How We Do It: Salt Lake City Veterans Affairs Medical Center Transitional Pain Service
Program Design and Implementation:
In January of 2018, we developed and implemented a Transitional Pain Service (TPS)1 at the Salt Lake City Veterans Administration Medical Center. The multidisciplinary team consists of an anesthesiologist with specialization in acute pain management, two nurse practitioners with experience in both acute and chronic pain management, four nurse care coordinators, and a psychologist (Figure 1).
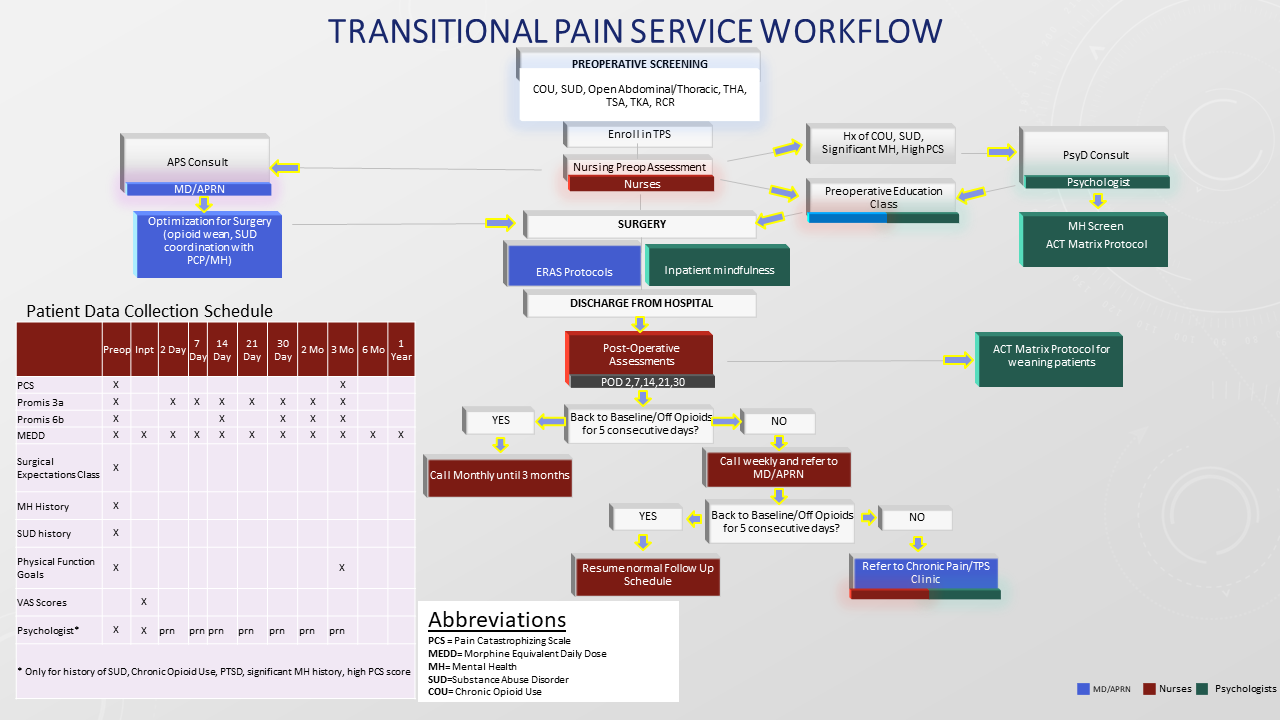
Figure 1. Transitional Pain Service Workflow
We enroll all patients who are at high risk for persistent postoperative pain,2 as well as all patients who have a history of substance abuse disorder or chronic opioid use. Once identified, the patients are contacted by one of our TPS team members and invited to attend a one-time presurgical expectations class that includes topics on expectations for postoperative pain,3,4 available analgesic therapies, appropriate use of opioids, and the impact of psychological factors on pain.5,6 Pain coping strategies are introduced using a Mindfulness-Based Intervention and Acceptance and Commitment Therapy matrix.7 In addition, the nurse practitioner and/or anesthesiologist meets individually with patients to develop a personalized plan that may include preoperative opioid taper, a buprenorphine use strategy, or opioid-free strategies.
Chronic opioid use patients have been more likely to stop opioid use altogether or decrease their dose from baseline compared to prior to TPS implementation and are less likely to increase their opioid use after surgery.
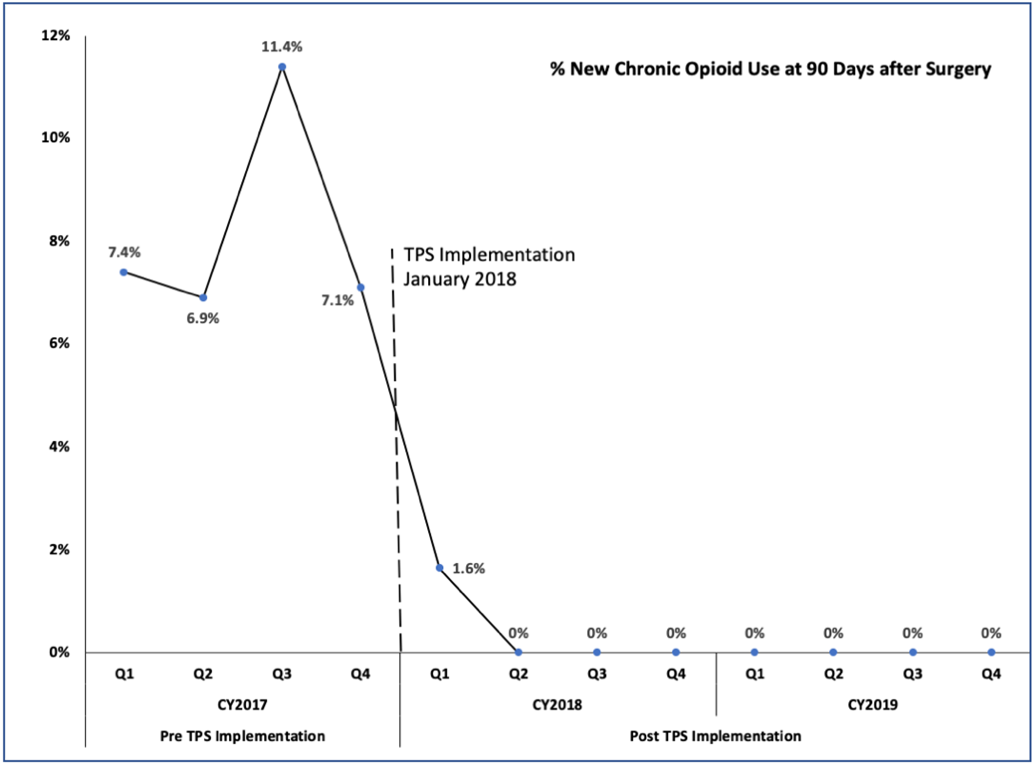
Figure 2: Percent of Preoperative Opioid Naïve Patients with New Chronic Opioid Use 90-Days after Surgery before and after TPS implementation8
Conclusion
Michael J. Buys, MD, is an anesthesiologist at Salt Lake City Veterans Administration Medical Center and an associate professor in the department of Anesthesiology at the University of Utah in Salt Lake City.
References:
- Huang A, Azam A, Segal S, et al. Chronic postsurgical pain and persistent opioid use following surgery: the need for a transitional pain service. Pain Manag. 2016;6:435-43.
- Glare P, Aubrey KR, Myles PS. Transition from acute to chronic pain after surgery. Lancet. 2019;393:1537-46.
- Lee BH, Wu CL. Educating patients regarding pain management and safe opioid use after surgery: a narrative review. Anesth Analg. 2020;130:574-81.
- Rucinski K, Cook JL. Effects of preoperative opioid education on postoperative opioid use and pain management in orthopaedics: A systematic review. J Orthop. 2020;20:154-9.
- Dunn LK, Sun EC. Mind over matter: reducing perioperative opioid use through patient education. Anesth Analg. 2020;130:556-8.
- Horn A, Kaneshiro K, Tsui BCH. Preemptive and preventive pain psychoeducation and its potential application as a multimodal perioperative pain control option: a systematic review. Anesth Analg. 2020;130:559-73.
- Azam MA, Weinrib AZ, Montbriand J, et al. Acceptance and commitment therapy to manage pain and opioid use after major surgery: preliminary outcomes from the Toronto General Hospital Transitional Pain Service. Can J Pain. 2017;1(1). https://doi.org/10.1080/24740527.2017.1325317
- Buys MJ, Bayless K, Romesser J, et al. Opioid use among veterans undergoing major joint surgery managed by a multidisciplinary transitional pain service. Reg Anesth Pain Med. 2020;6:rapm–2020–101797–852.

Leave a commentOrder by
Newest on top Oldest on top