How I Do It: Hip Radiofrequency Ablation
Cite as: Nagpal A. How I do it: hip radiofrequency ablation. ASRA News 2020;45. https://doi.org/10.52211/asra110120.066
Hip joint pain affects 11% of the population.[1] Groin pain, with radiation to the buttocks or upper-outer thigh, is the most common symptomatic complaint from these patients, and often the pain is due to osteoarthritis of the hip.
Future work is needed to identify posterior hip innervation landmarks for prospective denervation.
Several manuscripts have detailed the anatomy of the innervation of the hip joint; Locher et al.[2] published perhaps the first well-written manuscript for understanding innervation from the obturator nerve for purposes of ablation. In this study, 14 cadaver hip joints were studied; the location of the articular branch of the obturator nerve was visualized, and a cartoon was made to demonstrate the location of these nerve projections, along with a prospective radiofrequency ablation target zone. After that dissection, Tinnirello et al. were able to adopt a prior procedure (Kawaguchi et al) to modernize the radiofrequency ablation of the hip joint procedure.[3,4] In this procedure, the obturator articular branch was blocked and ablated at the inferior junction of the ischium and pubis, the so-called “acetabular notch” or “acetabular incisura.” The femoral articular branch was blocked and ablated just below the anterior inferior iliac spine (Figure 1).
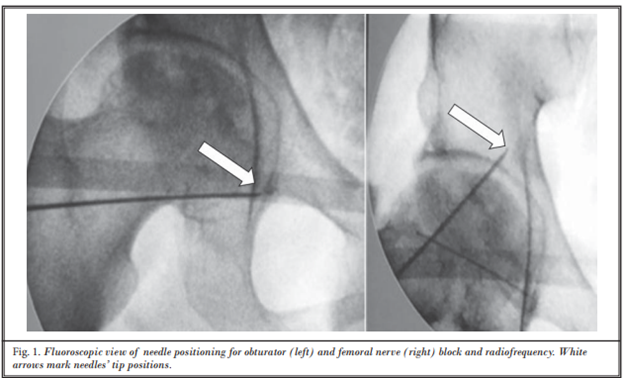
Figure 1: Fluoroscopic view of hip radiofrequency ablation
Reprinted with permission from Tinnirello et al, Pain Physician. 2018;21(4):407-14.
The above history certainly leaves out many important scientists who paved the way toward performing this procedure. But, ultimately, all of that work led to the seminal work by Short et al,[5] who completed the most thorough cadaveric dissection in terms of identifying anatomic landmarks specifically for the purpose of denervating the anterior hip joint. This manuscript confirmed that the acetabular notch and the anterior inferior iliac spine are the most important targets for denervation of the anterior hip joint and also added the iliopubic eminence as a possible target for the accessory obturator nerve. This manuscript also suggested ultrasonographic methods to gain access to these targets.
Based on much of this work, Dr. Kapural’s team published the most recent data and updated method of performing this procedure, and his methodology is the one that I continue to use. Perhaps the most important part of his manuscript is the use of cooled radiofrequency ablation.[6] This allows for creating a larger lesion with forgiveness for not being parallel to the nerve itself, as heat emanates directly from the tip in addition to circumferentially around the active portion of the needle. Dr. Kapural used a combination of ultrasound and fluoroscopy for final needle positioning (Figure 2). Ultimately, a modified version of this technique is the one that I currently use to perform the ablation. I have outlined these steps below:
- Patient is placed in supine position. Fluoroscopy is positioned to obtain a true anterior-posterior view of the femoroacetabular joint (also known colloquially as the “hip joint”).
- Sedation is offered to the patient if we are performing the procedure in an outpatient hospital facility (ie, for cooled radiofrequency ablation). If we are performing the procedure in our outpatient clinic (ie, traditional radiofrequency ablation), sedation is not typically used.
- Ultrasound is used for both locations to ensure that the femoral bundle is not trespassed by the 17-gauge trocar that accompanies cooled radiofrequency ablation kits.
- Local anesthetic is infiltrated to anesthetize the skin and subcutaneous tissues.
- The trocar is brought from lateral to medial for the femoral articular branch, to lay 1-2 cm cephalad to the joint and just inferior to the anterior inferior iliac spine.
- For the obturator articular branch, the trocar is brought from medial to lateral to land on the “teardrop” appearance of the junction of the ischium and pubis inferiorly.
- Stimulation is carried out in the usual manner; I often perform purely motor stimulation up to 2.00 mA to ensure that there is only a local contraction.
- 1 mL of 2% lidocaine is injected in each of the two locations.
- Cooled radiofrequency ablation is performed for 60 seconds on each location.
- 1 mL of 0.5% bupivacaine is injected in each location and the trocars are removed.
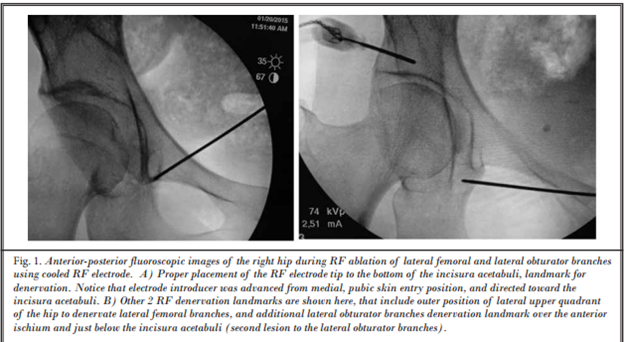
Figure 2: Fluoroscopic view of hip cooled radiofrequency ablation
Reprinted with permission from Kapural et al, Pain Physician. 2018;21(3):279-84.
Future work is needed to identify posterior hip innervation landmarks for prospective denervation. Previous studies have demonstrated that the posterior hip capsule is innervated, potentially, by the sciatic nerve, the superior gluteal nerve, and the nerve to quadratus femoris. Perhaps more pressingly, there are currently no controlled trials demonstrating efficacy of this procedure. It is time for sham-controlled trials to determine the true efficacy of hip articular branch radiofrequency ablation.
References
- ^ Fernandes L, Hagen KB, Bijlsma JW, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72:1125-35.
- ^ Locher S, Burmeister H, Böhlen T, et al. Radiological anatomy of the obturator nerve and its articular branches: basis to develop a method of radiofrequency denervation for hip joint pain. Pain Med. 2008;9(3):291–8.
- Tinnirello A, Todeschini M, Pezzola D, Barbieri S. Pulsed radiofrequency application on femoral and obturator nerves for hip joint pain: retrospective analysis with 12-month follow-up results. Pain Physician. 2018;21(4):407–14.
- Kawaguchi, M, Hashizume K, Iwata T, Furuya H. Percutaneous radiofrequency lesioning of sensory branches of the obturator and femoral nerves for the treatment of hip joint pain. Reg Anesth Pain Med. 2001;26(6):576–81.
- ^ Short AJ, Barnett JJG, Gofeld M, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2018;43:186-92.
- ^ Kapural L, Jolly S, Mantoan J, Badhey H, Ptacek T. Cooled radiofrequency neurotomy of the articular sensory branches of the obturator and femoral nerves - combined approach using fluoroscopy and ultrasound guidance: technical report, and observational study on safety and efficacy. Pain Physician. 2018;21(3):279–84.
Leave a commentOrder by
Newest on top Oldest on top