How I Do It: Epidural Electrical Stimulation (Tsui Test) for Thoracic Epidural Catheter Confirmation
Cite as: Kwofie K., Tsui B. How I do it: epidural electrical stimulation (tsui test) for thoracic epidural catheter confirmation. ASRA News. 2021;46. https://doi.org/10.52211/asra050121.029.
Background
Thoracic epidural catheter placement has long been viewed as the gold standard for postoperative analgesia following thoracic and abdominal surgeries. Unfortunately, the failure rate for thoracic epidural catheters can be as high as 30%.1,2 Placement failure can be due to a variety of factors. Technical failure may be caused by the inability to locate an interlaminar space. In addition, subcutaneous catheter placement following a “false loss” also may be a cause of analgesic
failure. A further etiology of epidural failure includes a catheter being cited at an inappropriate level and resulting inadequate analgesia or leg weakness.
A variety of techniques have been used to increase the success of thoracic epidural catheter placement (Table 1).3 These include:
- Real-time fluoroscopy
- Test dose of local anesthetic
- Epidural waveform analysis
- Epidural electrical stimulation test (Tsui test).
Table 1. Common Techniques for Thoracic Epidural Catheter Confirmation.
| Technique | Equipment | Improves Access to Epidural Space | Confirms Catheter In Epidural Space | Confirms Catheter Level |
| Real-time Fluoroscopy | · Image Intensifier · Lead Gowns · Shielded Location | Yes | Yes (Objective) | Yes (Objective) |
| Test Dose of Local Anesthetic | · None | No | Yes (Subjective) | Yes (Subjective) |
| Epidural Waveform Analysis | · Sterile Arterial Line Set · Monitor | No | Yes (Objective) | No |
| Pre-procedural Ultrasound | · Ultrasound | 1 RCT No Benefit | Only In Young Children | No |
| Epidural Electrical Stimulation Test (Tsui test). | · Johan Adapter · Nerve Stimulator | No | Yes (Objective) | Yes (Objective) |
Each of these approaches has its own merits and drawbacks.
Fluoroscopy with a contrast epidurogram offers the gold standard for technical guidance in locating the interlaminar space, confirmation of injectate/catheter in the epidural space, and identification of the vertebral level of the catheter tip. Unfortunately,
the required equipment is bulky, expensive, not widely available, and practically challenging (eg, non-shielded block rooms), and interventional fluoroscopy training is not universal in anesthesia residency. Therefore, despite being widely adopted
in an interventional/chronic pain management setting, fluoroscopy is not a common practice in acute pain management settings for thoracic epidural placement or catheter confirmation. Though simple and cost-effective, a test dose comprised of local
anesthetic and epinephrine can be time consuming, subjective, influenced by a patient’s current medication regimen, and occasionally associated with hemodynamic perturbations. Epidural wave form analysis allows for an objective assessment of
catheter placement in the epidural space; however, it requires significant equipment preparation and material waste. The latter two techniques do not offer information on the vertebral level of the catheter.
The epidural electrical stimulation test was first described more than 20 years ago.4 During the test, an electrical current is conducted through a column of saline and a standard wire reinforced catheter.5 This test has a sensitivity
and specificity of 80-100% to 91.6-100%, respective of confirming epidural placement within the epidural space.4,6
The epidural electrical stimulating test not only allows for objective assessment of the correct catheter placement in the epidural space but also confirmation of the vertebral level of the catheter tip. This method of epidural catheter placement confirmation
is simple to use and interpret, effective, and efficient. A disadvantage of the Tsui test is that, unlike fluoroscopy, it is not a tool that allows for visualization of spinal anatomy nor assistance with access to the epidural space. Though it is
possible to use epidural electrical stimulation for lumbar epidurals, we generally limit the use of electrical stimulation for thoracic epidural placement. Nonetheless, in the pediatric population, an epidural catheter can be inserted from the caudal
space and advanced in a cephalad direction within the epidural space to the desired vertebral level under direct guidance of the epidural stimulation test.7
The epidural stimulation test provides valuable objective information that aids in the assessment of catheter placement. Potential rationale for increased incorporation and utilization of the Tsui test include the following.
- The described failure rate of epidural catheter placement in the literature can be significant.1,2
- When less experienced trainees perform an epidural, a subjective loss of resistance may be less reliable than in more seasoned hands.
- The clinician who is taking care of the patient on the acute pain service postoperatively may be different than the practitioner inserting the epidural and, therefore, may not be aware of the confidence with which the epidural space was accessed.
- For many practitioners, the first opportunity to objectively assess the success of the procedure is the patients comfort level in the post-anesthesia care unit (PACU), which does not typically allow an easy opportunity for re-siting of a poorly functioning
epidural catheter. This is particularly problematic if a patient has received anticoagulation intraoperatively.
Equipment
The equipment required for the Tsui test includes the following (Figure 1).
- Standard epidural kit with a typical wire reinforced catheter
- Nerve stimulator that can deliver current to at least 15mA
- Johan adapter
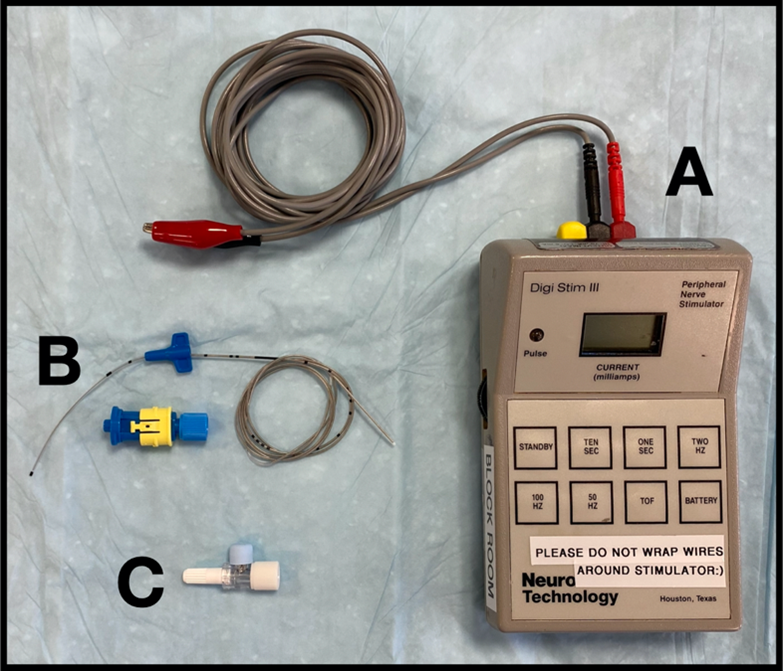
Figure 1: Equipment for Tsui Test. (A) Nerve Stimulator, (B) Standard Wire-Reinforced Epidural Catheter, (C) Johan Adapter.
Many anesthesiologists may not be familiar with the Johan adapter.8 It consists of a short lumen with a male and female luer-lock connector on either end, respectively. In the center of the lumen there is a metallic pin which is used to connect an alligator clip and conduct an electrical signal from the alligator clip to a column of fluid in the lumen of the adapter. There is a removable protective cover on the metallic pin (Figure 2). Though originally described for intravascular electrocardiography, the Johan adapter allows an electrical current to be conducted through a column of saline to neural structures and culminate in an observable evoked motor response.8
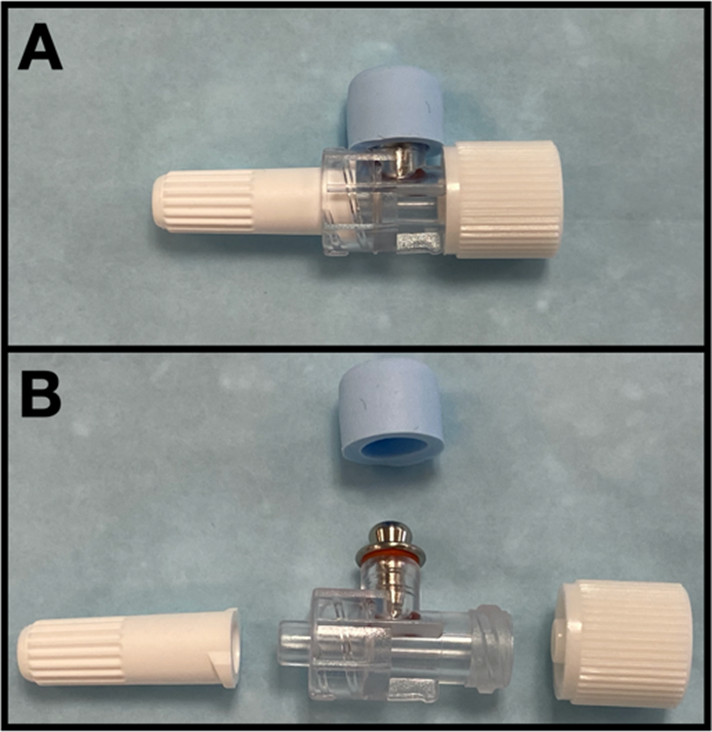
Figure 2: Johan Adapter, with lumen and hub guards (A) attached and (B) removed.
Some have commented on the “need to set up special equipment,”9 however, at Dalhousie University shared regional anesthesia carts in the operating room core contain Johan’s adapters, nerve stimulators, and necessary epidural
equipment, which are transported easily to the operating room when catheters are placed. In addition, our anesthesia technologists are trained to assist anesthesiologists with the technique. This test is commonly performed at our institutions, we
do not find the equipment cumbersome, and the test takes less than 60 seconds to set up, perform, and interpret in most cases.
Any commonly used, wire-reinforced uni-port or multiport epidural catheter is suitable for the test; a stimulating epidural catheter is NOT required.10 Non-reinforced catheters create a higher impedance, preventing stimulation, and should not
be used. The continual column of normal saline in the catheter and the epidural space forms a medium that allows for conduction of the electrical current.
The nerve stimulator must have an adjustable current clearly displayed. The typical stimulator settings used are a pulse width of 0.1 msec with a frequency of 1 Hz. However, using a higher-pulse width, up to 1.0 msec, will decrease the minimum current
necessary to achieve an evoked motor response. A nerve stimulator with a maximum voltage of < 400 V may not be able to stimulate at currents above 5 mA.11
Thoracic Epidural and Testing Procedure
After landmarking to determine the site of needle entry, sterile preparation, and local infiltration of the skin, the epidural space is accessed using a loss-of-resistance technique. We usually use a loss-of-resistance to saline rather than air, as the
presence of air within the epidural space might impede the ability to elicit an evoked motor response during stimulation. After the wire-reinforced catheter is advanced into the epidural space, the Tuohy needle is removed. The epidural catheter is
then withdrawn to the desired depth, and the Luer lock adapter is attached to the epidural catheter. The Luer lock allows the Johan adapter to be attached, and a sterile syringe of normal saline is attached to the other end of the Johan adapter such
that the epidural catheter can be flushed to prevent any air bubbles within the system. This is a critical step because any air bubbles in the catheter will increase the impedance and prevent effective stimulation through the catheter. The rubber
cover on the Johan adapter is removed from the metallic conductor, and the cathode (positive) lead of the nerve stimulator is attached to the metallic connector. The anode (negative) lead of the nerve stimulator is placed on the patient’s lateral
thigh.
The nerve stimulator is set to a frequency of 1 Hz and a pulse width of 0.1 msec. The current is increased incrementally until the patient has a sensory response. Then the current is further increased slowly (usually by 1-2mA) until a visible or palpated
evoked motor response is observed or palpated. Gentle continuous pressure on the syringe of saline while attempting to elicit an evoked motor response will compress any small air bubbles that may be inadvertently present in the adapter or catheter.
It is important to note that a catheter that is positioned intrathecally, subdurally, or near a spinal root will result in a more brisk and low current responses, therefore, it is prudent to start at a low current and increase very gradually. The
nerve stimulator is then removed from the Johan adapter, and the epidural catheter is secured to the patient in the usual fashion.
In addition to the standard epidural procedural documentation, we would also recommend documenting the following.
- Minimum current for the evoked motor response
- Laterality of the evoked motor response
- Dermatomal level of the evoked motor response
Interpretation of the Epidural Stimulation Response
An observable unilateral-evoked motor response with a current of 1 to 15 mA is typical of a catheter correctly positioned within the epidural space; the level of the observed motor response corresponds to the level of the catheter tip.12 Though
the initial description of the technique suggested a pulse width of 0.2 msec and a current range of 1-10 mA, it has been suggested that the range of acceptable currents should be increased.4,8,13 The use of larger pulse width up to 1.0
msec leads to a decrease in the minimum current required to elicit the same evoked motor response.11
Many other characteristic stimulation patterns can be seen (Table 2). An evoked motor response that is bilateral with minimum current < 1 mA is typical of an intrathecal catheter. This should have an aspiration test and may need to be replaced.6 A low-current motor response (< 1mA) with a multi-segmental distribution is typical of a subdural catheter.14 A catheter with a unilateral evoked motor response with a stimulating current < 1 mA may be within a nerve root sheath and may need to be withdrawn slightly.4
Table 2: Typical Pattern of Evoked Motor Responses
| Catheter Location | Motor Response | Minimum Current |
| Epidural | Unilateral | 1-15 mA |
| Nerve Root | Unilateral | < 1 mA |
| Subcutaneous | No Response or Unilateral > 15 mA | > 15 mA |
| Subdural | Multi-segmental | < 1 mA |
| Intrathecal (Spinal) | Strong Response Bilateral | < 1 mA |
Although it is often possible to stimulate a well-positioned epidural catheter after local anesthetic has been administered, this generally increases the minimum current required to generate an evoked motor response and may completely prevent an evoked
motor response altogether.15 A catheter that is intravascular may initially stimulate similar to the characteristics of a well-positioned epidural catheter, but the minimum current required will be unaffected by a test bolus of local anesthetic.
16
Conclusion
In conclusion, the Epidural Electrical Stimulation Test (Tsui Test) is an objective, effective, and efficient technique to confirm the position and vertebral level of epidural catheter tips. It requires minimal equipment and is quick to perform. This test ensures the accuracy of epidural catheter placement, especially in the context of thoracic epidural placement for postoperative analgesia for major surgery.
Kwesi Kwofie, MD, FRCPC, is an associate professor in the department of anesthesia, perioperative medicine and pain management at Dalhousie University in Halifax, Canada.
Ban Tsui, MD, MSc, FRCPC, is a professor in the department of anesthesiology, perioperative and pain medicine at Stanford University in California.
References
- Ready LB. Acute pain: Lessons learned from 25,000 patients. Reg Anesth Pain Med. 1999;24(6):499-505. https://doi.org/10.1016/S1098-7339(99)90038-X.
- Tran DQ, Van Zundert TC, Aliste J, Engsusophon P, Finlayson RJ. Primary failure of thoracic epidural analgesia in training centers: The invisible elephant? Reg Anesth Pain Med. 2016;41(3): 309-313. http://doi.org/10.1097/aap.0000000000000394
- Elsharkawy H, Sonny A, Chin KJ. Localization of epidural space: A review of available technologies. J Anaesthesiol Clin Pharmacol. 2017;33(1):16-27. http://dx.doi.org/10.4103/0970-9185.202184.
- Tsui BC, Gupta S, Finucane B. Confirmation of epidural catheter placement using nerve stimulation. Can J Anaesth. 1998;45(7):640-644. https://doi.org/10.1213/01.ANE.0000080609.05942.38.
- Tsui BC, Sze CK. An in vitro comparison of the electrical conducting properties of multiport versus single-port epidural catheters for the epidural stimulation test. Anesth Analg. 2005;101(5):1528-1530. https://doi.org/10.1213/01.ANE.0000181006.36917.3E.
- de Medicis E, Tetrault JP, Martin R, Robichaud R, Laroche L. A prospective comparative study of two indirect methods for confirming the localization of an epidural catheter for postoperative analgesia. Anesth Analg. 2005;101(6):1830-1833. https://doi.org/10.1213/01.ANE.0000184130.73634.BE.
- Tsui BC, Wagner A, Cave D, Kearney R. Thoracic and lumbar epidural analgesia via the caudal approach using electrical stimulation guidance in pediatric patients: a review of 289 patients. Anesthesiology. 2004 Mar;100(3):683-9. https://doi.org/10.1097/00000542-200403000-00032.
- Wood Library Museum of Anesthesiology. Johans adapter. Available at: https://www.woodlibrarymuseum.org/museum/johans-adapter/. Accessed November 20, 2020.
- Abdallah FW, Chan VW. From the journal archives: Practical applicability of the epidural electrical stimulation test. Can J Anaesth. 2014;61(9):881-885. https://doi.org/10.1007/s12630-014-0145-6.
- Patel R, Arzola C, Petrounevitch V, Balki M, Downey K, Tsui BC, Carvalho JC. Response patterns to the electric stimulation of epidural catheters in pregnant women: a randomized controlled trial of uniport versus multiport catheters. Anesth Analg. 2016;123(4):950-954. https://doi.org/10.1213/ANE.0000000000001236.
- Tsui BC, Tsui JH, Corry GN. Estimation of equivalent threshold currents using different pulse widths for the epidural stimulation test in a porcine model. Can J Anaesth. 2014;61(3):249-253. https://doi.org/10.1007/s12630-013-0096-3.
- Tsui BC, Guenther C, Emery D, Finucane B. Determining epidural catheter location using nerve stimulation with radiological confirmation. Reg Anesth Pain Med. 2000;25(3):306-309. https://doi.org/10.1016/s1098-7339(00)90017-8.
- Sutherland MA, Viscomi CM, Dominick TS, Anderson EL. Minimum current requirements for epidural stimulation test confirmation of epidural and intrathecal catheter placement. Reg Anesth Pain Med. 2009;34(6):575-577. https://doi.org/10.1097/aap.0b013e3181bfbe1e.
- Lena P, Martin R. Subdural placement of an epidural catheter detected by nerve stimulation. Can J Anaesth. 2005;52(6):618-621. https://doi.org/10.1007/BF03015772.
- Förster JG, Niemi TT, Salmenperä MT, Ikonen S, Rosenberg PH. An evaluation of the epidural catheter position by epidural nerve stimulation in conjunction with continuous epidural analgesia in adult surgical patients. Anesth Analg. 2009;108(1):351-358. https://doi.org/10.1213/ane.0b013e31818d0392.
- Tsui BC, Gupta S, Finucane B. Detection of subarachnoid and intravascular epidural catheter placement. Can J Anaesth. 1999;46(7):675-678. https://doi.org/10.1007/BF03013957.


Leave a commentOrder by
Newest on top Oldest on top