Interview with the 2023 John J. Bonica Award Recipient: Dr. David Julius
Cite as: Shanthanna, H. Interview with the 2023 John J. Bonica award recipient: Dr. David Julius. ASRA Pain Medicine News 2023;48. https://doi.org/10.52211/asra110123.004.
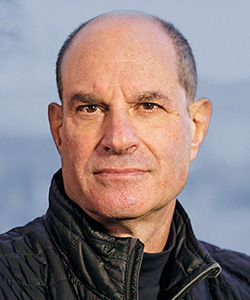 David Julius, PhD, who received the Nobel Prize in Medicine in 2021, has been selected to receive ASRA Pain Medicine’s 2023 John J. Bonica Award. Dr. Julius is a professor and chair in the department of physiology
at the University of California, San Francisco, where he has worked since completing his postdoctoral fellowship at Columbia University in New York in 1990. He received his undergraduate degree at Massachusetts Institute of Technology and his
graduate degree at the University of California, Berkeley.
David Julius, PhD, who received the Nobel Prize in Medicine in 2021, has been selected to receive ASRA Pain Medicine’s 2023 John J. Bonica Award. Dr. Julius is a professor and chair in the department of physiology
at the University of California, San Francisco, where he has worked since completing his postdoctoral fellowship at Columbia University in New York in 1990. He received his undergraduate degree at Massachusetts Institute of Technology and his
graduate degree at the University of California, Berkeley.
He is the recipient of numerous impressive awards and honors, including the 2010 Shaw Prize in Life Sciences and Medicine and the 2020 Breakthrough Prize in Life Sciences. He shared the Nobel Prize with Ardem Patapoutian, PhD, in 2021 “for their discoveries of receptors for temperature and touch,” according to the Nobel Prize organization.
ASRA Pain Medicine News Special Projects Associate Editor Harsha Shanthanna recently interviewed Dr. Julius about his career path and research interests as well as his perspective on mentorship, success, and future directions for pain research.
Harsha Shanthanna: You are recognized as an exceptional researcher, leader, educator, and clinician within the field of pain medicine. Can you briefly outline your journey? How did you decide to focus on pain medicine?
David Julius: My professional background and training are in the area of basic biomedical research (I am not a clinician), and my initial experience and inspiration come from working to understand how enzymes catalyze reactions to modulate cellular activities, such as protein synthesis and hormone maturation and secretion. Thus, my scientific compass has always pointed towards a goal of determining how molecules do what they do in the framework of understanding physiology and disease.
I came to focus on the biology of pain through the convergence of two interests, namely, the molecular biology of neurotransmitter receptors and the use of natural products as investigational and therapeutic agents. Together, these paths led me to exploit natural products, such as capsaicin, menthol, and isothiocyanates (wasabi), as probes to uncover receptors involved in nociception and pain.
HS: What inspired you to take up research into neuropharmacological molecular mechanisms in the field of pain management? Were there any personal or professional influences?
DJ: Mostly just curiosity. I was generally interested in sensory systems, and at that time, nociception/pain seemed to be the sensory modality that was most in need of basic insights into underlying molecular mechanisms. Also, as noted above, I was captivated by the prior and foundational work of others, such as Jansco and Zotterman, in using plant-derived irritants like capsaicin and menthol to probe cellular mechanisms’ underlying somatosensation and pain. What was missing was a molecular understanding of how these agents work, which was already a looming question in the nascent field of molecular pain research. This seemed like too exciting of a challenge to ignore.
HS: As a researcher who primarily works in the laboratory, what are your views on the translational gap that exists between basic science research using experimental pain models and clinical pain research that depends on patient-reported outcomes?
DJ: Of course, in vitro cell models, and even mice, are not humans, and they cannot tell us how they feel and experience pain. This leaves gaps in our ability to connect findings from such model systems to the human experience and therapeutics, not to mention specific physiological differences. Certainly, comparisons across species have their inherent limitations for understanding complex integrative components of the pain experience, such as emotional and affective aspects, which cannot be achieved by studying cells in a dish or non-declarative animals such as mice. But you work with what you have and go from there.
Indeed, cell biology, mouse genetics, and the like have already provided tremendous insights into cellular pathways, receptors, and other molecules that are relevant to nociception and pain sensation in all mammals—information that enables us to bootstrap to humans through genetic and pharmacological approaches. Also, the goal of developing more objective methods for assessing pain, such as imaging and identification of biomarkers, could help to close gaps between animal models and the human experience.
HS: It is very interesting that you discovered that the same transient receptor potential (TRP) ion channel transmits noxious heat and the pungent/burning characteristic of chili peppers. It is also somewhat (from an evolutionary point) counterintuitive that capsaicin is used to help relieve pain. Do you think these effects are different depending on whether the pain is acute or chronic?
DJ: Yes, there is this paradoxical use of capsaicin for treating pain, and to my knowledge this does apply only to chronic situations, such as post-viral neuropathies or hyperactive bladder. This concept and approach are based on the early observations of Jansco, Szolcsányi, and others, showing that prolonged or high-dose capsaicin treatment desensitizes nociceptors, thereby rendering them non-responsive for some period. This is an interesting phenomenon for which the underlying mechanism(s) is not fully understood, but something that we are now looking at in greater detail.
HS: With your discoveries, do you see TRP channel modulators as new targets for pain medications?
DJ: I am not involved in drug discovery or clinical trial endeavors, but the biology seems right in that TRP channels, such as transient receptor potential vanilloid 1 (TRPV1) and transient receptor potential ankyrin 1 (TRPA1), are involved in inflammatory hyperalgesia, making them potentially relevant to a range of chronic pain syndromes. TRPV1 antagonists have run into problems associated with “on-target” side effects, such as diminished sensitivity to noxious heat and transient alterations in core body temperature, but perhaps there is still a way forward for this target. What this outcome does illustrate is the challenge of targeting “nociceptive receptors” in a way that reduces maladaptive pain without diminishing acute protective pain.
TRPA1 antagonists could also have potential utility in treating pain syndromes where chemically reactive irritants (exogenous or endogenous) are involved; these might include arthritic joint pain, hemorrhagic cystitis resulting from chemotherapy, or airway irritation and hyper-reactivity. For TRPM8, a potential application might include treating cold allodynia, resulting from chemotherapy or nerve injury.
I truly hope that one or more of the channels that we have worked on prove to be targets for new analgesics—that would be a fantastic practical outcome. But I think the bigger message is that we must continue to probe the basic biology of nociception and pain sensation as this is essential to taking a rational, mechanism-based approach to finding new non-opioid analgesics. If not TRP channels, then other therapeutic targets or strategies will hopefully emerge from this approach.
HS: With more than 5,000 members worldwide, ASRA Pain Medicine is perhaps the largest organization dedicated to excellence in the practice of regional anesthesia and acute and chronic pain medicine. Do you have any key messages for ASRA Pain Medicine’s leaders on advancing pain research?
DJ: Not surprisingly, supporting both basic and clinical research is critical to making progress in this area. A broad view of the field that fosters interaction among scientists and clinicians will ensure that fresh ideas and approaches are brought to the table.
Success is measured differently by each person, but for me it’s defined by making impactful discoveries, having opportunities and resources to explore new scientific territory, and watching my trainees succeed and move on to top-notch independent positions in academia or industry.
HS: How do you define success, and which qualities do you think allow one to grow as a successful researcher?
DJ: I think that some of the most important qualities are curiosity, persistence, regular and open engagement with colleagues, a passion and drive for experimentation, and an honest and unbiased approach to research. At my stage (ie, group leader), energetic and thoughtful mentorship is also a critical factor for success and professional fulfillment.
Success is measured differently by each person, but for me it’s defined by making impactful discoveries, having opportunities and resources to explore new scientific territory, and watching my trainees succeed and move on to top-notch independent positions in academia or industry.
HS: As much as we cannot depend on it, luck or chance tends to play a role in everyone’s life. Has chance had any influence in your career?
DJ: Yes, I’ve had moments when chance intervened favorably. In graduate school, I came to work with my mentors through an unanticipated change in circumstances, which initiated an incredibly exciting, productive, and formative time in my early career.
HS: Mentors play a great role in shaping our success. What are your thoughts on mentorship, and who do you think has had the most influence in your career?
DJ: Yes, mentorship is key and who you are as a scientist is, to some extent, a reflection of those with whom you have trained. I have absorbed important insights and strategies from each of my mentors, who have approached science from different viewpoints and with distinct styles. I can see aspects of their styles in my own scientific persona.
HS: Which do you think were the most defining moments in your career?
DJ: Every stage has had its important and defining moments. As an undergraduate, I learned that I had an affinity for hands-on experimental research. In graduate school, I realized that I could do something exciting and original. As a postdoctoral fellow, I learned to be resilient and persistent in the face of failure. As a faculty member, I’ve learned how to mentor and inspire others.
HS: You have won so many awards and accomplished so much in your career. Which of them have been the most rewarding or satisfying?
DJ: It’s hard to choose a favorite discovery or moment as one’s scientific trajectory is a continuum of learning and progress. In the end, one’s legacy consists of the discoveries you’ve helped make and the people you’ve mentored.
HS: Do you have any advice to offer current trainees or early career professionals who are looking for a career in pain research?
DJ: As research scientists, we have the freedom and luxury to explore and satisfy our curiosity. This comes with the risk of failure and some uncertainty about where our work is headed. So, my advice is to pick a problem that is sufficiently engrossing to maintain your passion for exploration, even when times are tough, and you need to be persistent. For me, pain research meets this high bar because there is so much that we don’t yet understand, and the potential payoff from both intellectual and therapeutic standpoints is huge.
HS: Where do you see the most potential/unexplored areas for future research in pain medicine? Which question(s) may be most influential to future practice?
DJ: We use one term, “pain,” to describe what is really a collection of distinct maladies. Osteoarthritic knee pain is different from lower back pain, gastrointestinal pain, headache, viral or diabetic neuropathy, and so on. The challenge is to choose or define a system or approach that can help to better define specific peripheral and/or central mechanisms that contribute to each of these chronic pain syndromes. With the continuous discovery and development of new molecular probes and imaging tools, we can begin to delve into the specific factors (genetic, cellular, biochemical) that promote or sustain specific chronic pain syndromes – to understand which are shared and which are unique across syndromes. Another challenge, and an area that is now attracting great interest, is to better understand mechanisms of bidirectional communication between peripheral organs (such as the gut) and the brain and how chronic pain and other maladaptive syndromes affect emotional and affective states.
HS: What do you love the most about your job?
DJ: As a mentor of an academic lab, I’m always surrounded by energetic and curious young people—graduate students and postdoctoral fellows who stay for a few years to train before moving onto the next stage of their careers. Consequently, I have this false sense of perpetual youth!
