Plastic in Healthcare: Everywhere and Hidden in Plain Sight
Cite as: Kelleher DC, Fouts-Palmer EB, Ip V. Plastic in healthcare: everywhere and hidden in plain sight. ASRA Pain Medicine News 2024;49. https://doi.org/10.52211/asra050124.006.
The theme for Earth Day 2024 is “Planet vs Plastics.”1 Since their introduction over 70 years ago, plastics have grown exponentially with more than 430 million tons produced annually and continued growth expected.2 Unfortunately, most of these plastics are used briefly and quickly end up in landfills or as litter on the streets and in our oceans. Less than 9% of all plastics are recycled.2
Beyond the physical waste, fossil fuels burned, and emissions created from producing plastic, more concerning are the now ubiquitous breakdown products of macroplastics – micro (< 5 mm) and nanoplastics (< 1 µm). Furthermore, the polymers and the chemicals associated with plastic are now permanently accumulating in our environment. Microplastics have been detected in 81% of global tap water samples and 93% of bottled water with bottled water having over 20 times the amount of microplastics compared to tap (94 particles/L versus 4 particles/L).3 Plastic is also present in our food chain, both from animals consuming plastic in their own diets and from plastic packaging leaching into food products. Microplastics have been detected in honey, beer, salt, sugar, and seafood. They are also in the air (9.8 particles per 1000 L), and higher amounts are detected in areas where plastics and fabrics are produced.3
With the amount of plastic found in our environment, it is no surprise that micro and nanoplastics are now detected throughout the human body, including in the heart, lungs, liver, gastrointestinal tract, vasculature, and blood.4 The particles enter our body mainly through ingestion and inhalation. Microplastics are transported into cells through lysosomes and other means, and nanoplastics are small enough to easily be absorbed both in the gastrointestinal tract and alveolar surface. In fact, nanoplastics are feared to be more toxic than microplastics as their size allows them to easily cross most physiologic barriers and accumulate in almost any organ of the body.5 Plastic particles are also detected in both the extracellular and intracellular compartments of the human placenta and in newborn meconium, indicating not only maternal-fetal transfer of plastics, but fetal processing of plastic in newborns’ gastrointestinal tract as well.6,7

The effects of these plastics on human health are just beginning to be investigated. While several chemicals associated with plastic, including “bisphenol A (BPA), phthalates, triclosan, bisphenone, organotins, and brominated flame retardants (BFR),"have been officially noted to be harmful to human health, many other chemicals are likely to be harmful as well, but have yet to be tested in-depth.3 Through in vivo and in vitro studies, micro and nanoplastics have been associated with increased inflammation, oxidative stress, and metabolic disruption.3 Strong evidence also exists that these particles contribute to endocrine disruption, altering both thyroid and steroid hormone production and function, potentially contributing to decreased fertility and increased cancer risk.5 Furthermore, the effect of micro and nanoplastics on the gut microbiota may increase the prevalence of gut dysbiosis-associated diseases, such as obesity, cardiovascular disease, hypertension, and diabetes.8 Analysis of human placentas shows evidence of intracytoplasmic organelle dysfunction, including endoplasmic reticulum and mitochondrial stress, near areas of microplastic particles.6 Similar findings have previously only been found in placentas associated with pathological states, such as those with preeclampsia or intrauterine growth restriction. Finally, as nanoplastics can readily cross the placenta and blood-brain barrier, there is concern that they may contribute to the growing prevalence of neurodevelopmental conditions, including autism and attention-deficit/hyperactivity disorder (ADHD) in children, and dementia in adults.9
With the amount of plastic found in our environment, it is no surprise that micro and nanoplastics are now detected throughout the human body, including in the heart, lungs, liver, gastrointestinal tract, vasculature, and blood.
Healthcare contributes substantially to the plastic waste problem, especially with the unrelenting trend towards single-use devices and the overuse of personal protective equipment. Few of our medications avoid touching plastic before delivery to our patients. Many are delivered in plastic tubing and syringes, while some are even made of plastic, as is the case with polyethylene glycol (PEG).10 While much of the plastic we use in healthcare is deemed necessary for the safety and well-being of our patients, it is important to take a critical look at the products we use. Below we breakdown some areas of hidden plastics in healthcare.
Disposable perioperative warm-up jackets: Typically made of spunbond meltdown spunbond (SMS) material, an industry term meaning spunbond meltblown spunbond, referring to a tri-layer non-woven plastic product made of polypropylene,11 these jackets were briefly mandated as surgical attire by the Joint Commission at great cost to medical facilities and the environment. In one roughly two-year study, the jackets increased hospital costs by $1.7 million with no effect on surgical site infections.12 Plus, the 2 million jackets purchased at this institution alone contributed unnecessary plastic waste to the landfill. While many hospitals have dropped the mandate for these jackets, many continue to offer them for the comfort of their employees.
Recommendation: Offer reusable warm-up jackets in natural fabrics (Figure 1).

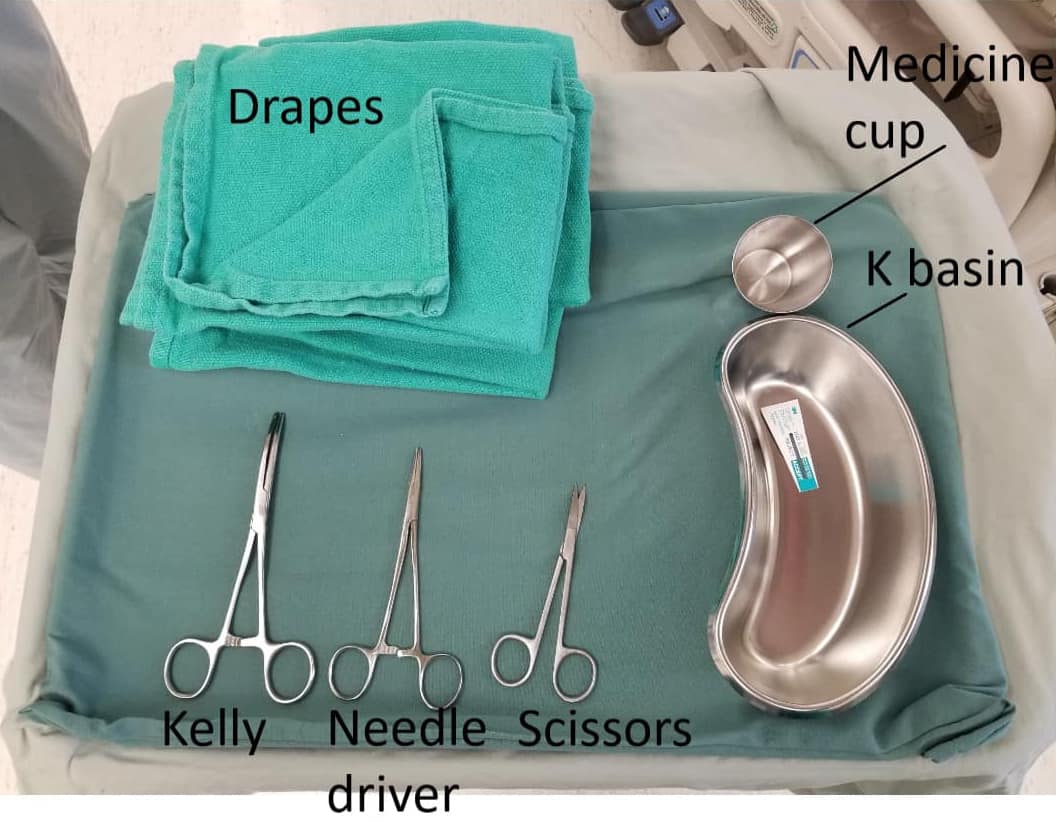
Disposable surgical gowns and drapes: Both are made of SMS. While necessary for sterile surgical procedures, there is a trend towards overuse, including use of gowns for provider comfort and drapes for procedures not needing sterile barrier precautions. Gowns and drapes have different permeabilities, and more plastic and carbon emissions are associated with thicker, less permeable products.13
Recommendation: Limit the use of surgical gowns and drapes to sterile surgical procedures only. Use the protection level commensurate with the risk of the procedure. Limit the number of individuals who scrub into any given case. Make smaller add-on drapes and sleeves available to avoid opening a large drape for a small area or needing a new gown for a contaminated sleeve.
Disposable Bouffant Caps: Made of polypropylene. Avoiding disposable caps may be simpler than avoiding other forms of personal protective equipment as there is a ready alternative: reusable cloth caps. Disposable caps have shown no infection control advantage over reusable versions. In fact, reusable cloth caps may be superior; the disposable versions have been found to be more permeable with greater microbial shed.14 Furthermore, they can help with patient safety when they include a clinician’s name and role by improving communication and teamwork within the perioperative setting.15
Recommendation: Encourage the use of natural fabric, reusable surgical caps.
Surgical Masks: Made of various plastic materials, including polypropylene, polyurethane, and polyacrylonitrile. In 2020, over 3 million tons of surgical mask waste was created (up from 700,000 tons in 2019) due to the global pandemic.11 At the time, increased use of masks was necessary to protect healthcare workers and the public. It is now important to critically assess when masks are necessary in terms of risks-benefits ratio, widespread availability, and adoption of vaccinations as well as overall reduction in disease severity. Additionally, educating the public on proper use and disposal of masks will help decrease the negative environmental effects being seen from their widespread use.16
Gloves: Since natural latex gloves have been mostly eliminated, sterile and non-sterile gloves are made of different types of plastic, including nitrile.
Recommendation: Choose hand hygiene for tasks that do not require gloves.17 This may include tasks such as placing monitors and non-invasive examinations of patients.
Scrubs: Much of our clothing is made of plastic. Most hospital-provided scrubs are made of at least 50% polyester, a synthetic plastic fiber. While reusable items are preferred to disposable ones, the creation of polyester fabric and the subsequent washing of the material leads to plastic fibers in the air and water (Laundering 6 kg of polyester-based materials can result in over 700 fibers contaminating the water per wash).4
Recommendation: Limit the availability of polyester-based, hospital-laundered scrubs to necessary personnel only. Wear scrubs only when working in attire-restricted areas. Not only does this reduce air and water plastic contamination, but also energy use from the high heat washing required for hospital-provided garments and any emissions from transporting the scrubs to and from the laundering site.
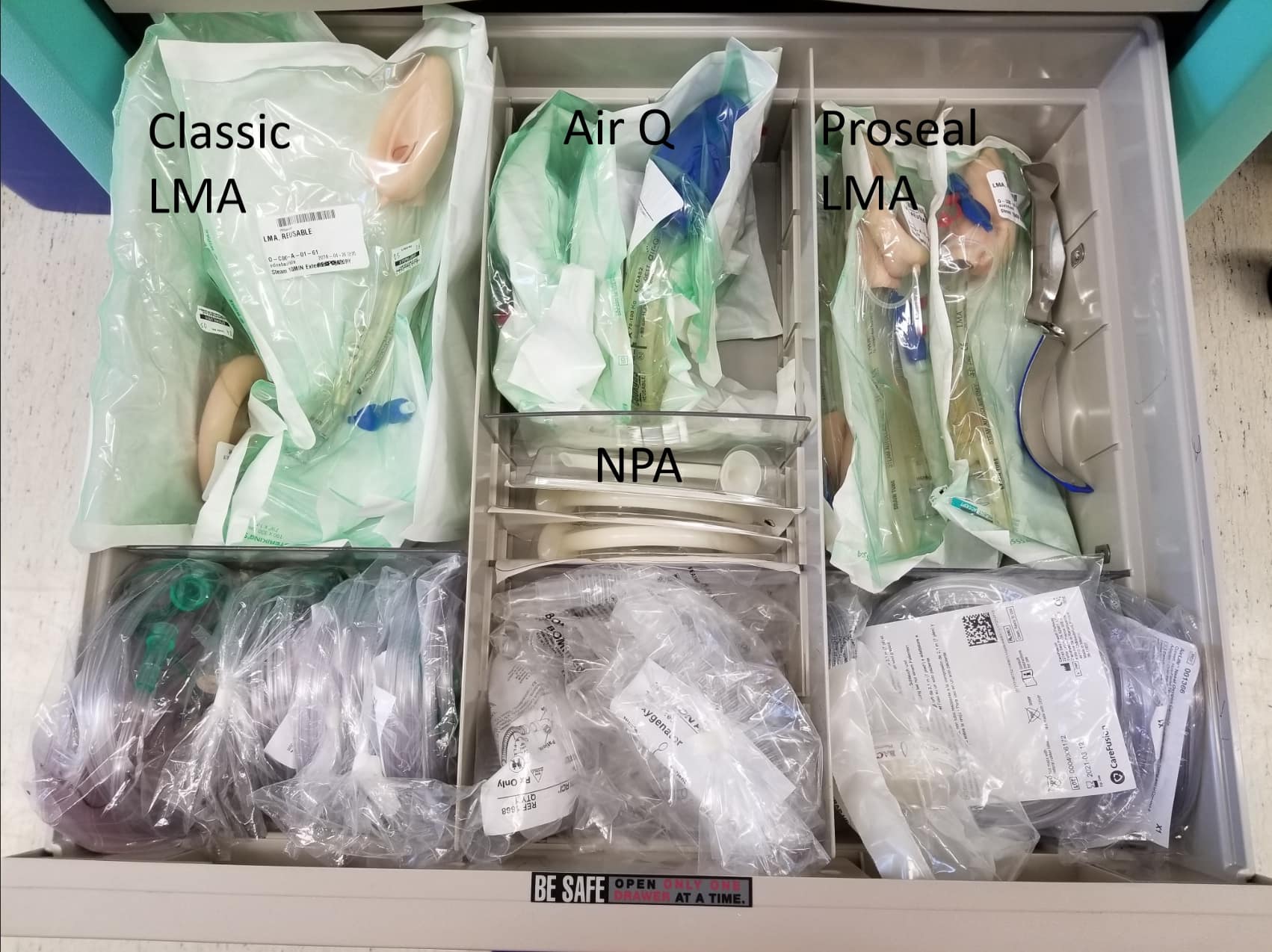
Single-use laryngoscopes, bronchoscopes, and laryngeal mask airways: These are not so hidden, but increasing in prevalence, and made of various plastic types. There is increasing adoption of these devices in the name of infection prevention despite the minimal evidence that the reusable versions increased risk. A review of much of the available evidence continues to point to poor hand hygiene as the main cause of anesthesia-related infections and emphasizes that proper disinfection of clinicians’ hands should be prioritized over switching to single-use devices.18 Reusable devices reduce costs, plastic waste, and carbon emissions.
Recommendation: Use evidence to guide decisions on single use versus reusable devices. Be active in participating in procurement decisions for your department. Invest in proper cleaning practices for reusable devices to avoid early breakage and reduce risk of contamination (Figure 2).
Plastic is unavoidable in healthcare. However, its use and breakdown products contribute to potential harm for not only our current patients, but for our future patients as well. In general, hospital administrators must be thoughtful when making policies regarding personal protective equipment and when purchasing equipment (reusable versus disposable). Individuals should be mindful about their overuse of available equipment and avoid using items out of convenience rather than necessity. Humans are responsible for creating plastics, and in doing so, we are indirectly harming our planet and humanity. Reducing healthcare’s overall consumption of goods is critical to lessening the plastic burden created from the care we provide.



References
- Earth Day: The Official Site. Washington, DC: EARTHDAY.ORG. Available at: https://www.earthday.org.Accessed January 30, 2024.
- Fast facts — what is plastic pollution? United Nations Sustainable Development. https://www.un.org/sustainabledevelopment/blog/2023/08/explainer-what-is-plastic-pollution. Published August 25, 2023. Accessed January 30, 2024.
- Yee MS, Hii LW, Looi CK, et al. Impact of microplastics and nanoplastics on human health. Nanomaterials (Basel) 2021;11(2):496. https://doi.org/10.3390/nano11020496
- La Porta E, Exacoustos O, Lugani F, et al. Microplastics and kidneys: an update on the evidence for deposition of plastic microparticles in human organs, tissues and fluids and renal toxicity concern. Int J Mol Sci 2023;24(18):14391. https://doi.org/10.3390/ijms241814391
- Leso V, Battistini B, Vetrani I, et al. The endocrine disrupting effects of nanoplastic exposure: a systematic review. Toxicol Ind Health 2023;39(11):613-29. https://doi.org/10.1177/07482337231203053
- Ragusa A, Matta M, Cristiano L, et al. Deeply in plasticenta: presence of microplastics in the intracellular compartment of human placentas. J. Environ. Res. Public. Health2022;19:11593. https://doi.org/10.3390/ijerph191811593
- Liu S, Liu X, Guo J, et al. The association between microplastics and microbiota in placentas and meconium: the first evidence in humans. Environ Sci Technol 2023;57(46):17774-85. https://doi.org/10.1021/acs.est.2c04706
- Niu H, Liu S, Jiang Y, et al. Are microplastics toxic? A review from eco-toxicity to effects on the gut microbiota. Metabolites 2023;13(6):739. https://doi.org/10.3390/metabo13060739
- Chen S, Chen Y, Gao Y, et al. Toxic effects and mechanisms of nanoplastics on embryonic brain development using brain organoids model. Sci Total Environ 2023;904:166913. https://doi.org/10.1016/j.scitotenv.2023.166913
- Ragusa A, Lelli V, Fanelli G, et al. Plastic and placenta: identification of polyethylene glycol (PEG) compounds in the human placenta by HPLC-MS/MS system. Int J Mol Sci 2022;23(21):12743. https://doi.org/10.3390/ijms232112743
- Uddin MA, Afroj S, Hasan T, et al. Environmental impacts of personal protective clothing used to combat COVID- 19. Adv Sustain Syst 2022;6(1):2100176. https://doi.org/10.1002/adsu.202100176
- Stapleton EJ, Frane N, Lentz JM, et al. Association of disposable perioperative jackets with surgical site infections in a large multicenter health care organization. JAMA Surg 2020;155(1):15-20. https://doi.org/10.1001/jamasurg.2019.4085
- Quintana-Gallardo A, del Rey R, González-Conca S, et al. The environmental impacts of disposable nonwoven fabrics during the COVID-19 pandemic: case study on the Francesc de Borja Hospital. Polymers 2023; 15(5):1130. https://doi.org/10.3390/polym15051130
- Markel TA, Gormley T, Greeley D, et al. Hats off: a study of different operating room headgear assessed by environmental quality indicators. Journal of the American college of surgeons. 2017;225(5):573-81. https://doi.org/10.1016/j.jamcollsurg.2017.08.014
- Wong BJ, Nassar AK, Earley M, et al. Perceptions of use of names, recognition of roles, and teamwork after labeling surgical caps. JAMA Netw Open 2023;6(11):e2341182. https://doi.org/10.1001/jamanetworkopen.2023.41182
- Wang L, Li S, Ahmad IM, et al. Global face mask pollution: threats to the environment and wildlife, and potential solutions. Sci Total Environ 2023;887:164055. https://doi.org/10.1016/j.scitotenv.2023.164055
- Jeffries SD, Tu Z, Xu H, et al. Use of hand sanitiser as a potential substitution for nonsterile gloves in reducing carbon emissions. Br J Anaesth 2023;131(1):e22-e25. https://doi.org/10.1016/j.bja.2023.03.029
- Reynier T, Berahou M, Albaladejo P, et al. Moving towards green anaesthesia: are patient safety and environmentally friendly practices compatible? A focus on single-use devices. Anaesth Crit Care Pain Med2021;40(4):100907. https://doi.org/10.1016/j.accpm.2021.100907