Oxygenation Strategies in COVID-19
In December of 2019, a novel respiratory illness, COVID-19, was first identified and reported.[1] As of June 1, 2020, there have been over 6.2 million cases and 370,000 deaths worldwide including approximately 1.8 million cases and more than 100,000 deaths in the United States from COVID-19.[2] COVID-19 infections have been reported in 188 countries. Case fatality has been reported as high as 16.2% with a case fatality rate of 5.8% in the US.[3] Five to twenty percent of patients with COVID-19 require critical care services, and early reports note that 71-88% of patients may require intubation and mechanical ventilation.[4-7] For patients requiring intensive care unit (ICU) admission, mortality increases to 26-62%.[5-9]
In our experience, we were able to postpone or, in some instances, avoid intubation with the use of helmet ventilation.
COVID-19, the disease caused by SARS-CoV-2, is characterized by fever, chills, malaise, fatigue, chest pain, shortness of breath, headache, and GI symptoms (nausea, vomiting, and diarrhea).[10-11] COVID-19 can also result in acute kidney injury, coagulation abnormalities, and cytokine storm. In more severe cases, COVID-19 is associated with significant hypoxia secondary to viral pneumonia and acute respiratory distress syndrome (ARDS). Laboratory hallmarks include lymphopenia, elevations in inflammatory markers (i.e. CRP, ferritin, IL-6), elevated coagulation studies (i.e. D-dimer), and abnormal troponin levels.[11] Radiographic studies reveal bilateral patchy opacities with ground glass appearance on CT scan.[12]
COVID-19-related hypoxia is associated with an increased alveolar-arterial (A-a) oxygen gradient.[13] Common causes of increased A-a gradient include ventilation-perfusion (V/Q) mismatch and intra-pulmonary shunt. Patients with predominant shunt physiology will not have significant increases in saturations or PaO2 with delivery of supplemental oxygen. The lack of response to oxygen may trigger a lower threshold for early intubation and mechanical ventilation.[13] Patients with predominantly V/Q mismatch will respond to higher levels of FiO2, which can allow for treatment with noninvasive oxygenation and ventilation.
Initial management of critically ill patients with COVID-19 within our institution as well as many others called for early intubation for hypoxia related to ARDS.[11,14-15] Intubation allows for more precise delivery of oxygen and control of tidal volumes and respiratory pressures. However, intubation and mechanical ventilation have drawbacks including need for sedation to promote ventilator synchrony, sedation-related hypotension, potential need for paralysis, ventilator associated infections, and ventilator-induced lung injury (VILI).[16] In addition, intubation is considered an aerosol-generating procedure, which may increase risks of viral transmission to those present and performing the procedure.[17]
While randomized, controlled studies are lacking in COVID-19-related ARDS, multiple strategies of noninvasive oxygen delivery and ventilation have been investigated prior to the appearance of SARS-CoV-2. For patients with moderate to severe non-hypercarbic respiratory failure (PaO2 < 200 mmHg), high-flow nasal cannula (HFNC) has been shown to prevent intubation and be associated with decreased ICU and 90-day mortality.[18] Similarly, noninvasive ventilation strategies have been associated with decreased rate of intubation and lower ICU mortality in hypoxic respiratory failure.[19-20] For patients with ARDS who ultimately fail non-invasive ventilation (NIV) and require intubation, there has been no difference in mortality for those who experienced early vs late intubation.[21]
Given concerns for potential need for rationing of resources (ie, ventilators, ICU beds) and high morbidity and mortality in intubated and mechanically ventilated patients, we pivoted our strategy to include the use of noninvasive ventilation and oxygenation modalities in late March 2020. [8,22-23] All patients requiring supplemental oxygen greater than 6 liters per minute (lpm) were transferred to the ICU where patients were started on HFNC. Patients with continued hypoxia but without signs or symptoms of respiratory distress received a trial of alternative NIV (ie, Helmet, CPAP, BiPAP). For those with a P:F ratio of < 150, we encouraged patients to position themselves prone to improve oxygenation and attempt to avoid intubation.[24-26] Patients with subjective shortness of breath or who had clinical signs or symptoms of respiratory distress were intubated and started on mechanical ventilation, which often subsequently required high levels of sedation, paralysis, and proning. The mortality outcomes in our intubated patients have been statistically similar whether intubated early or after a trial of HFNC or NIV as has been previously reported by Thille et al.[21]
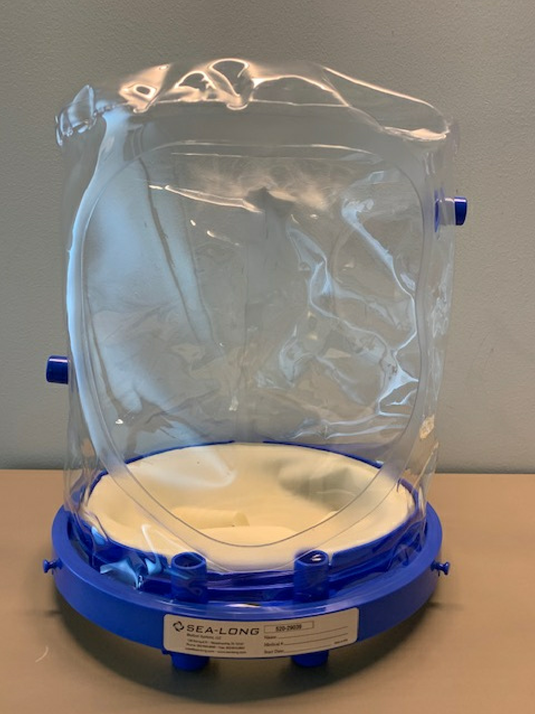 Figure 1: Helmet ventilation system
Figure 1: Helmet ventilation system
In our experience, we were able to postpone or, in some instances, avoid intubation with the use of helmet ventilation. The helmet system consists of a polyvinyl chloride latex-free hood and neck seal (Figure 1). The hood is placed over the patient’s head and connected to a ventilator or high-flow oxygen/medical air supply via the inspiratory port. A PEEP valve is placed on the expiratory port to provide positive pressure to prevent against atelectasis. A viral filter also may be placed on the expiratory side to prevent viral transmission in respiratory illnesses. The helmet system also may decrease the risk of transmission by providing a barrier to droplet spread.
A potential disadvantage of using NIV and HFNC is the increased risk of aerosolization of particles. Flow rates as high as 60 lpm utilized by HFNC have resulted in limited use in some institutions because of concern for transmission of viral infection.[5] The use of HFNC at 60 lpm does generate more aerosolization than HFNC at 10 lpm. Studies have shown that even at 60 lpm, the degree of aerosolization may be equivalent to or less than the risk of aerosolization with simple facemask, non-rebreather, or Venturi masks.[27-29] In order to decrease viral spread, the patient may wear a surgical mask over HFNC. Less data is available regarding aerosolization with the use of BiPAP/CPAP and helmet ventilation, but risk can be minimized by using expiratory filters and maintaining an adequate seal.
Given the use of HFNC and NIV in our COVID cohort units, multiple strategies were employed to minimize the risk of virus transmission. Two floors of our institution were converted into negative pressure environments for COVID-19 patients. Given concerns of aerosolization with the use of multiple devices within the ICU, staff working within the cohort units were encouraged to wear N95, N100, or PAPR along with eye shields while in the unit even outside of patient rooms. Occupational medicine enacted widespread fit testing for reusable half facepiece respirators with P100 filters for extended use in the cohort units as well as for other aerosolizing procedures (ie, intubations in the OR), which has led to preservation of N95 masks.
With the emergence of a novel respiratory infection, we have been challenged to reassess our typical management of ARDS. Due to potential and actual shortages of ventilators and ICU beds throughout the world, patients with ARDS have been treated with HFNC and NIV with some success in avoiding intubation and mechanical ventilation and preventing the need to ration scarce resources during a global pandemic.
References
- Ludwig S, Zarbock A. Coronaviruses and SARS-CoV-2: A brief overview. Anes Analg. 2020; 10.1213/ANE. 0000000000004845.
- Johns Hopkins University. COVID-19 dashboard by the Center for Systems and Engineering (CSSE) at Johns Hopkins University.” Available at: https://coronavirus.jhu.edu/map.html. Accessed May 28, 2020.
- Johns Hopkins University. Mortality analyses. Available at: https://coronavirus.jhu.edu/data/mortality. Accessed June 2, 2020.
- Ziehr DR, Alladina J, Petri CR, et al. Respiratory pathophysiology of mechanically ventilated patients with COVID-19: A cohort study. Am J Respir Crit Care Med 2020;201(12)1560-4. doi: 10.1164/rccm.202004-1163LE.
- Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020; 323:1612-4. doi: 10.1001/jama.2020.4326
- Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020;323:1574-81. doi: 10.1001/jama.2020.5394.
- Yang X, Yu Y, Xu J et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8(5)475-81. doi: 10.1016/S2213-2600(20)30079-5.
- Auld SC, Caridi-Scheible M, Blum JM, et al. ICU and ventilator mortality among critically ill adults with coronavirus disease 2019. Crit Care Med 2020 May 26 [online ahead of print]. doi: 10.1097/CCM.0000000000004457.
- Bhatraju PK, Ghassemieh BJ, Nichols M, et al. COVID-19 in critically ill patients in the Seattle region – case series. N Engl J Med 2020;382(21):2012-22.
- Guan WJ, Ni Zy, Hu Y, et al. Clinical characteristics of coronavirus disease in 2019 in China. N Engl J Med 2020;382:1708-20. doi: 10.1056/NEJMoa2002032.
- Sommer P, Lukovic E, Fagley E, et al. Initial clinical impression of the critical care of COVID-19 patients in Seattle, New York City, and Chicago. Anesth Analg 2020;131:55-60. doi: 10.1213/ANE.0000000000004830.
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020; 20(4);425-34. doi: 10.1016/S1473-3099(20)30086-4
- Tobin MJ. Basing respiratory management of coronavirus on physiological principles. Am J Respir Crit Care Med 2020;201:1319-20. doi: 10.1164/rccm.202004-1076ED
- Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med 2020;382:2372-4. doi: 10.1056/NEJMc2010419.
- Richardson S, Hirsch JS, Narasimhan M et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 2020;323(20)2052-9. JAMA. doi: 10.1001/jama.2020.6775.
- Gattinoni L, Marini JJ, Collino F, et al. The future of mechanical ventilation: lessons from the present and past. Crit Care 2017;21(183) doi: 10.1186/s13054-017-1750-x
- Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 2012; 7(4):e35797. doi: 10.1371/journal.pone.0035797.
- Frat J, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015;372(23):2185-96. doi: 10.1056/NEJMoa1503326.
- Antonelli M, Conti G, Esquinas A, et al. A Multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med 2007;35(1):18-25. doi: 10.1097/01.CCM.0000251821.44259.F3
- Patel BK, Wolfe KS, Pohlman AS, et al. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 2016;315(22):2435-41. doi: 10.1001/jama.2016.6338.
- Thille AW, Contou D, Fragnoli C, et al. Non-invasive ventilation for acute hypoxemia respiratory failure: intubation rate and risk factors. Crit Care 2013;17(6):R269. doi: 10.1186/cc13103.
- Hanidziar D, Bittner EA. Sedation of mechanically ventilated COVID-19 patients: challenges and special considerations. Anesth Analg 2020. doi:10.1213/ANE.0000000000004887
- Meng L, Qiu H, Wan L et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan's experience. [published online March 26, 2020]. Anesthesiology 2020;132(6)1317-32. doi: 10.1097/ALN.0000000000003296.
- Pelosi P, Brazzi L, Gattinoni L. Prone position in acute respiratory distress syndrome. Eur Respir J 2002;20(4):1017-28. doi: 10.1183/09031936.02.00401702.
- Pérez-Nieto OR, Guerrero-Gutiérrez MA, Deloya-Tomas E, et al. Prone positioning combined with high-flow nasal cannula in severe noninfectious ARDS. Crit Care 2020;24(28)114. doi: 10.1186/s13054-020-2821-y.
- Ding L, Wang L, Ma W, Hangyong H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care;24(1)28. doi: 10.1186/s13054-020-2738-5.
- Hui DS, Chow BK, Lo T, et al. Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks. Eur Respir J 2019;53(4):1802339. doi: 10.1183/13993003.02339-2018.
- Ip M, Tang JW, Hui DS, et al. Airflow and droplet spreading around oxygen masks: a simulation model for infection control research. Am J Infect Control 2007;35(10):684-9. doi: 10.1016/j.ajic.2007.05.007.
- Leung CCH, Joynt GM, Gomersall CD, et al. Comparison of high-flow nasal cannula versus oxygen face mask for environmental bacterial contamination in critically ill pneumonia patients: a randomized controlled crossover trial. J of Hospital Infection 2019;101(1):84-7. doi: 10.1016/j.jhin.2018.10.007.
Leave a commentOrder by
Newest on top Oldest on top