How I Do It: Serratus Anterior Plane Block for Rib Fractures
Rib fractures are common following blunt trauma,[1] and morbidity increases with age.[2,3] Prompt analgesia after injury may prevent pulmonary complications such as atelectasis, pneumonia, mechanical ventilation, or intensive care unit admission because it stops the sequelae of altered respiratory mechanics, which normally peak at 48–72 hours post injury.[2] However, excessive use of opioids to manage pain often leads to hypoventilation and inadequate secretion clearance because of cough inhibition, compounding the likelihood of developing adverse respiratory complications.[2] Combined with the current era of opioid abuse, physicians are increasingly searching for opioid-sparing analgesic techniques.[4]
Fascial plane blocks (serratus anterior plane block, erector spinae plane block) are alternative regional techniques that provide good pain control while expanding the spectrum of patients who might benefit.
The Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society guidelines recommend epidural and multimodal analgesia as best practices to treat rib fracture pain.[5] However, trauma patients frequently have contraindications to neuraxial anesthesia, including restricted mobility, altered cognition, increased intracranial pressure, and coagulopathy. Fascial plane blocks (serratus anterior plane [SAP] block, erector spinae plane [ESP] block) are alternative regional techniques that provide good pain control while expanding the spectrum of patients who might benefit.[6] The SAP block with catheter placement is favored at our center because of its enhanced safety profile (versus neuraxial) and ease of performance with the patient supine.[7]
Clinical Anatomy of Sap Block
Initially intended to provide analgesia for breast surgery,[8] the SAP block was quickly found to be effective for rib fracture pain[9,10] while improving spirometry volumes[7] and allowing for continuous analgesia with catheter insertion.[11]
The block targets the lateral cutaneous branches of the T2–T9 intercostal nerves. At the midaxillary line, the lateral cutaneous nerve penetrates the external intercostal and serratus anterior muscles before dividing into anterior and posterior divisions (Figure 1), which innervates the anterolateral chest wall (Figure 2).[12,13]
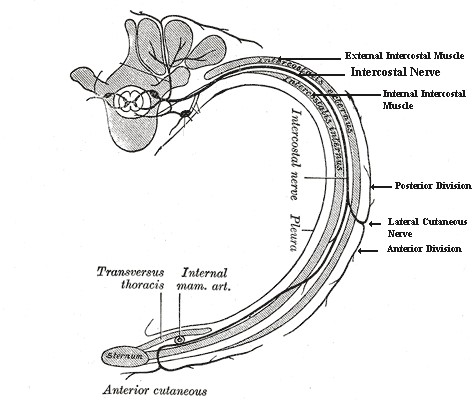 Figure 1: Each intercostal nerve gives off a lateral cutaneous branch around the midaxillary line, which further divides into anterior and posterior divisions
Figure 1: Each intercostal nerve gives off a lateral cutaneous branch around the midaxillary line, which further divides into anterior and posterior divisions
Reprinted from Gray H, Lewis WH. Anatomy of the Human Body. 20th ed. Philadelphia, PA: Lea & Febiger; 1918.
In addition, the long thoracic nerve (LTN), thoracodorsal nerve (TDN), and thoracodorsal artery lie in the fascial plane superficial to the serratus anterior muscle (SAM), between SAM and the latissimus dorsi muscles.[13] The thoracodorsal artery runs with the thoracodorsal nerve and serves as a landmark for the appropriate level of blockade at the midaxillary line, targeting ribs 4 and 5. The LTN provides motor supply to the serratus anterior muscle, assisting with scapular abduction.
The mechanism by which the SAP block produces analgesia for rib fractures is an ongoing area of study.[12,14] Unlike the original SAP block for breast analgesia, which blocks the anterolateral chest wall,[15] the SAP for rib fracture analgesia has been found clinically to provide anterolateral[10] and posterior analgesia.[16] The mechanism is likely due to rib trauma, because the disrupted tissue planes appear to facilitate spread of injectate through the muscle planes to the intercostal nerves, allowing for posterior coverage.[14]
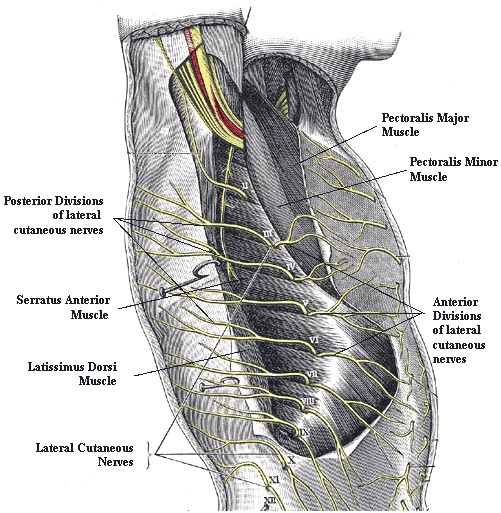
Figure 2: The posterior and anterior divisions of the lateral cutaneous nerves penetrate the serratus anterior muscle to innervate the antero-lateral thorax. The nerves lie in the tissue plane between the serratus anterior and the latissimus dorsi muscles.
Reprinted from Gray H, Lewis WH. Anatomy of the Human Body. 20th ed. Philadelphia, PA: Lea & Febiger; 1918.
The Ottawa Hospital Experience
Regional anesthesia is one component of the multimodal management of rib fracture pain, particularly in the setting of multisystem trauma. We developed a pathway to guide clinicians with this management (Figure 3). If the rib fracture score is greater than 6 or the patient requires supplemental oxygen, the acute pain service is consulted. If a regional anesthetist is not readily available, the patient may be started on a lidocaine or ketamine infusion with a hydromorphone patient-controlled anesthesia, in addition to oral foundational analgesics. In cases where the patient is intubated on admission, the SAP catheter can be inserted to facilitate ventilator weaning in the intensive care unit.
Description of Technique
Obtain written consent from the patient prior to the procedure. If the patient is intubated, obtain verbal or written consent from the next of kin. Following informed consent, apply standard monitors and ensure intravenous access. Pressure from the ultrasound probe and needling may increase pain with anterolateral fractures. To mitigate this, give preprocedure sedation. A major advantage of the SAP block for rib fractures is the lack of patient repositioning. Keep the patient supine with gentle abduction of the arm to expose the anterior axillary area. Elevating the head of the bed approximately 30 degrees can be beneficial to prevent operator fatigue and improve respiratory mechanics.
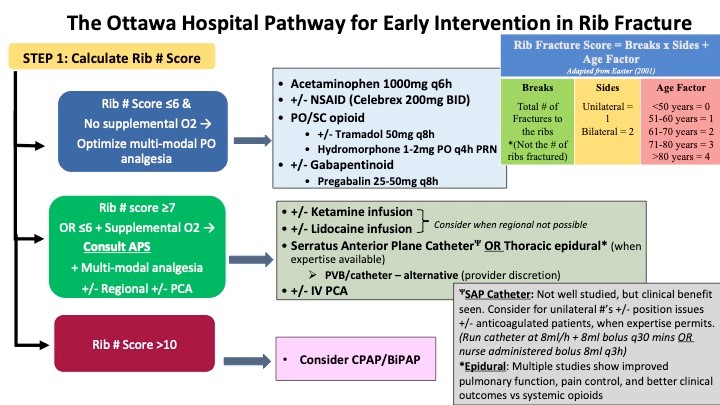
Figure 3. Rib Fracture Pain Management Pathway, utilized by the Acute Pain Service at The Ottawa Hospital, Ottawa, ON, Canada.
Using a high-frequency linear probe oriented in the sagittal plane, obtain an infraclavicular view in the midclavicular line. The second rib will be visible posterior and just caudal to the axillary vessels (Figure 4). Rotate the probe parallel to the deltopectoral groove (Figure 5). Slide the probe caudally and laterally along the groove to rib 3. To improve visualization of the ribs, tilt the probe medially (Figure 6), and continue sliding to ribs 4 and 5. Note that the pectoralis major and minor muscles will taper off as you slide laterally (Figure 7). At the anterior to midaxillary line over rib 5, SAM is clearly visible superficial to the ribs. Overlying SAM is the latissimus dorsi muscle (Figure 8). If a patient has a chest tube dressing in the way, this can easily be removed and a new one replaced at the end of the procedure.
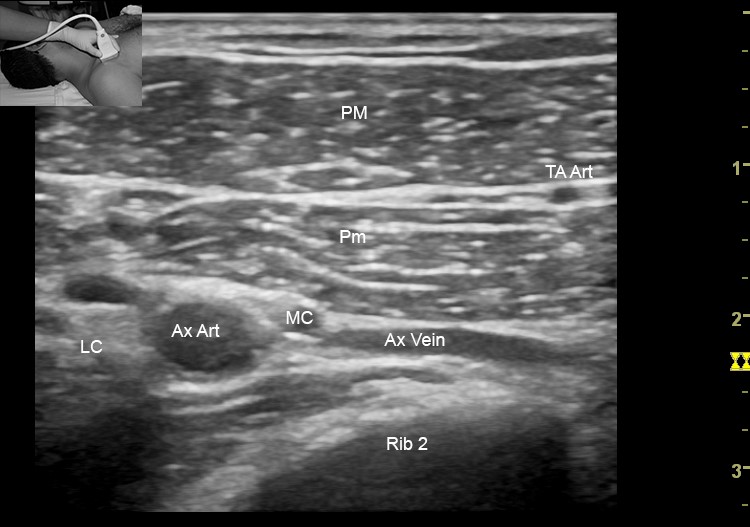 Figure 4: Infraclavicular view at the midclavicular line. The second rib is the first visible rib, just below and caudal to the axillary vessels. Note the axillary vein is collapsed due to probe pressure. Ax Art, axillary artery; Ax Vein, axillary vein; LC, lateral cord; MC, medial cord; PM, pectoralis major muscle; Pm, pectoralis minor muscle; TA Art, thoraco-acromial artery in the plane between the pectoralis muscles.
|
PM, pectoralis major muscle; Pm, pectoralis minor muscle.
|
IC, intercostal muscles; PM, pectoralis major muscle; Pm, pectoralis minor muscle; SA, serratus anterior muscle.
|
IC, intercostal muscles; SA, serratus anterior muscle.
|
IC, intercostal muscles; LD, latissimus dorsi muscle; SA, serratus anterior muscle.
|
LD, latissimus dorsi muscle; SA, serratus anterior muscle; TA, thoracodorsal artery. |
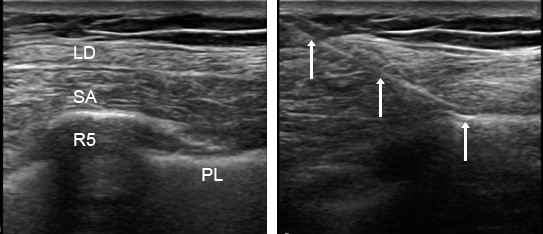
Figure 10: Image demonstrates inplane insertion of a Tuohy needle through the latissimus dorsi and serratus anterior muscle onto the rib surface.
LD, latissimus dorsi muscle; SA, serratus anterior muscle; arrows, needle.
We typically target the rib level that corresponds to the middle of the range of fractured ribs. For example, if ribs 4–8 are fractured, we target rib 6. Use the colour-flow function to identify vascular structures in the planned needle trajectory path. The thoracodorsal artery may be visible at this level between the latissimus dorsi and SAM (Figure 9). After skin infiltration, insert the needle in plane from an anterocranial to posterocaudal direction. The needle should be directed toward the rib to minimize inadvertent pleural puncture. Our usual endpoint is the needle tip on the rib deep to SAM (Figure 10).
The tissue plane superficial to SAM is an alternate target. However, older trauma patients often have thin SAM and muscle planes that can be obscured by air, hematomas, or chest tubes, making it simpler to target the rib underlying SAM as the endpoint. Additionally, injection of local anesthetic deep to SAM may prevent LTN blockade because the nerve lies on the superficial surface of SAM.[15]
Once the needle contacts the rib, decrease the angle and advance it slightly to ensure the needle opening is completely below the muscle. Use small boluses of fluid to hydrodissect along the rib, then fill the plane with local anesthetic observing for SAM elevation and linear fluid spread along the intercostal space to the adjacent rib (Figure 6). Insert the catheter after the plane is opened.
As with all plane blocks, volume is essential, particularly for multiple rib fractures. We deposit 20–40 mL of 0.5% ropivacaine with epinephrine 1:400,000 under the serratus muscle. A lower concentration (0.25%) may be used when bilateral blocks are required or the patient weight dictates. Two separate injections of 20 mL have been shown to achieve greater cephalocaudad spread in cadavers compared to a single 20 mL injection. The larger volume achieved a dye spread of four to seven levels.[15] Clinically, because we always insert a catheter, we perform one injection and adjust the initial volume of injection based on the number of ribs fractured. An initial bolus volume of 30 mL will typically achieve excellent analgesia in a patient with six levels of fractures.
We infuse 0.2% ropivacaine at the maximum rate of our pump (8 mL/hr), with an 8 mL bolus every 30 minutes. Because patients are often unable to push the bolus button, we order RN boluses every three hours to theoretically optimize local anesthetic spread.[17]
Ongoing Management
The acute pain service performs daily ward rounds on rib fracture patients in the trauma unit or intensive care unit. Adjunctive oral and intravenous medications are adjusted as required. We perform SAP catheters for all rib fracture locations (anterior and posterior) and have found the degree of analgesia provided by the SAP catheter can aid in weaning patients off the ventilator, in addition to facilitating ambulation and chest physiotherapy. Select patients with isolated rib fractures may receive analgesia on an ambulatory basis.[18]
References
- Bulger EM, Arneson MA, Mock CN, Jurkovich G J. Rib fractures in the elderly. J Trauma. 2000;48(6):1040–1046; discussion 1046–1047. https://doi.org/10.1097/00005373-200006000-00007
- May L, Hillermann C, Patil S. Rib fracture management. BJA Educ. 2016;16(1):26–32. https://doi.org/10.1093/bjaceaccp/mkv011
- Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54(3):478–485. https://doi.org/10.1097/01.TA.0000037095.83469.4C
- Wu CL, King AB, Geiger TM, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative joint consensus statement on perioperative opioid minimization in opioid-naïve patients. Anesth Analg. 2019;129(2):567–577. https://doi.org/10.1213/ANE.0000000000004194
- Galvagno SM, Smith CE, Varon AJ, et al. Pain management for blunt thoracic trauma: a joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J Trauma Acute Care Surg. 2016:81(5);936– 951. https://doi.org/10.1097/TA.0000000000001209
- Thiruvenkatarajan V, Cruz Eng H, Adhikary SD. An update on regional analgesia for rib fractures. Curr Opin Anaesthesiol. 2018;31(5):601–607. https://doi.org/10.1097/ACO.0000000000000637
- Hernandez N, de Haan J, Clendeninn D, et al. Impact of serratus plane block on pain scores and incentive spirometry volumes after chest trauma. Local Reg Anesth. 2019;12:59–66. https://dx.doi.org/10.2147%2FLRA.S207791
- Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107–1113. https://doi.org/10.1111/anae.12344
- Durant E, Dixon B, Luftig J, Mantuani D, Herring A. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2017;35(1):197.e3–197.e6. https://doi.org/10.1016/j.ajem.2016.07.021
- Kunhabdulla NP, Agarwal A, Gaur A, et al. Serratus anterior plane block for multiple rib fractures. Pain Physician. 2014;17(4):E651– E653. https://www.painphysicianjournal.com/current/pdf?article=MjE0MQ%3D%3D&journal=83
- Bossolasco M, Bernardi E, Fenoglio, L. Continuous serratus plane block in a patient with multiple rib fractures. J Clin Anesth. 2017;38:85–86. https://doi.org/10.1016/j.jclinane.2016.12.015
- Mayes J, Davison E, Panahi P, et al. An anatomical evaluation of the serratus anterior plane block. Anaesthesia. 2016;71(9):1064–1069. https://doi.org/10.1111/anae.13549
- Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB. Perioperative breast analgesia: a qualitative review of anatomy and regional techniques. Reg Anesth Pain Med. 2017;42(5):609–631. https://doi.org/10.1097/AAP.0000000000000641
- Johnston DF, Black ND, O’Halloran R, Turbitt LR, Taylor SJ. Cadaveric findings of the effect of rib fractures on spread of serratus plane injections. Can J Anesth. 2019;66(6):738–739. https://doi.org/10.1007/s12630-019-01340-9
- Biswas A, Castanov V, Li Z, et al. Serratus plane block: a cadaveric study to evaluate optimal injectate spread. Reg Anesth Pain Med. 2018;43(8):854–858. https://doi.org/10.1097/AAP.0000000000000848
- Rose P, Ramlogan R, Sullivan T, Lui A. Serratus anterior plane blocks provide opioid-sparing analgesia in patients with isolated posterior rib fractures: a case series. Can J Anaesth. 2019;66(10):1263–1264. https://doi.org/10.1007/s12630-019-01431-7
- Ilfeld BM, Gabriel RA. Basal infusion versus intermittent boluses for perineural catheters: should we take the ‘continuous’ out of ‘continuous peripheral nerve blocks’? Reg Anesth Pain Med. 2019;44:285–286. https://doi.org/10.1136/rapm-2018-100262
- Rose P, Ramlogan R, Madden S, Lui A. Serratus anterior plane block home catheter for posterior rib fractures and flail chest. Can J Anesth. 2019;66(8):997–998. https://doi.org/10.1007/s12630-019-01383-y
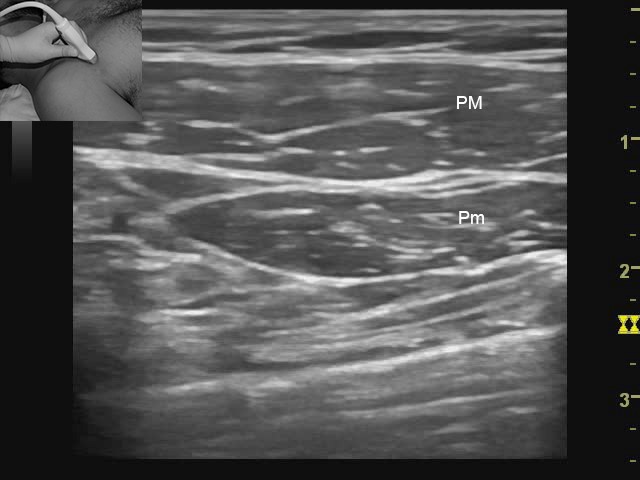 Figure 5: The probe is rotated along the delto-pectoral groove (see inset). From here, the probe slides along the antero-lateral thorax towards the axilla, while counting the ribs
Figure 5: The probe is rotated along the delto-pectoral groove (see inset). From here, the probe slides along the antero-lateral thorax towards the axilla, while counting the ribs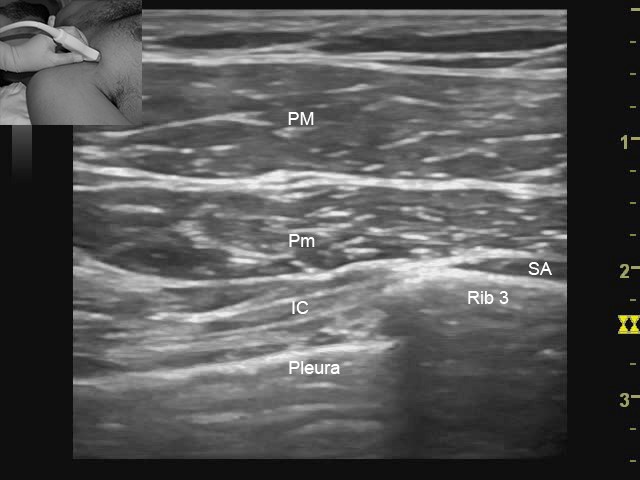 Figure 6: If the ribs are not visible when sliding parallel to the delto-pectoral groove, tilting the probe medially (see inset) will regain visualization of the ribs. The medial edge of the serratus can be seen coming into view on the surface of the 3rd rib
Figure 6: If the ribs are not visible when sliding parallel to the delto-pectoral groove, tilting the probe medially (see inset) will regain visualization of the ribs. The medial edge of the serratus can be seen coming into view on the surface of the 3rd rib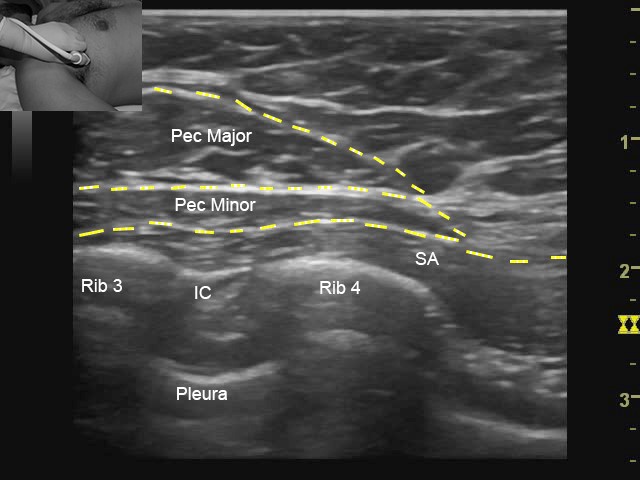 Figure 7: At the level of the 4th rib at the anterior axillary line, the pectoralis muscles can be seen to taper off, as the serratus muscle size increases.
Figure 7: At the level of the 4th rib at the anterior axillary line, the pectoralis muscles can be seen to taper off, as the serratus muscle size increases.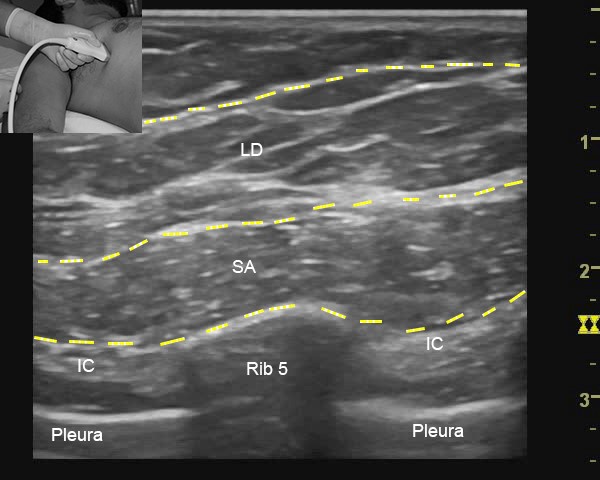 Figure 8: Continuing to slide the probe laterally and caudad towards the mid-axillary line, the latissimus dorsi is seen overlying the serratus muscle
Figure 8: Continuing to slide the probe laterally and caudad towards the mid-axillary line, the latissimus dorsi is seen overlying the serratus muscle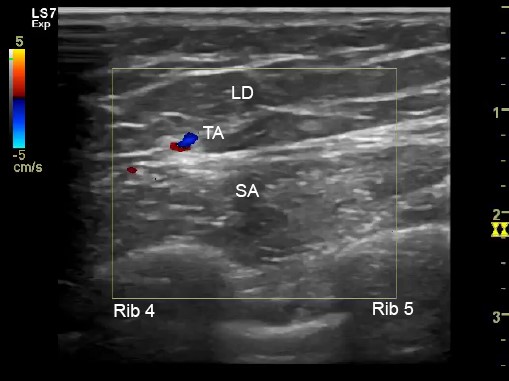 Figure 9: Colour Doppler aids in identifying muscle planes between the latissimus dorsi and serratus anterior muscles, as well as planning needle trajectory to avoid the thoracodorsal artery
Figure 9: Colour Doppler aids in identifying muscle planes between the latissimus dorsi and serratus anterior muscles, as well as planning needle trajectory to avoid the thoracodorsal artery
Leave a commentOrder by
Newest on top Oldest on top