG block covers the anticipated pain from the anterior capsule and is theoretically an ideal analgesic block for hip arthroscopy, recent literature does not show any clinically relevant benefit. Contraindications to the PENG block include patient refusal, infection at the needle insertion site, and risk of bleeding for patients on anticoagulants.
Clinical Pearls
- Although the PENG block is motor sparing, use of large, local anesthetic volume (>20 mL) can cause greater spread and increase chances of anterior thigh weakness due to femoral nerve blockade. A large volume of local anesthesia can track through the junction between pectineus and psoas to the superficial surface of the psoas, resulting in motor block.13
- One of the major contributions for the motor block is the spread of local anesthesia in inadvertent intramuscular injection. Having a needle touching bone does not guarantee the needle is on the bone as the bone prevents the fascia to yield for the
needle to “pop” through. One way to get around this is to rotate the needle to simulate a piercing action on the fascia (Figure 5). Even though one can see the spread of injectate deep to the fascia, one should monitor and prevent
intramuscular spread. It is possible for a small volume of local anesthetic to track through a thin psoas muscle towards the femoral nerve.
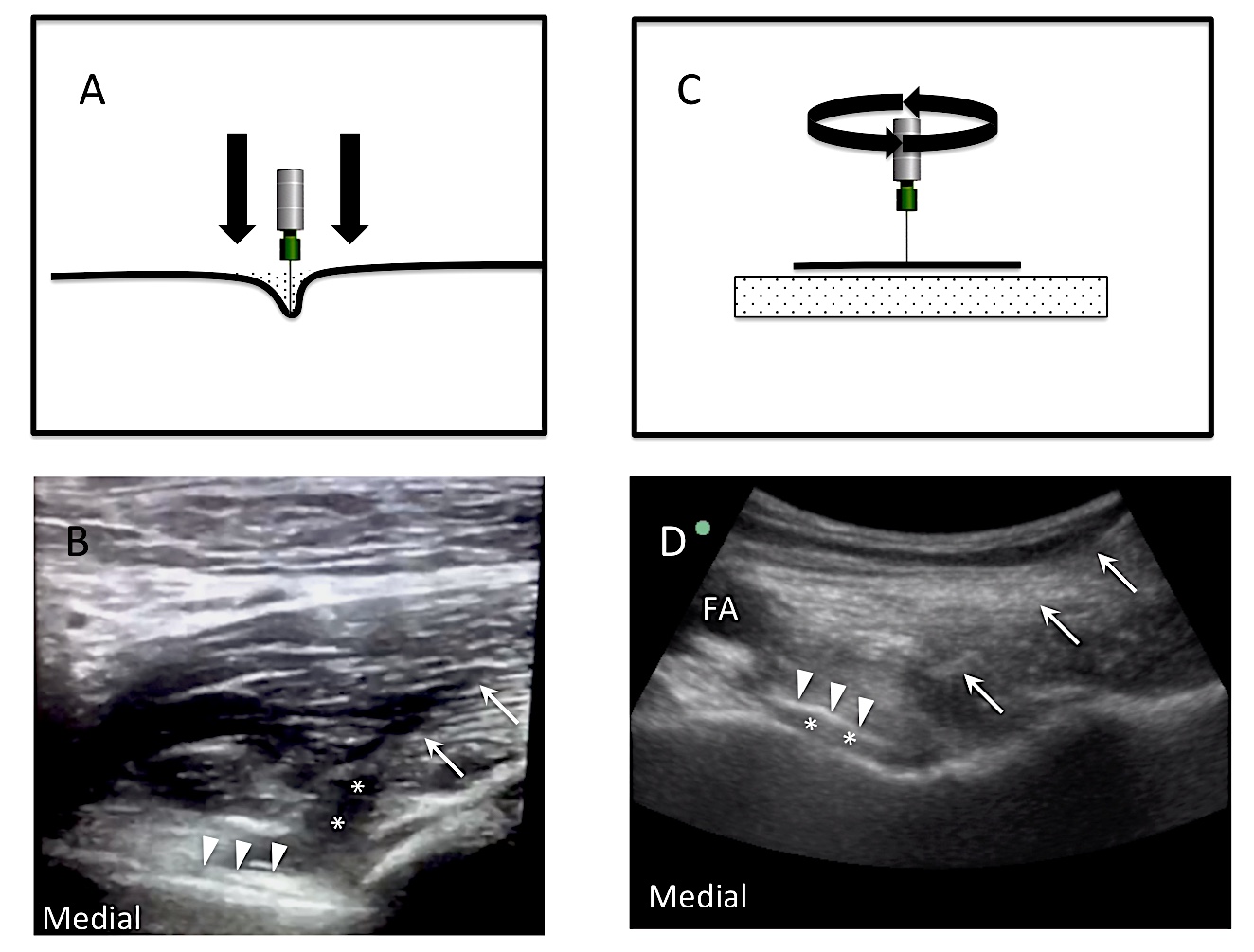
Figure 5. A: When a needle pierces through a fascia, it indents the fascia first, which yields eventually for the needle to pass through. B: When a needle (arrows) is inserted through the psoas muscle and touch the bone, it does not necessarily imply that the needle is “ON” the bone. It may not pierce the muscle fascia (arrowheads), and when local anesthetic is injected through the needle, it results in intramuscular spread (**). C: A schematic diagram to expand how it happens. Because the bone supports the fascia to prevent indentation, a needle touching bone does not mean the needle is on the bone. To pierce through the fascia, the authors suggest rotatory movement of the needle. D: When the needle (arrows) pierces through the fascia, the local anesthetic (**) will result in lifting of the psoas (arrowheads).
FA = femoral artery
Reproduced with permission from Philip Peng Educational Series. - In some situations, the clinician may find it hard to inject local anesthetic via the needle. It is likely that the needle tip is within the iliofemoral ligament especially if the needle tip position is closer to the hip capsule. Rotating the needle bevel 180 degrees should be the first step before slightly withdrawing the needle.
- Quite often, one may not see the “lifting” of the psoas due to either intramuscular placement or the cephalad placement of the needle (Figure 6: Position 2). There are a few ways to help to avoid this. First, when one pivots the probe
around the AIIS, make sure the depth is the same before and after the pivoting. Second, when the probe is in perfect position over the AIIS and IPE, the echogenicity of the bone is the highest. A cephalad placement can be easily recognized by
the decreased echogenicity of the bone (Figure 6: Position 2). Third, the most common reason for a needle placed cephalad is the tilting of the probe in cephalad direction due to the protuberant abdomen of the patient. This can be avoided by placing
a large pillow beneath the buttock on the side of the block. Alternatively, taping of the abdomen or the retracting of the abdomen by an assistant will help.
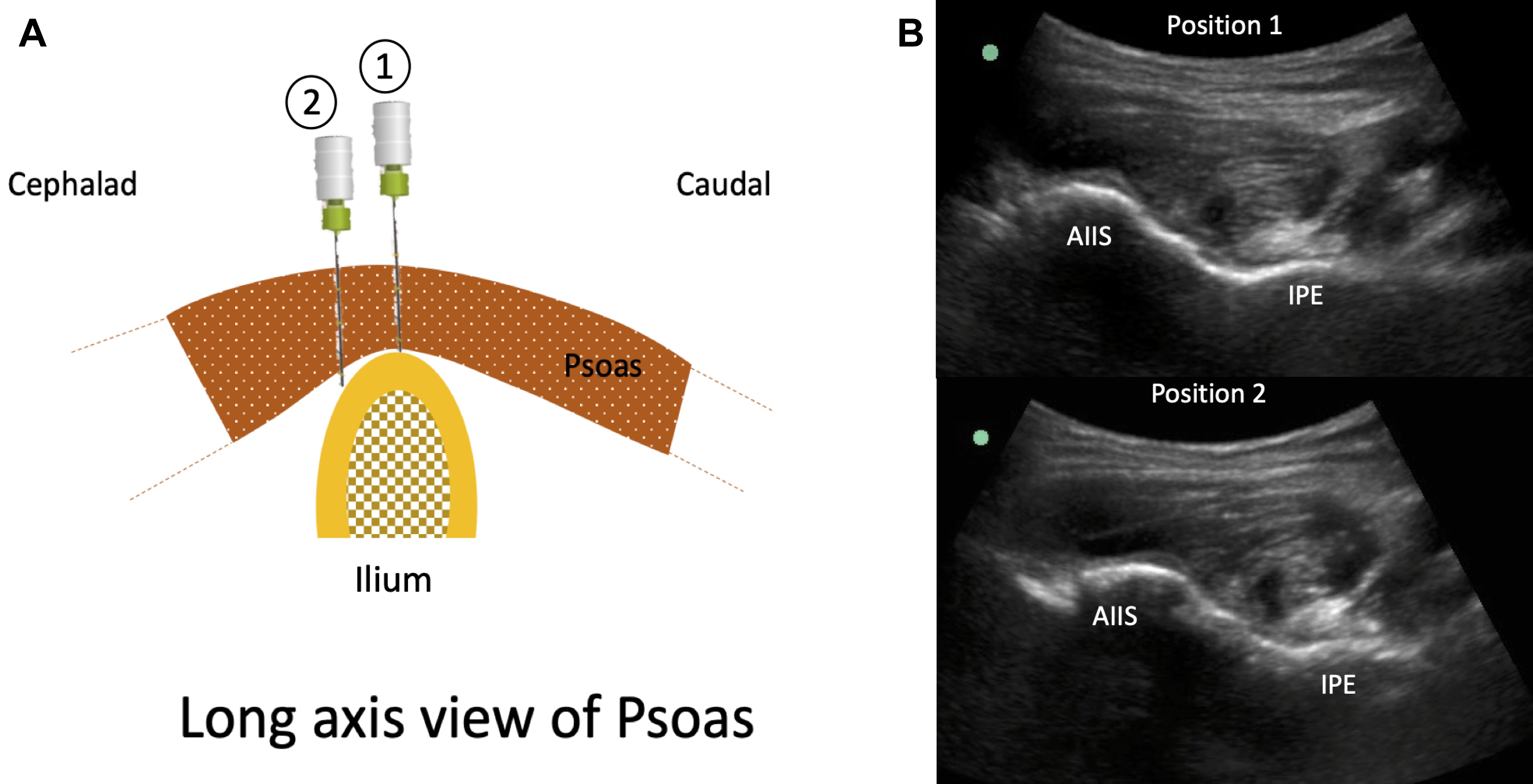
Figure 6. A: Shows illustration of the long axis view of the psoas over the ilium. When the needle is directed toward the anterior portion of the ilium (position 1), injection of local anesthetic will result in a psoas lift. When the needle tip position moves to a more cephalad location (position 2), psoas lift will not be seen in the sonograph. B: Ultrasound images of the ilium in positions 1 and 2. The more cephalad ultrasound position or needle position (position 2) is evident, but the decreased in the echogenicity of the ilium compared with that in position 1. AIIS = anterior inferior iliac spine, IPE = iliopubic eminence
Reproduced with permission from Philip Peng Educational Series. - An optimal scan should include the femoral artery as the femoral nerve is lateral to it. In some situations, the femoral nerve is close to the trajectory of the needle, and tilting of the probe laterally can increase the options of the trajectory
to avoid the femoral nerve (Figure 7).
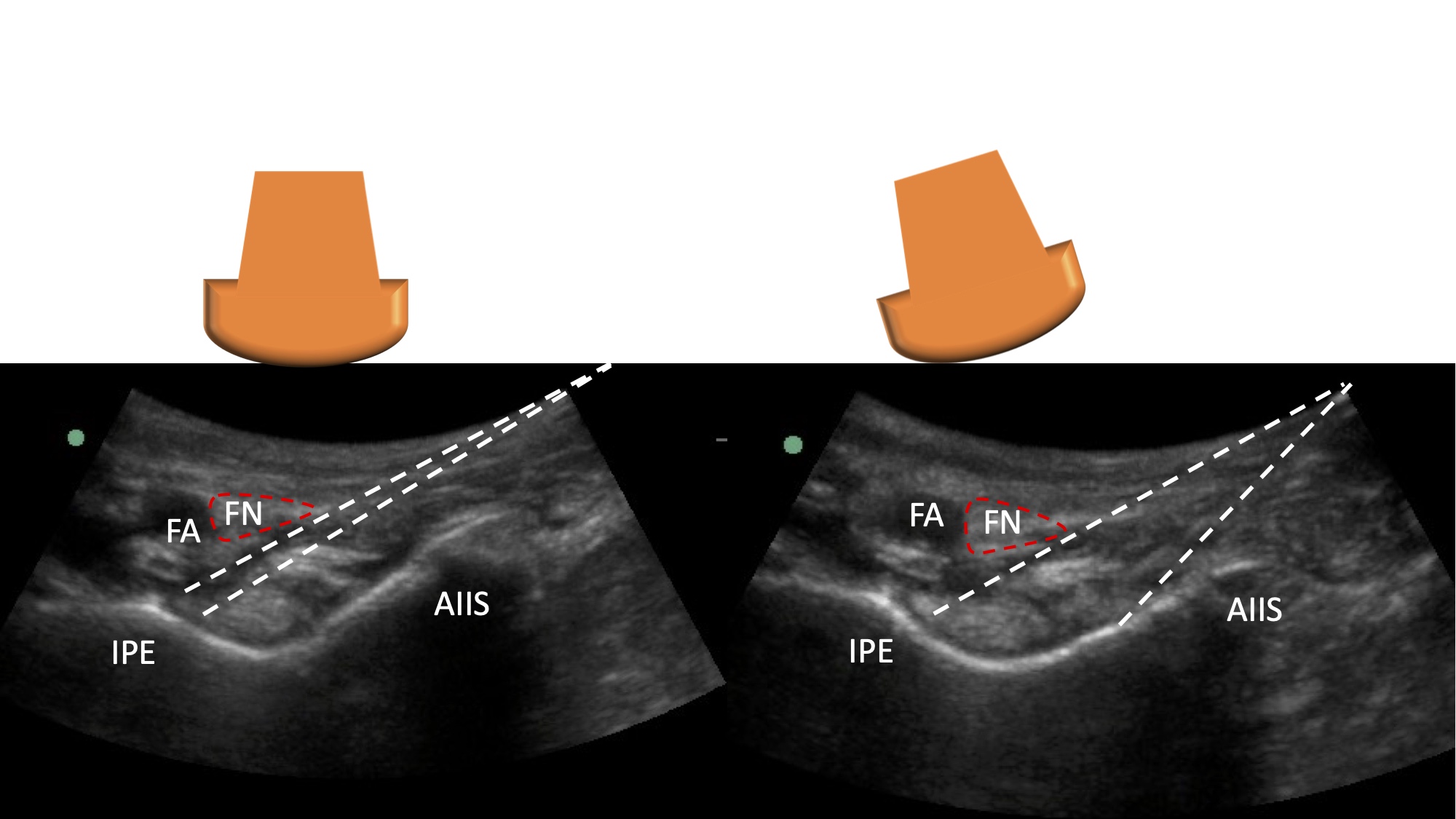
Figure 7. Optimization of the scan to avoid the needle path being too close to the femoral nerve. Left panel shows the range of the needle paths towards the target, which is close to the femoral nerve (FN). By toggling the ultrasound probe toward the lateral side, the possible range of needle paths increases, and one can avoid advancing the needle too close to the FN.
FA = femoral artery, AIIS = anterior inferior iliac spine, IPE = iliopubic eminence
Reproduced with permission from Philip Peng Educational Series. - The injection point for the PENG block is in the vicinity of the lateral femoral cutaneous nerve (Figure 8).14,15 To avoid injury to the nerve, the authors suggest paying attention to the patient when putting local infiltration to the skin
before needle insertion. If the patient complains of pain, we should inquire whether the pain is localized from the needle or radiates down the lateral thigh, suggesting a paresthesia of the lateral femoral cutaneous nerve. In the latter case,
the needle needs to be relocated.
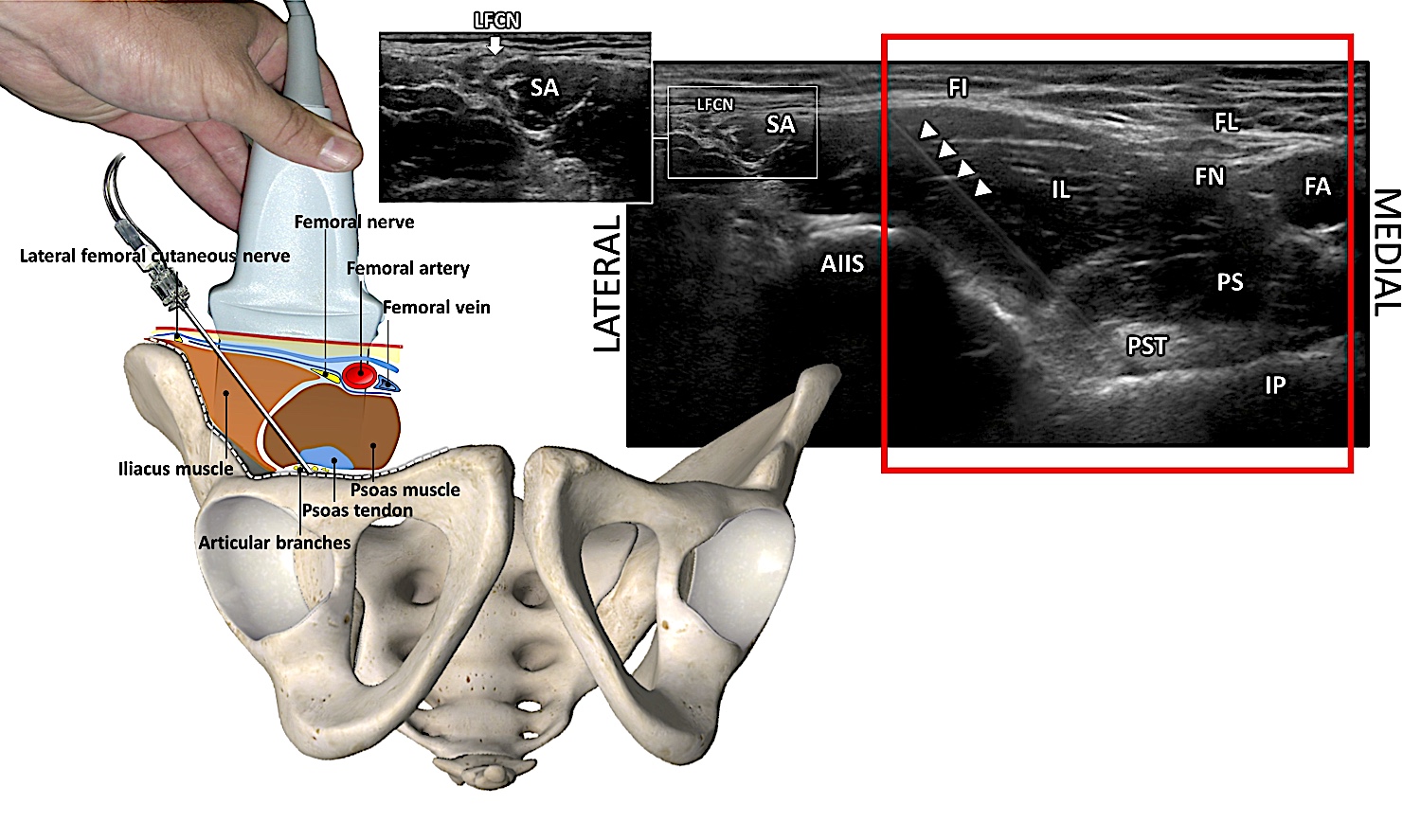
- Although a curvilinear ultrasound probe is often used to identify the iliopubic eminence, a high-frequency linear ultrasound probe (4-15 MHz) is more suitable for slender patients.
Figure 8. Extended field of view of the inguinal region for the PENG block. The sonograph shows the target for PENG block, which is the fascia plane deep to the psoas muscle/tendon between AIIS and IPE. The sonograph within the red rectangle is the image acquired with the linear probe as shown in the left diagram. However, the extended view also shows the proximity of the needle entry site to the lateral femoral cutaneous nerve, which lies in the fat-filled grove lateral to the sartorius as shown in the insert.
FL = fascia lata, FI = fascia iliaca, FN = femoral nerve, FA = femoral artery, PS = psoas muscle
Reprinted with permission from Imedar.com.
The illustration was created by Dr. Vicente Roques, and the sonograph was provided by Dr. Philip Peng.
Sree Kolli, MD, EDRA, is a clinical assistant professor in the Anesthesiology Institute at the Cleveland Clinic in Ohio.
Sindhuja R Nimma, MD, is an assistant professor in the department of anesthesiology and perioperative medicine at the Mayo Clinic in Jacksonville, FL.
Promil Kukreja, MD, PhD, FASA, is a professor in the department of anesthesiology and perioperative medicine at the University of Alabama in Birmingham.
Philip Peng, MBBS, FRCPC, Founder (Pain Medicine), is a professor in the department of anesthesiology and pain management for the University Health Network and Sinai Health Network at the University of Toronto in Canada.
References
- Maradit Kremers H, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 2015;97(17):1386-97. https://doi.org/10.2106/JBJS.N.01141
- Girón-Arango L, Peng PWH, Chin KJ, et al. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med 2018;43(8):859-63. https://doi.org/1097/AAP.0000000000000847
- Short AJ, Barnett JJG, Gofeld M, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med 2018;43(2):186-92. https://doi.org/10.1097/AAP.0000000000000701
- Tomlinson J, Zwirner J, Ondruschka B, et al. Innervation of the hip joint capsular complex: a systematic review of histological and immunohistochemical studies and their clinical implications for contemporary treatment strategies in total hip arthroplasty. PLoS One 2020;15(2):e0229128. https://doi.org/1371/journal.pone.0229128
- Guay J, Parker MJ, Griffiths R, et al. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev2017;5(5):CD001159. https://doi.org/10.1002/14651858.CD001159.pub2
- Pascarella G, Costa F, Del Buono R, et al. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: a randomised, observer-masked, controlled trial. Anaesthesia 2021;76(11):1492-98. https://doi.org/10.1111/anae.15536
- Kukreja P, Avila A, Northern T, et al. A retrospective case series of pericapsular nerve group (PENG) block for primary versus revision total hip arthroplasty analgesia. Cureus 2020;12(5):e8200. https://doi.org/10.7759/cureus.8200
- Lin DY, Morrison C, Brown B, et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: a single-center double-blinded randomized comparative trial. Reg Anesth Pain Med 2021;46(5):398-403. https://doi.org/10.1136/rapm-2020-102315
- Lin DY, Brown B, Morrison C, et al. Pericapsular nerve group block results in a longer analgesic effect and shorter time to discharge than femoral nerve block in patients after hip fracture surgery: a single-center double-blinded randomized trial. J Int Med Res 2022;50(3):3000605221085073. https://doi.org/10.1177/03000605221085073
- Mosaffa F, Taheri M, Manafi Rasi A, et al. Comparison of pericapsular nerve group (PENG) block with fascia iliaca compartment block (FICB) for pain control in hip fractures: a double-blind prospective randomized controlled clinical trial. Orthop Traumatol Surg Res 2022;108(1):103135. https://doi.org/10.1016/j.otsr.2021.103135
- Aliste J, Layera S, Bravo D, et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg Anesth Pain Med 2021;46(10):874-878. https://doi.org/10.1136/rapm-2021-102997
- Choi YS, Park KK, Lee B, et al. Pericapsular nerve group (PENG) block versus supra-inguinal fascia iliaca compartment block for total hip arthroplasty: a randomized clinical trial. J Pers Med 2022;12(3):408. https://doi.org/10.3390/jpm12030408
- Yeoh SR, Chou Y, Chan SM, et al. Pericapsular nerve group block and iliopsoas plane block: a scoping review of quadriceps weakness after two proclaimed motor-sparing hip blocks. Healthcare (Basel) 2022;10(8):1565. https://doi.org/
- Girón-Arango L, Roqués V, Peng P. Reply to Dr Roy et al: total postoperative analgesia for hip surgeries: PENG block with LFCN block. Reg Anesth Pain Med 2019;44:684-5. https://doi.org/10.1136/rapm-2019-100505
- Nanda M, Rojas A, Stander S, et al. Single-pass needle trajectory for lateral femoral cutaneous nerve and PENG blocks, and caution to avoid injury. Reg Anesth Pain Med 2022;rapm-2022-103782.https://doi.org/10.1136/rapm-2022-103782



