How I Do It: The Oblique “Scotty Dog” Approach to the S1 Transforaminal Epidural Injection
Cite as: Gogna M., Ahmed M. How I do it: the oblique “scotty dog” approach to the S1 transforaminal epidural injection. ASRA News. 2021;46. https://doi.org/10.52211/asra050121.027.
Introduction
Chronic low back pain (LBP) is highly prevalent and a significant economic burden to our society. Fluoroscopically guided transforaminal epidural steroid injection (TFESI) is an interventional procedure that is effective against radicular pain due to conditions like herniated intervertebral disc, spinal stenosis, and failed back surgery syndrome. Often the radicular pain arises from a herniated intervertebral disc causing mechanical or chemical irritation of the nerve root leading to its inflammation.1 It is postulated that the application of medications directly onto the nerve root(s) using the transforaminal approach permits maximum concentration of medications delivered to the site of suspected pathology compared to less direct approaches (ie, interlaminar or caudal). 2
Approach to transforaminal injections varies based on region of the spine, with regional variations in vertebral, vascular, and neural elements influencing desired placement of the needle and final location of the needle tip. Multiplanar fluoroscopic
guidance with the use of contrast dye to verify the trajectory and confirm the location of the needle tip is necessary prior to injecting particulate/non-particulate steroid. Digital subtraction angiography (DSA) is the reference standard for detecting
cases of inadvertent vascular access prior to injection, with one study showing that real-time fluoroscopy has a sensitivity of 71%.3
The anteroposterior approach to S1 transforaminal epidural steroid injection has been the most common technique; however, it is not necessarily the safest or the most productive. Fish et al. reported that using the S1 “Scotty dog” image as
a bony anatomic landmark to guide the needle toward the S1 foramen, not in the classic way but in an oblique (and usually caudal tilted) fluoroscopic view, during performance of L5 and S1 transforaminal epidural steroid injection, can save procedure
time and reduce the risk of radiation exposure.4 Moreover, in a study comparing the anteroposterior vs oblique techniques, Kim et al. found the incidence of intravascular injections, as determined through real-time fluoroscopy with the
DSA method during S1 transforaminal epidural steroid injection in the oblique view, was significantly lower than that in the anteroposterior view (29% vs. 11%).5
Case Report
A 50-year old female presented suffering from morbid obesity, diabetes mellitus, asthma, and lumbosacral radicular pain syndrome. She has been experiencing the pain for few years and failed numerous conservative therapies. She described the pain as an
electric shooting pain down her right lower extremity in the distribution of right L5 and S1 dermatomes. She states the pain has greatly limited her daily activities. Clinical examination is remarkable for right L5 and S1 radiculopathy. She reports
her preprocedure visual analog pain score as a 7/10. The standard AP S1 view was extremely difficult to obtain, so an S1 oblique view was obtained to perform the procedure as described below. A L5 TFESI was performed in a standard Scotty dog shadow
oblique view using the subpedicular approach.
Five minutes following the injection, the patient had very clear dermatomal analgesia involving L5 and S1 nerve root. She noted much improvement in her pain levels (0/10) and was pleased with improvement in her overall functional status.
Description of the Technique of S1 Lateral Approach
After obtaining informed consent, the patient is placed in the prone position. Pillows are placed under the abdomen to reduce lumbar lordosis. The patient is then prepped and draped using sterile technique.
Caudal tilt is adjusted to line up the L5-S1 endplate in anteroposterior view using a fluoroscope.
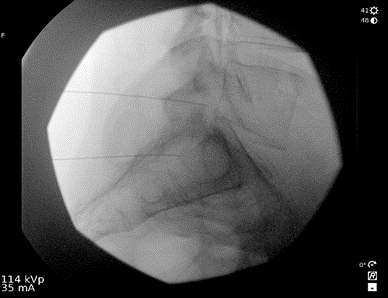
Furthermore, by cephalic or caudal tilt, the lower endplate of L5 is aligned parallel to the upper endplate of the sacrum in an anteroposterior projection. To obtain the Scotty dog (Figure 1 and 2) appearance at the L5 vertebral segment – the fluoroscope is rotated in an ipsilateral, oblique fashion (which in this case was right oblique). Once the appearance of a Scotty dog at L5 is obtained, the dog’s neck and forelimb (superomedial landmarks of the S1 foramen) are identified at the S1 segment. (Figure 2) The superior articular process of the S1 represents the ear of a S1 dog. If trouble in visualizing a Scotty dog at the S1 vertebral segment is encountered, the tilt can be adjusted slightly and the angle of oblique projection modified if needed. If the iliac crest is in your way, the needle pass can be cleared by adjusting the caudal tilt.
 | 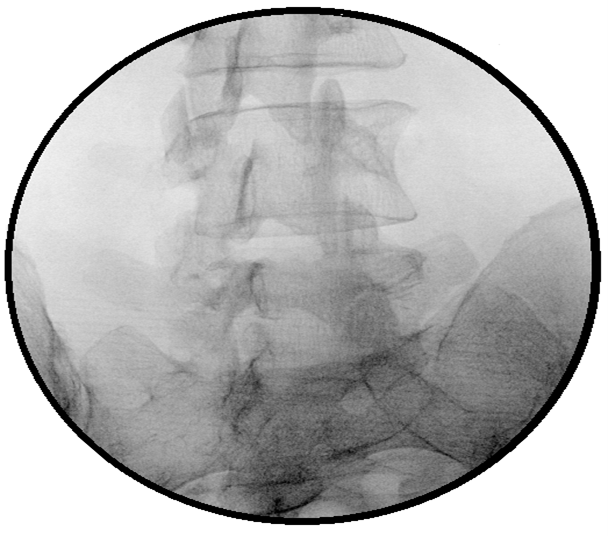 |
Figure 1. The oblique ‘Scotty dog’ formation view approach for S1 transforaminal injection and the corresponding position of the C-arm.
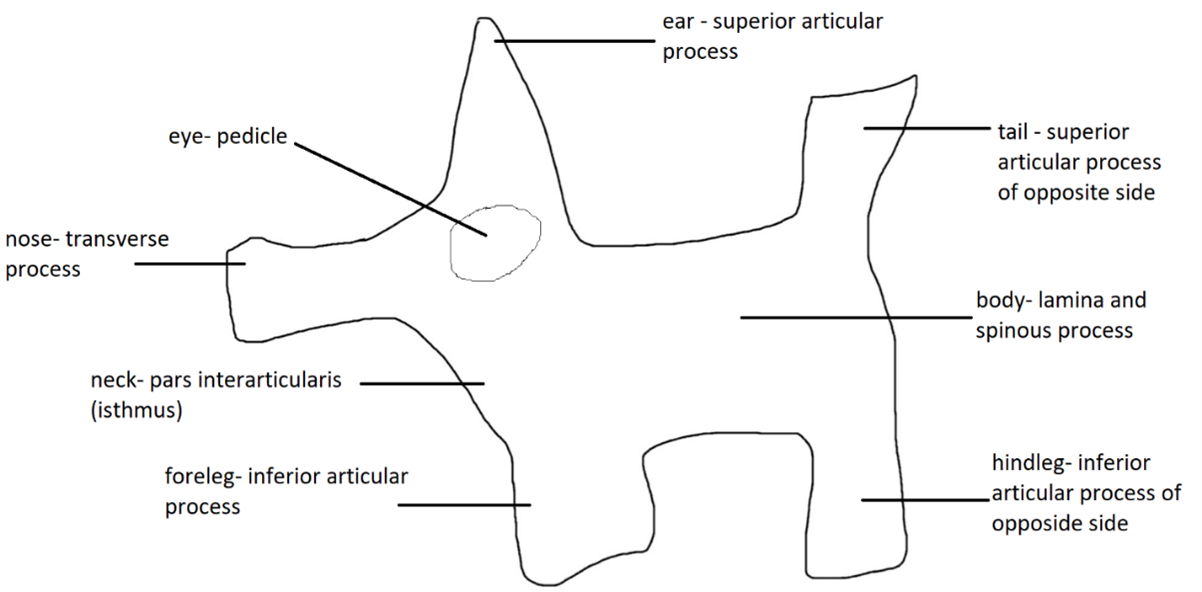
Figure 2. Different parts of the Scotty dog.
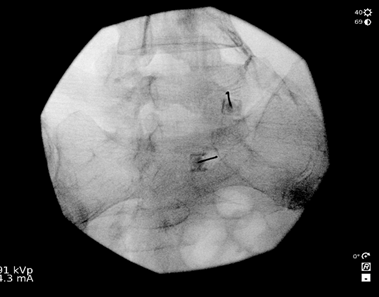
Lidocaine 1% (3 mL) is injected at the skin entry point – the target (ie, neck of Scotty dog at S1), after which a 22-G, 7-cm Quincke spinal needle is advanced under fluoroscopic guidance toward S1 neural foramen. To confirm that the needle tip at the sacral canal is at the perfect depth, a lateral image is obtained (Figure 3), and the needle is repositioned as appropriate. The lateral view allows one to verify the needle depth to make sure the needle tip is not too far ventral. The needle tip should not be advanced to the floor of the sacral canal. It should not exit the ventral S1 foramen. After obtaining the image, the procedure is continued, similar to a transforaminal epidural steroid injection in the anteroposterior view. Following negative aspiration for blood and cerebral spinal fluid and after confirming absence of paresthesia, nonionic contrast is injected, after which the therapeutic agents (ie, preservative-free bupivacaine 0.25% 2mL and dexamethasone 10mg/mL 1mL were given. (Figure 4) In this case, right L5 and S1 were done simultaneously in the same Scotty dog oblique view and the depth adjusted in the lateral view using the same amount of nonionic contrast and therapeutic agent as well.
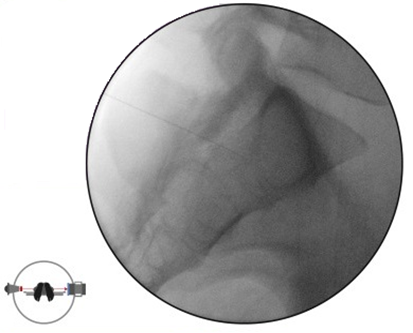
Figure 3. Lateral fluoroscopic image of the right S1 transforaminal injection and corresponding position of the C-arm.
 |  |
 | 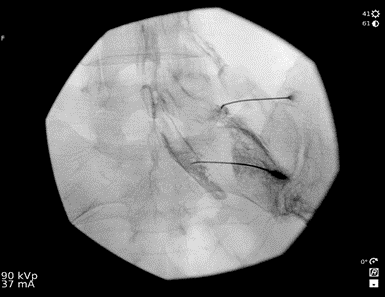 |
Figure 4. The final needle position in oblique view for right L5 and S1 transforaminal injection and the corresponding position of the C-arm.
Conclusion
The oblique approach to S1 transforaminal epidural steroid injection provides a safe, productive, and predictable alternative to the traditional anteroposterior approach. The oblique view can be effectively used to guide the needle tip into the S1 foramen as well as to the L5 foramen, which reduces the amount radiation exposure. This is an advantage not provided by the traditional anteroposterior approach, in which separate views must be obtained to advance the S1 needle and the L5 needle.
Mayank Gogna, MD, is a CA-1/PGY2, in the department of anesthesiology at the University of Texas Health Science Center at Houston McGovern Medical School.

Moustafa Ahmed, MD, is an assistant professor of anesthesia and critical care and director of the Chronic Pain Division at The University of Texas Health Science Center at Houston McGovern Medical School.

References
- Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013;38:175–200. https://doi.org/10.1097/AAP.0b013e31828ea086.
- Desai MJ, Shah B, Sayal PK. Epidural contrast flow patterns of transforaminal epidural steroid injections stratified by commonly used final needle-tip position. Pain Med. 2011;12:864–70. https://doi.org/10.1111/j.1526-4637.2011.01119.x.
- Hong JH, Huh B, Shin HH. Comparison between digital subtraction angiography and real-time fluoroscopy to detect intravascular injection during lumbar transforaminal epidural injections. Reg Anesth Pain Med. 2014;39:329–32. https://doi.org/10.1097/AAP.0000000000000096.
- Fish DE, Lee PC, Marcus DB. The S1 ‘‘Scotty Dog’’: report of a technique for S1 transforaminal epidural steroid injection. Arch Phys Med Rehabil. 2007;88:1730–3. https://doi.org/10.1016/j.apmr.2007.07.041.
- Kim D‐H., Yoon DM, Yoon KB. Incidence of intravascular injection and the spread of contrast media during s1 transforaminal epidural steroid injection by two approaches: anteroposterior vs oblique.” Anaesthesia. 2015;70(8):975–84. https://doi.org/10.1111/anae.13079.
Leave a commentOrder by
Newest on top Oldest on top