Reflections of Creating a Sustainable Regional Anesthesia Curriculum in Ghana
Cite as: Alcibiade E. Reflections of creating a sustainable regional anesthesia curriculum in Ghana. ASRA Pain Medicine News 2024;49. https://doi.org/10.52211/asra020124.009.
Approximately 5 billion people in the world do not have reliable access to surgery, of which more than 2 billion people have no access to surgical care at all.1,2 Unfortunately, safe anesthetic care is an even more difficult endeavor. This issue is often related to resources we take for granted in the United States, such as reliable electricity, anesthesia machines, medications, supplies, oxygen, monitors, and adequate training. Anesthesia providers who work in these difficult conditions are extremely dedicated and hardworking, but they recognize their resource-limited environments. Anesthesia-related mortality in low-income countries has been estimated between 3-1000x higher than in high-income countries. Regional and spinal anesthesia have been cited as being safer than general anesthesia in these locations with lower mortality rates (0.06% regional, 0.04% spinal, and 1.69% general endotracheal anesthesia).2 These striking numbers make efforts like the ASRA Global Health Equity Fellowship Rotation an extremely valuable resource in low-income countries. My personal experience at Komfo Anokye Teaching Hospital (KATH) in Kumasi, Ghana, in May 2023 demonstrated the long-lasting impact and sustainable benefit these efforts can create.
I’m beyond thankful for the opportunity for this fellowship rotation provided by ASRA Pain Medicine
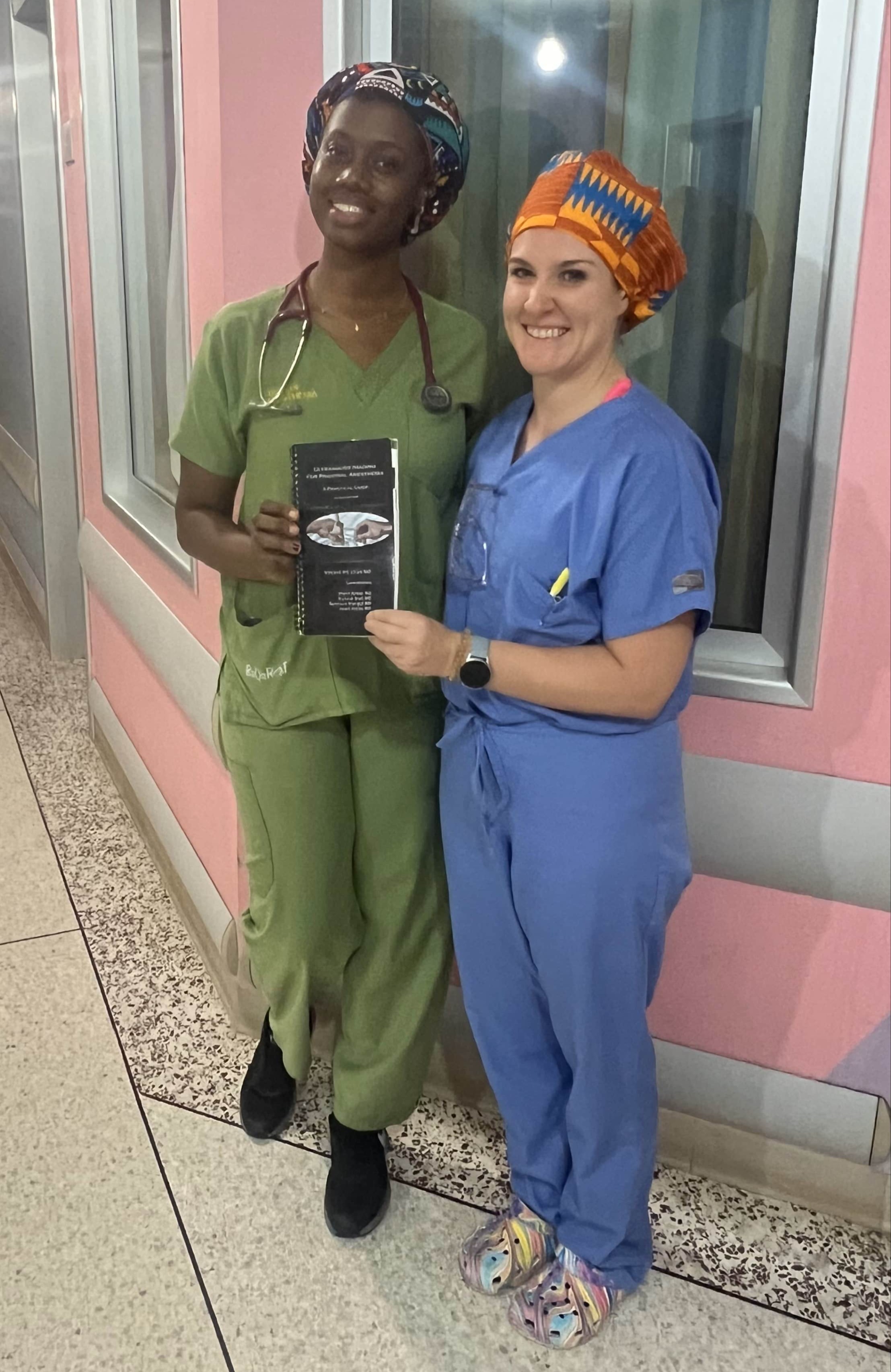
The groundwork Dr. Mark Brouillette, an anesthesiologist from Hospital for Special Surgeries (HSS) who established the connection with KATH and aided in creation of the Global Regional Anesthesia Curricular Engagement (GRACE) program3, has laid at KATH during the past several years is quite remarkable. Dr. Obiageli Ofungwu, who serves concurrently as an anesthesiologist and the first pain fellow at KATH, seeks to learn and grow not only a regional anesthesia service, but also a pain service, as her curriculum involves a combination of acute and chronic pain management techniques. Although she reports realistic views that currently there is a shortage in the staffing that would be needed to expand their service lines farther, she has high hopes that as more providers are educated on regional and pain techniques, the service will develop in the future. In fact, the regional services offered at KATH have expanded so much in recent years that the World Federation Society of Anesthesiologists (WFSA) offers a 3-month regional fellowship rotation to anesthesiologists in low- and middle-income countries to further their training and share resources with their home countries. Seeing this program occur firsthand, it was evident the impact the GRACE program has created.3
The ability to step back and watch core regional principles being passed on to new trainees demonstrates the true sustainability of these efforts. Providers at KATH are regularly performing spinals as well as upper and lower extremity blocks for primary anesthetics; however, the focus for Dr. Ofungwu during our May 2023 trip was learning new blocks to aid with pain control, focusing on placement and management of catheters and fascial plane blocks, such as the fascia iliaca, PEricapsular Nerve Group, transversus abdominis plane, rectus sheath, pectoralis, and erector spinae plane (ESP), blocks with goals to continue developing these services beyond the accident and emergency operating theaters. The ultimate goal is to have a regional and acute pain service similar to perioperative pain services that exist at many hospitals in North America.

Seeing the WFSA program in action firsthand was another noteworthy experience. Dr. Omajuwa Dudu, an anesthesiologist from Nigeria, was beginning her program at KATH when I arrived. Being able to implement the “see one, do one, teach one” model through multiple levels of training was amazing. This growth highlights the efficacy and sustainability of such programs, not only in Ghana, but their potential in many low resource settings across the world.


Adaptability, diligence, and effective communication are essential while working in unfamiliar environments. Many people accustomed to western medicine are fascinated by the fact that regional anesthesia is truly a primary anesthetic with no additional sedation, infusions, or analgesics utilized during the procedure or surgery with conversion to general anesthesia being a risky or impossible backup plan. This approach partially stems from differences in patient’s expectations, where in the United States patients expect to be “asleep” during all anesthetics, which also speaks to the improved safety profile. It may be valuable for those in the developed world to understand that patient expectation is important for surgical anesthesia with no or minimal sedation. To this notion, I often cite a healthy, 8-year-old female, who suffered a forearm fracture in a motorbike accident. Although tearful while receiving a brachial plexus block without sedation, she was smiling and singing along to the music during her operation, which would rarely occur in the United States, secondary to a variety of reasons.
Another example that emphasizes many of these logistical differences was assisting in primary blocks of the femoral and popliteal nerves for ankle surgery. Nerve blocks at KATH are commonly performed using IV needles rather than traditional block needles because they are easily and reliably obtained, cheap, and multifunctional within the hospital. During the case, the patient reported pain with deep surgical manipulation that could not be localized to a specific nerve distribution on exam. It was later discovered that “half bupivacaine” actually meant half the bottle of 0.5% bupivacaine in an attempt to conserve medication, rather than 0.5% bupivacaine! Lower concentration blocks are utilized in some centers; however, this practice is often in association with additional sedation and/or analgesia methods, which are not routinely provided in low-income countries in an attempt to lower expenses for patients. This experience was also unique from a cultural and political perspective. Dr. Alfred Aidoo, an anesthesiologist at KATH who works closely with the Hospital for Special Surgery (HSS) collaboration, and his family kindly welcomed me with open arms until the rest of the HSS crew arrived for the second week of the trip.

They invited me into their lives outside the hospital and taught me about their culture, history, education, food, and daily life, which provided amazing insight and understanding of the Ghanian people and lasting friendships! Additionally, having a diverse group consisting of anesthesiologists, an orthopedic surgeon, a pharmacist, operating room service specialist, and their Ghanian counterparts created a collaborative environment, allowing a unique multidisciplinary system. The group would regularly discuss their experiences, and having feedback offered from various mindsets created a better understanding of how to make realistic impacts within the KATH system. Furthermore, with the assistance of Dr. Aidoo, several important meetings occurred with both hospital and government officials to further create a sustainable, long-term impact, which is extremely imperative and often overlooked or difficult to achieve during medical missions.
With the sponsorship of such a prominent organization, such as ASRA Pain Medicine, trainees can start getting involved in global health early in their careers. Although I’ve always been passionate about global health, I’m beyond thankful for the opportunity for this fellowship rotation provided by ASRA Pain Medicine, the connections of the Global Health SIG, and the collaboration and friendships with local Ghanian providers, recognizing that although my goal was to teach, I simultaneously learned even more myself. This rotation was a priceless experience, and I highly recommend that anyone passionate about regional anesthesia and global health get involved with such opportunities. Finally, I would like to thank Dr. Vincent Chan for his generous book donations.


Erica Alcibiade, DO, is a regional anesthesia and acute pain medicine fellow at Johns Hopkins University in Baltimore, MD.
References
- Dohlman LE, Thakkar N, Jivanelli B, et al. Regional anesthesia global health collaborations- a scoping review of current intervention methods. Curr Opin Anaesthesiol 2022;35(5):647-53. https://doi.org/10.1097/ACO.0000000000001178
- Dohlman LE. Providing anesthesia in resource-limited settings. Curr Opin Anaesthesiol 2017; 30(4):496-500. https://doi.org/10.1097/ACO.0000000000000477
- Brouillette MA, Aidoo AJ, Hondras MA, et al. Regional anesthesia training model for resource-limited settings: a prospective single-center observational study with pre–post evaluations. Reg Anesth Pain Med 2020;45(7):528–35. https://doi.org/10.1136/rapm-2020-101550