Peer-Driven Principles Promote Correct-Site Nerve Blocks
Overview
Wrong-site nerve blocks (WSBs) comprise nearly 26% of all wrong-site procedures reported in Pennsylvania since 2004. To address their frequency, the Pennsylvania Society of Anesthesiologists and Pennsylvania Patient Safety Authority joined forces to review the literature and consider Pennsylvania health care facilities’ current prevention practices. With the assistance of a multidisciplinary task force, 21 principles emerged reflecting clinical, environmental, and cultural practices to prevent WSBs.
“Although professional organizations have previously published recommendations for preventing wrong-site procedures, including those specific to nerve blocks, the consensus-based, peer-driven 21 principles resulting from this collaboration are unique compared with other guidelines and statements.”
Data Define the Problem
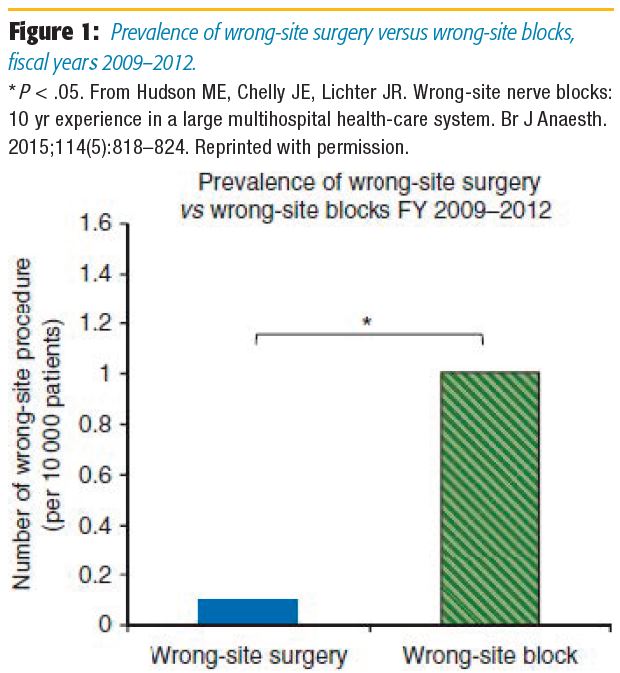
The Pennsylvania Patient Safety Authority (authority) has tracked reports of wrong-site procedures through the Pennsylvania Patient Safety Reporting System (PA-PSRS) since 2004.* Of all the wrong-site procedures identified between July 2004 and September 2017, nearly 26% were WSBs administered by anesthesiologists or surgeons. In a systematic literature review, Deutsch et al[2] noted that the incidence of WSB from four publications reporting at least 10,000 patients ranged from 0.52 to 5.07 per 10,000 blocks, unilateral blocks, or at-risk procedures. In one of the publications, Hudson et al,[3] from the University of Pittsburgh, determined that the prevalence of WSB was 1.28 per 10,000 unilateral procedures between 2003 and 2012 and that the organization's prevalence of WSB was 10 times higher than that of wrong-site surgery between 2009 and 2012 (Figure 1).
* PA-PSRS is a secure, web-based system that permits medical facilities to submit reports of serious events and incidents involving patients, as defined by the Medical Care Availability and Reduction of Error Act.[1]
Partnership Addresses Common Goal. In response to what appeared to be a slower adoption of wrong-site prevention practices by anesthesiologists in perioperative or pain services than by surgical teams, the Pennsylvania Society of Anesthesiologists (society) and authority partnered in 2015 to help Pennsylvania physicians and health care facilities implement a set of clinical, organizational, and cultural approaches to prevent WSBs. The initiative focused on perioperative nerve blocks performed by anesthesiologists on the day of surgery and excluded both local anesthetic infiltration or peripheral nerve blocks administered by surgeons as part of a surgical procedure and nerve blocks performed for chronic pain management.
To obtain a broad perspective of the contributing factors, morbidity, and potential strategies for preventing WSBs, representatives from the authority and society performed a systematic review of the English-language world literature.[2] In the 70 publications reviewed, they identified the following 5 common themes as contributing to WSBs:
- Time pressure (eg, case volume, time required for additional safety steps, production demand, pressure from patients)
- Personnel factors (eg, changes in personnel, novice care providers, cognitive error, apraxia, reliance on memory, incompetence, complacency, fatigue)
- Site mark not visible (eg, block mark not done, block mark smeared, surgical mark not visible during nerve block or not done)
- Distraction (eg, interruption, teaching, time delay, running two rooms, intervening procedures)
- Inadequate communication (eg, language barriers; inadequate documentation; missing, inconsistent, or incorrect documentation; lack of surgical consent; use of abbreviations)
The collaborative team also engaged a multidisciplinary task force of 11 anesthesiologists: 9 with expertise in perioperative nerve blocks and 2 consultants, 4 surgeons, 3 pain service nurses, and 2 patient representatives. The task force represented 10 academic and private health care centers in Pennsylvania.
Each task force member participated in a structured interview with the collaborative team to discuss potential WSB risk factors and their respective facility’s prevention techniques. The systematic literature review and task force interviews yielded 66 clinical, organizational, and cultural practices for preventing WSB. Of those, 53 pertained to care processes before, during, and after nerve block administration. The remaining 13 practices pertained to the environment of a health care facility's structure and culture of safety.
Principles Promote Prevention. The collaborative team collated the 66 WSB prevention practices and used them to develop a survey. The task force members reviewed the practices and rated their level of agreement with each practice's potential for preventing WSB using a five-point scale (ie, strongly agree, agree, neutral, disagree, and strongly disagree). The task force achieved consensus regarding the practices during two meetings and unanimously approved a final set of 21 principles. The Principles for Reliable Performance of Correct-Site Nerve Blocks proposed 12 Process of Care practices and 9 Health Care Facility Structure and Culture of Safety practices (Figure 2).
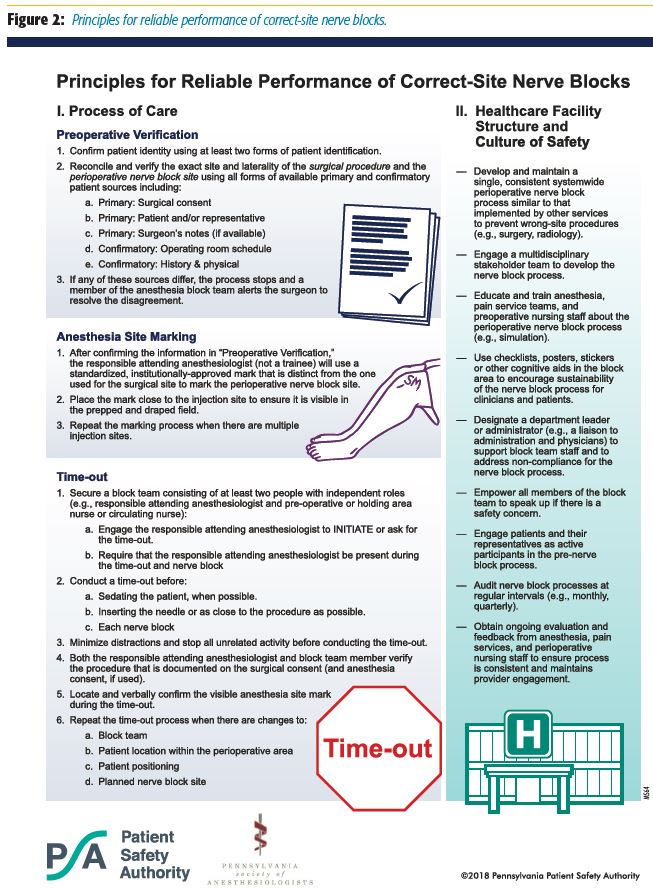
Although professional organizations have previously published recommendations for preventing wrong-site procedures, including those specific to nerve blocks,[4–7] the consensus-based, peer-driven 21 principles resulting from this collaboration are unique compared with other guidelines and statements. The principles:
- Demonstrate a successful collaborative partnership between a medical professional society and an independent state agency.
- Take advantage of the diverse training, culture, and perspectives of a multidisciplinary task force that included patients, pain service nurses, surgeons, and anesthesiologists.
- Reflect data from a robust state-based event reporting system (ie, PA-PSRS) that demonstrated the continued prevalence of WSB in clinical practice.
- Use primary and confirmatory preoperative data sources, including patients, to verify the exact location and laterality of the surgical site.
- Describe specific site-marking and time-out procedures based on needs identified in past or current practice.
- Consider the unique environment and culture in which nerve blocks are performed to promote successful implementation and sustainability of clinical processes.
Summary
WSBs accounted for about one-quarter of all wrong-site procedures reported to PA-PSRS between July 2004 and September 2017. In an attempt to reduce their incidence, the society and the authority identified a set of 21 principles—12 related to clinical practices and 9 specific to environmental and cultural improvements— to help facilities sustain and implement the clinical practices. Anesthesiologists are encouraged to review the peer-driven principles and work with their health care organizations to incorporate them as standard surgical-safety practices.
References
- Pennsylvania Patient Safety Authority. 2016 Pennsylvania Patient Safety Authority Annual Report. Harrisburg, Pennsylvania: Pennsylvania Patient SafetyAuthority; 2017. Available at: http://patientsafety.pa.gov/PatientSafetyAuthority/ Documents/annual_report_2016.pdf. Accessed July 3, 2018.
- Deutsch ES, Yonash RA, Martin DE, Atkins JH, Arnold TV, Hunt CM. Wrong-site nerve blocks: a systematic literature review. J Clin Anesth. 2018;46:101–111.
- Hudson ME, Chelly JE, Lichter JR. Wrong-site nerve blocks: 10 yr experience in a large multihospital health-care system. Br J Anaesth. 2015;114(5):818–824.
- World Health Organization. WHO Guidelines for Safe Surgery: 2009. Geneva, Switzerland: World Health Organization; 2009. http://apps.who.int/iris/ bitstream/10665/44185/1/9789241598552_eng.pdf
- French J, Bedforth N, Townsley P. Stop before you block campaign. Nottingham, UK: Nottingham University Hospitals. Available at: https://www.rcoa.ac.uk/sites/default/files/CSQ-PS-sbyb-supporting.pdf. Accessed July 3, 2018.
- Mulroy MF, Weller RS, Liguori GA. A checklist for performing regional nerve blocks. Reg Anesth Pain Med. 2014;39(3):195–199.
- Joint Commission. Universal Protocol. Oakbrook Terrace, Illinois: Joint Commission; 2018. Available at: https://www.jointcommission.org/standards_ information/up.aspx. Accessed July 3, 2018.
Acknowledgments
The authors would like to acknowledge the contributions of the following Authority and Society team members:
Pennsylvania Patient Safety Authority:
- Ellen Deutsch, MD, MS, FACS, FAAP
- Christina Hunt, MBA, MSN, HCM, RN, CPPS, LBBH
- Robert Yonash, RN, CPPS
Pennsylvania Society of Anesthesiologists
- Joshua H. Atkins, MD, PhD, University of Pennsylvania
The authors would also like to acknowledge the contributions of the following members of the Pennsylvania Correct-Site Nerve
Block Task Force:
Anesthesiologists
- Nabil Elkassabany, MD, University of Pennsylvania
- Michael Entrup, MD, Geisinger Medical Center
- Joseph Galassi, MD, Lehigh Valley Health System
- Arjunan Ganesh, MBBS, FRCS, Children's Hospital of Philadelphia and University of Pennsylvania
- Mark Hudson, MD, University of Pittsburgh
- Kristin Ondecko-Ligda, MD, University of Pittsburgh
- Bryan Matusic, DO, Advanced Surgical Hospital, Washington, Pennsylvania
- Laura Schleelein, MD, Children's Hospital of Philadelphia and University of Pennsylvania
- Mark Taylor, MD, Allegheny Health System
Pain Service Nurses
- Debbie Brickley, RN, Acute Pain Service Nurse, UPMC Mercy
- Beverly Kantz, RN, Director of Perioperative Care and Pain Management, Meadville Medical Center
- Christine Kreider, RN, Acute Pain Service Nurse, Penn State Health
Patient Representatives
- Mary Ellen Mannix, Philadelphia, Pennsylvania
- Dwight McKay, Lancaster, Pennsylvania
Consultants and Anesthesiologists With Expertise in Chronic Pain
- Vitaly Gordin, MD, Director of the Pain Management Service, Penn State Health
- Kieran Slevin, MD, Private Practice Pain Management Specialist affiliated with the University of Pennsylvania
Surgeons
- April Armstrong, MD, Orthopaedic Surgeon, Penn State Health
- Randy Hauck, MD, Plastic Surgeon, Penn State Health
- John Potochny, MD, Plastic Surgeon, Penn State Health
- Douglas Wisner, MD, Ophthalmologist, Wills Eye Hospital, Philadelphia
Leave a commentOrder by
Newest on top Oldest on top