How I Do It: Introducing Procedural Simulation into Pain Fellowship
Cite as: Elmofty DH. How I do it: introducing procedural simulation into pain fellowship. ASRA News. 2021;46. https://doi.org/10.52211/asra050121.025.
For centuries, medical education was based on the Halstedian Method, an apprenticeship training model that basically consisted of high-volume, hands-on training with graduated levels of supervision.1 In this day and age, this method is
becoming obsolete due to the decrease in duty hours and procedural volume for trainees. Two decades ago, the Institute of Medicine published its report To Err Is Human: Building a Safer Health System.2 It reported that approximately
98,000 people die per year from medical errors that occur in hospitals. This resulted in an increased awareness and call to attention for safer healthcare practice, improving teamwork, and a method to ensure the learner can show how to apply in a
controlled setting before performing in real life.
Several subspecialties have integrated simulation-based training for technical and non-technical skills acquisition into the educational curricula. The driving force is patient safety, shorter learning curves, and improved efficiency. Implementing simulation into the curricula consists curriculum development and framework for design.3,4 The fundamental principles of curriculum development have been described as a six-step approach6 (figure 1). The steps are not linear but interactive.
Figure 1: Six-step approach to curriculum development in medical education.
Step 1: Problem Identification
What problem will your simulation address? To identify the problem, you need to define the current approach, then determine the ideal approach. The gap between the ideal and current approach becomes your problem. This step will ground the simulation curriculum and determine the needs of the learner.
Ideal Approach – Current Approach = Gap Analysis
Achieving competency in procedural skills is vital in interventional pain management. Assessing competency in procedural skills poses a unique challenge because it is difficult to standardize the measurement of procedural mastery. We currently lack an approach to assess different aspects of neuromodulation skills during fellowship training.
Step 2: Target Needs Assessment
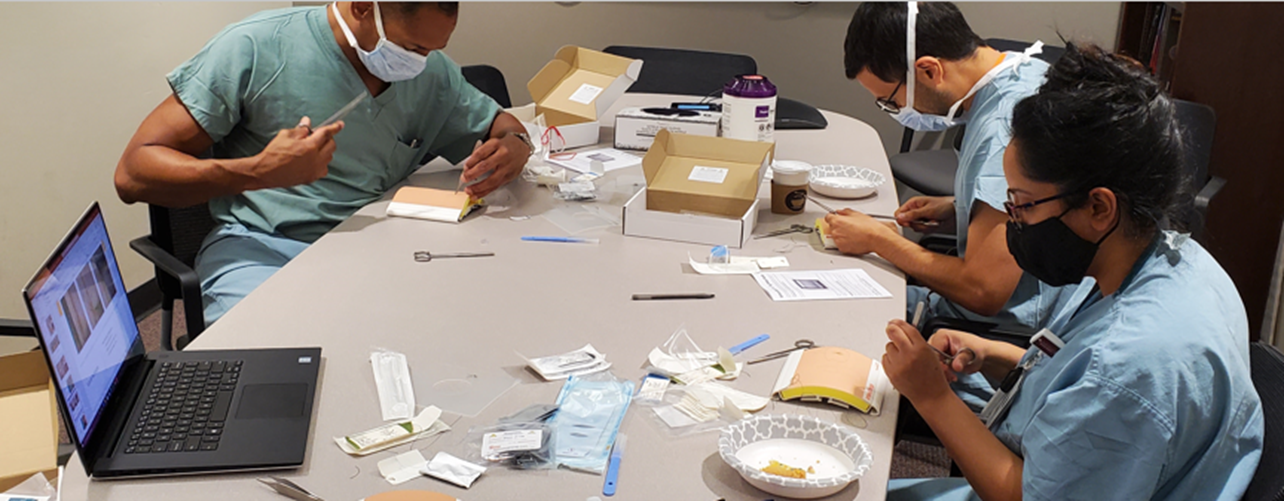
This step is intended to define the role of the simulation training within the overall curriculum. Who is the learner? What do the learners need to know, and how will they learn this target? We realized that a majority of our pain fellows struggle with basic surgical skills at the start of fellowship training and decided to introduce a workshop to help develop foundational skills (figure 2) prior to real-life patient encounters.
Figure 2: Surgical skills workshop.
Step 3: Goals & Objectives
Develop general goals as well as specific measurable objectives that will direct the educational content of your simulation. Goals should be broad in nature and strategic. Ask yourself what is the overall purpose of your simulation?
To develop well-written objectives, many will use the SMART approach.7 Developing objectives requires a clear picture of the results expected from program activities. The more specific your objectives are, the easier it will be to demonstrate success. SMART is a mnemonic acronym with each letter giving criteria for setting objectives.
- Specific: The specific part of an objective tells us what will change and for whom it will change.
- Measurable: This implies the ability to quantify an activity or its results. A baseline measurement is required to document change (e.g., to measure percentage increase or decrease).
- Attainable/Achievable: The objective must be feasible with the available resources. For example, do you have the task trainer that is needed?
- Relevant: Relevant relates to the relationship between the objective and the overall goals of the program.
- Timebound: A specified, reasonable time frame should be incorporated into the objective statement.
Goal: Develop basic surgical skills
Objectives:
- Learn the general types of instruments for basic surgical techniques.
- Learn the basic concepts fundamental to suture placement: simple running and interrupted sutures (subcuticular and buried).
Step 4: Educational Strategies
This step includes the content that will be taught and the educational method that will be used along with the faculty development strategies.
Content: Simulation curricula tend to use mastery learning, a competency-based learning, where training is personalized to learner’s ability and they continue to train until they reach 100% passing. The variable becomes the number of trials to reach 100%. It is important that we “teach errors” and how to identify, avoid, and remediate. Simulation is the only educational tool that provides “permission to fail” or “do harm” without injury to a real patient.
Method: The simulation-based training curriculum should incorporate evidence-based methodological principles such as deliberate, distributed practice, or proficiency-based learning (PBL). It is not intended to completely replace training,
but, rather, to provide an effective means of overcoming the initial learning curves.4 Deliberate practice is the repetitive performance of intended cognitive or psychomotor skills. Distributed practice (also known as spaced repetition or spaced practice) is a learning strategy where practice is broken up into several short sessions, over a longer period. Proficiency-based learning refers to series of assessments and academic reporting
that are based on students demonstrating that they have learned the knowledge and skills they are expected to learn as they progress through their education.
Faculty development: Faculty involved in simulation training need to have a baseline knowledge base for the use of simulation methods and teaching skills.
Step 5: Evaluation
Evaluation is broken down into overall program and individual assessment and feedback.
Individual assessment to the learner can be provided in two forms: formative (daily feedback provided to trainees to improve technical aspects) versus summative (weekly or monthly evaluations). The overall program evaluation is critical to ensure that the learners are achieving the desired outcome and that the curriculum evolves with improvements in the educational practice.
Step 6: Implementation
Implementation relates to all steps of the curricular development. Curriculum development does not need to proceed in sequence, one step at a time, but more in a dynamic process that continues as the curriculum evolves.
Framework for Design
A cognitive, technical, and team-based component; curriculum validation; and maintenance of training (figure 2) are key aspects in procedural simulation-based training.4
Figure 3: Framework for design.
Cognitive Component
The learner must master the factual knowledge and the cognitive aspects of the task. Obtaining a baseline assessment of knowledge by a pre-test is essential as it provides the instructor information about the learner and identifies areas of weakness. More importantly, it facilitates learning as it helps the trainee to focus on what they don’t know or did wrong.
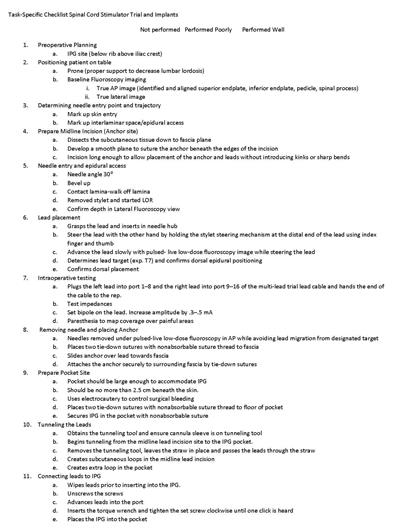
Technical Component
The technical component involves performing the task in a controlled environment and deconstructing the task into pieces. Objective Structured Assessment of Technical Skills (OSATS) were introduced to assess trainees’ skills using a task-specific checklists. 8 We have introduced a task-specific checklist for neuromodulation (figure 4) and use it to provide feedback in a formative (face-to-face and demonstrating alternative approaches on the spot) or summative (determining areas of weakness based on procedure specific assessment tool comparing against a benchmark or standard) manner.
Figure 4: Neuromodulation task-specific checklist. [View figure.]
The team-based component involves the non-technical skills, such as the ability to identify the roles and responsibilities of members in the health care team as well as improving communication skills and enhancing situational awareness. Curriculum validation is an important aspect in simulation. Being able to demonstrate effectiveness and transfer of skills to the clinical environment is the goal. Maintenance of training should include post-training sessions to assess for ongoing proficiency and help to identify cognitive knowledge and technical skills degradation in a particular task. A flow-chart approach to implementing simulation is illustrated in figure 5.
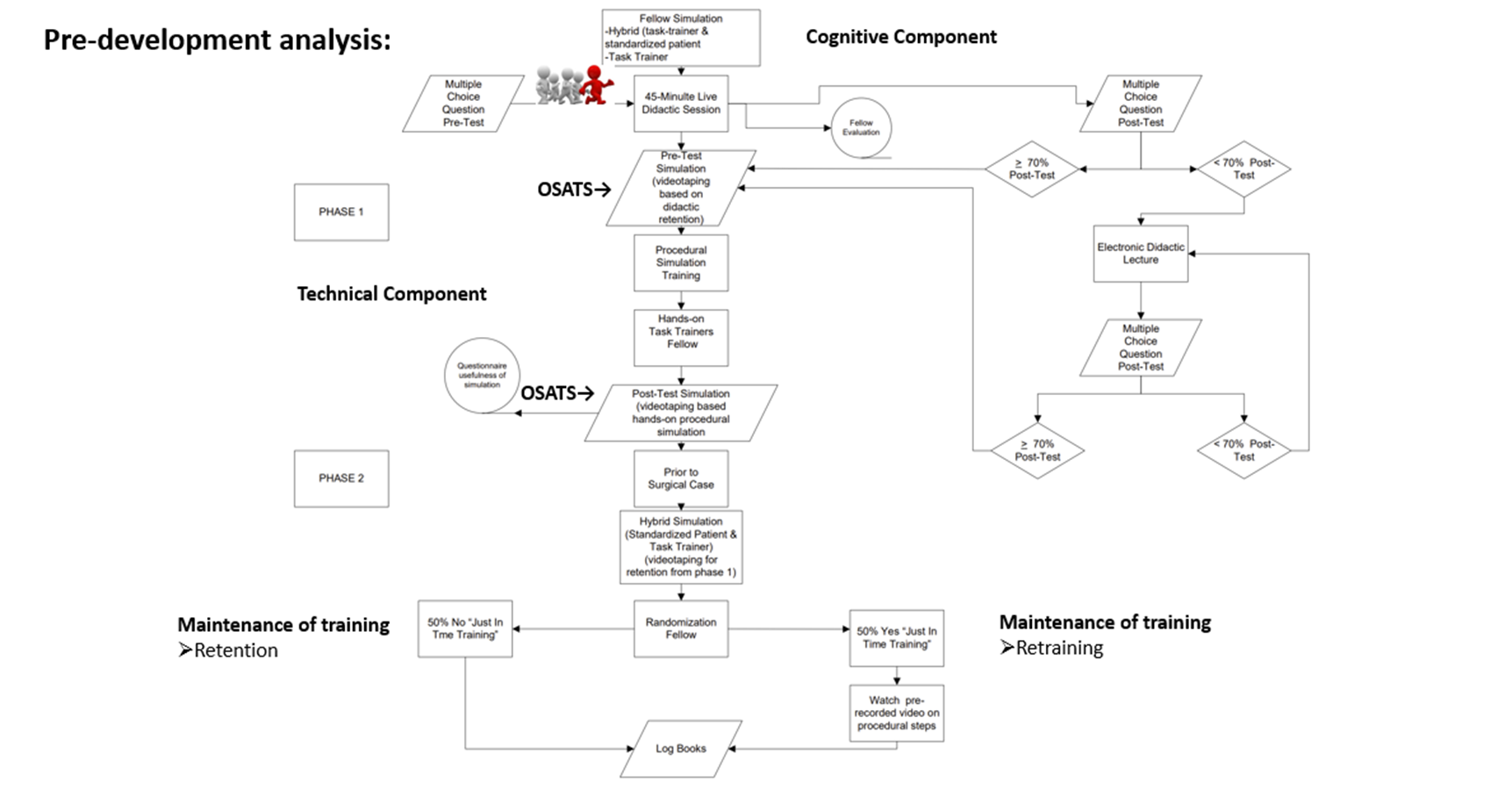
Figure 5: Flow-chart implementation of simulation-based training. [View figure.]
Conclusion
We need to shift from our traditional “see one, do one, teach one” educational approach to the “see one, simulate many, do one” approach. Improving healthcare starts at its fundamental state of medical education.
Dalia H. Elmofty, MD, is an associate professor and associate program director of the pain fellowship at the University of Chicago, IL.

References
- Halsted WS. The training of the surgeon. Bull Johns Hopkins Hosp. 1904;15:267-75.
- Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. https://doi.org/10.17226/9728.
- Khamis NN, Satava RM, Alnassar SA, Kern DE. A stepwise model for simulation-based curriculum development for clinical skills, a modification of the six-step approach. Surg Endosc 2016; 30: 279-87. https://doi.org/10.1007/s00464-015-4206-x.
- Zevin B, Levy JS, Satava RM, Grantcharov, TP. A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg. 2012;215(4):580-6. https://doi.org/ 10.1016/j.jamcollsurg.2012.05.035.
- McGaghie WC, Issenberg SB, Barsuk JH, Wayne DB. A critical review of simulation-based mastery learning with translational outcomes. Med Educ. 2014;48(4):375-85. https://doi.org/ 10.1111/medu.12391.
- Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum development for medical education: a six-step approach. Johns Hopkins University Press, 2015.
- Doran GT. There's a S.M.A.R.T. way to write management's goals and objectives. Management Review 1981;70(11):35-6.
- Martin JA, Regher G, Reznick R, et al. Objective structured assessment of technical skills (OSATS) for surgical residents. Br J Surg. 1997; 84 (2): 273-8. https://doi.org/ 10.1046/j.1365-2168.1997.02502.x

Leave a commentOrder by
Newest on top Oldest on top