How I Do It: Suprainguinal Fascia Iliaca Block
Cite as: Amato PE, Thames MR. How I do it: suprainguinal fascia iliaca block. ASRA News 2020;45. https://doi.org/10.52211/asra110120.063
Introduction
The suprainguinal fascia iliaca block has evolved as an effective means of providing analgesia to the thigh, the knee, and, most notably, the hip. The sensory innervation of the hip is complex, involving multiple nerves from both lumbar and sacral plexi. Prior studies have demonstrated a dense anterior capsule innervation, involving femoral, obturator, and accessory obturator nerves.[1,2] It is thus no surprise that initial block techniques for hip analgesia targeted the lumbar plexus as the origin of these peripheral nerves; however, psoas compartment blocks and other posterior approaches to the lumbar plexus can be technically challenging and may be associated with a greater risk of complications.[3] Hence, simpler anterior approaches to the plexus were developed almost simultaneously, beginning with Winnie’s “3-in-one” block in 1973,[4] and later Dalens’ “fascia iliaca compartment block” in 1989.[5] As ultrasound technology improved, image-guided versions of these blocks emerged, capitalizing on this shared compartment, and ultimately encouraging spread of the local anesthetic further cephalad into the iliac fossa. The ultrasound-guided suprainguinal fascia iliaca block, described by Hebbard in 2011, further built on earlier anatomic discoveries to more reliably anesthetize the 3 nerves originally targeted by Winnie: femoral, lateral femoral cutaneous, and obturator.[6] This relatively simple block has most notably been shown to provide opioid-sparing analgesia in the setting of hip surgery.[7]
The suprainguinal fascia iliaca block can be an effective means of providing analgesia for procedures of the knee or thigh but is perhaps best suited for hip analgesia.
Anatomical Premise
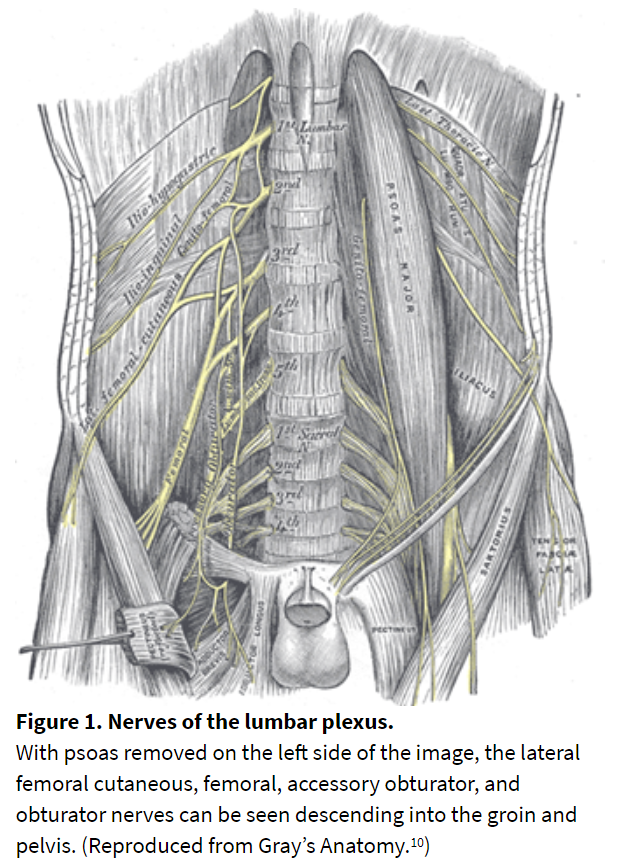
The femoral, lateral femoral cutaneous (LFCN), and obturator nerves all descend from the lumbar plexus into the pelvis and come to share a compartment beneath the fascia iliaca for a short distance (Figure 1). Dalens understood this when he created the original tactile and landmark-based fascia iliaca compartment block. Although the femoral nerve and LFCN were more consistently anesthetized compared to prior methods, subsequent studies have proven that obturator nerve blockade is still unreliable with this technique.[8] This can be explained by both the unpredictability of tactile feel to identify the correct fascial plane and the nature of the lumbar plexus anatomy in the pelvis. The femoral, LFCN, and obturator nerves branch and diverge from one another as they descend toward the inguinal region. The obturator nerve courses posteromedially toward the obturator canal and subsequently splits into anterior and posterior divisions. The LFCN exits the fascia iliaca plane laterally at the level of the inguinal ligament. The femoral nerve remains in this plane but gives off branches to the iliacus and acetabulum prior to reaching the inguinal ligament. It makes sense that, in order to reach these nerves with a single injection, local anesthetic spread well above the inguinal ligament is preferred. The ultrasound-guided suprainguinal approach we describe here does exactly that.
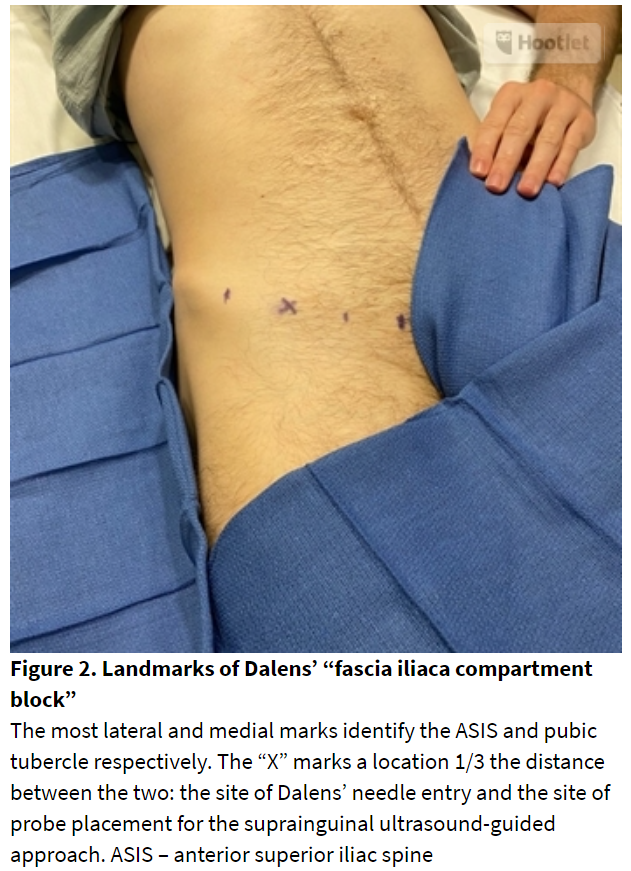
Dalens’ original landmark-based fascia iliaca block begins with a needle entry point 1/3 the distance between the anterior superior iliac spine and the pubic tubercle, along the inguinal ligament (Figure 2). The needle is advanced posteriorly until two “pops” are felt, the first through the fascia lata and the second through the fascia iliaca. This location along the inguinal ligament places the needle somewhere between the femoral and lateral femoral cutaneous nerves and forms the starting location for the ultrasound transducer in the suprainguinal fascia iliaca approach. However instead of injecting at or below the ligament, the needle is directed up into the pelvis, guided by clear visualization of the fascia iliaca as it passes beneath the abdominal wall muscles. The ultrasound-guided suprainguinal approach results in better anesthesia of anterior hip nerves, at least in part due to more reliable obturator blockade compared to landmark techniques.[6,9]
Technique and Sonoataomy
Our approach to the suprainguinal fascia iliaca block is very similar to that described by Hebbard in 2011. The patient is positioned supine with extended hip, and any abdominal pannus is retracted by an assistant or heavy tape. The anterior superior iliac spine (ASIS) is palpated and the ultrasound probe is placed slightly inferior and medial to it (in the vicinity of Dalen’s landmark based approach). Figure 3 shows typical probe positioning over the inguinal ligament. A parasagittal orientation was originally described, but an angle more perpendicular to the inguinal ligament is often preferable. A high-frequency linear ultrasound probe is typically sufficient, although a lower frequency curvilinear probe may be desirable for obese patients, as it is sometimes helpful to begin imaging at sufficient depth to identify the ilium at the bottom of the image.
The iliacus muscle is identified superficial to the ilium, and the hyperechoic fascia iliaca is identified on the superficial border of the muscle. Superficial to the fascia iliaca, one can visualize where the abdominal wall muscles meet those of the lower extremity at the inguinal ligament (Figure 4). The tapered confluence of the internal oblique (cephalad) and the sartorius (caudad) at the inguinal ligament has been described as a bow tie or horizontal hourglass sitting atop the iliacus muscle at the level of the anterior inferior iliac spine (AIIS). Singh described this technique of pattern recognition in 2013, and the authors find it quite useful especially when working with trainees.[11] To confirm location, one may scan along the inguinal ligament to identify the femoral artery medially and then retrace superiorly and laterally to where the anterior inferior iliac spine is seen as a protuberance towards the probe on the ilium. With the probe in this location, small maneuvers of tilt are performed to optimize the visualization of the fascia iliaca. The deep circumflex iliac artery may be identified between the internal oblique and fascia iliaca, and serves as both a landmark and structure to avoid.
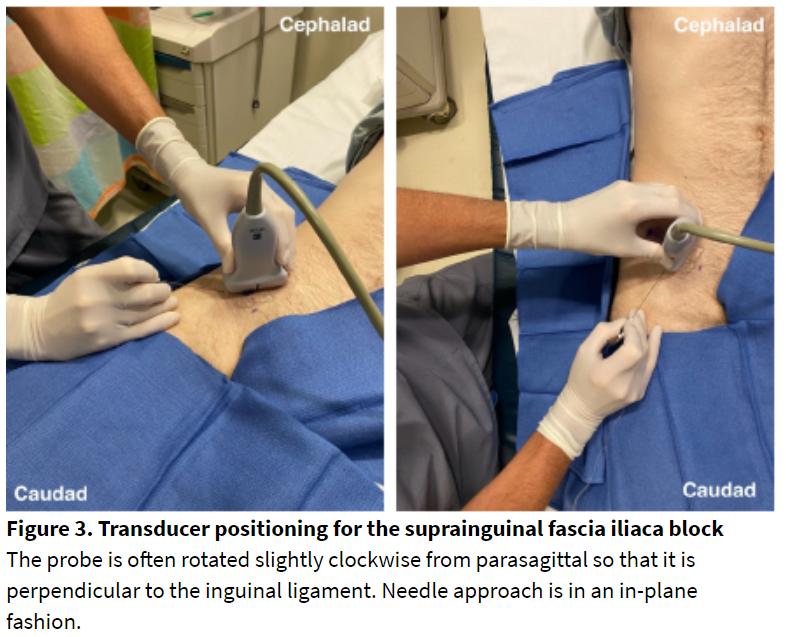
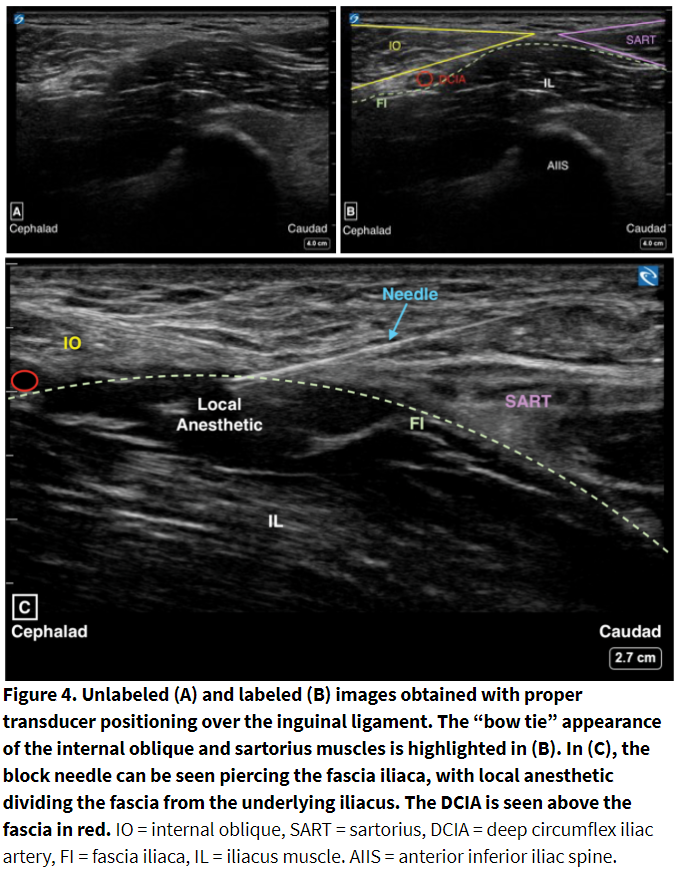
An echogenic B-bevel needle (22g 80 mm most often used at our institution) is inserted with an in-plane technique from the inferior aspect of the probe. Hebbard described entering skin just inferior to the inguinal ligament and reaching the fascia iliaca roughly at the level of the ligament, whereas Desmet entered just superior to the ligament with a significantly steeper angle, which enhances the tactile loss of resistance that is typically felt upon traversing the fascia iliaca and entering the iliacus muscle below.[7] We find either approach acceptable and vary our own based on sonoanatomy visualized and patient body habitus. After the “pop” through fascia iliaca, the needle may need to be withdrawn slightly to rest at the superficial border of the iliacus. Then, 1-2 mL of saline or local anesthetic is injected to confirm spread between the hyperechoic fascia iliaca and the more heterogeneous iliacus muscle beneath it. With appropriate spread, the needle is further advanced into the pocket of local anesthetic, moving in the cephalad direction as the iliacus muscle is hydro-dissected away from the overlying fascia iliaca. Approximately 30-40 ml of volume is usually required to open this potential space and reach the target nerves. At our institution, 0.25% ropivacaine or bupivacaine (with preservative-free dexamethasone for increased duration) is most commonly utilized. As with all regional techniques, it is prudent to aspirate prior to injection and throughout, as well as to consider total local anesthetic doses.
Discussion
The suprainguinal fascia iliaca block can be an effective means of providing analgesia for procedures of the knee or thigh but is perhaps best suited for hip analgesia, for which the authors use the block almost exclusively. It offers the convenience of a single injection site to reliably block the femoral, LFCN, and obturator nerves, while potentially decreasing risk compared to directly targeting the nerves individually. There are several approaches described now in the literature, but we feel the most important shared feature is to inject local anesthetic in a cephalad direction, beneath the iliac fascia, over the iliacus, into the pelvis. A recent video demonstrated a hybrid technique performed at the infrainguinal level, where the femoral nerve is targeted before making a cephalad fascia iliaca injection.[12] This approach is intriguing; however, it is likely more technically challenging due to the combined in and out of plane technique and thus may be less feasible when working with trainees.
With an emerging focus now on techniques that avoid motor blockade, we acknowledge that the suprainguinal block has the downside of causing quadriceps and adductor muscle weakness, and ambulation will be impaired. It is tempting to jump on the bandwagon of novel motor-sparing techniques such as the pericapsular nerve group block described by Girón-Arango et al,[2] which we have anecdotally also found useful to provide analgesia for both hip fracture and hip arthroscopy patients. Cleverly targeting the terminal branches that innervate the hip capsule does avoid weakness but may not provide as comprehensive analgesia in our experience. Time will tell if the suprainguinal fascia iliaca block falls out of favor due to preference for motor-sparing or more targeted alternatives, but a version of this block has been in the regionalist’s armamentarium for many years and arguably should continue to be in the future.
Clinical Pearls
- Start with the ultrasound probe orientated perpendicularly to the inguinal ligament, between the ASIS and the pubic symphysis. Slide toward and away from the ASIS, along the inguinal ligament, until the bow tie or hourglass of the sartorius and internal oblique are visualized.
- The AIIS, rising into view below the iliacus, is also a good indicator of correct left-to-right orientation of the probe.
- It can be difficult to advance the needle into the suprainguinal local anesthetic pocket due to the fascia iliaca’s shallow depth, tensile strength, and the initial flat needle approach. Sliding the probe cephalad prior to needle entry, such that the needle pierces the skin closer to the inguinal ligament, may help provide a better angle for suprainguinal advancement.
- The deep circumflex iliac artery, seen just posterior to the internal oblique, is a helpful marker for local anesthetic spread. The pocket of the local should form below the vessel, above the iliacus, and spread cephalad.
- The anterior border of the iliacus can appear ill-defined compared to the hyperechoic fascia iliaca above it. Ensure the local anesthetic spreads along its anterior edge cephalad to avoid intramuscular injection.
References
- Birnbaum K, Prescher A, Heßler S, Heller KD. The sensory innervation of the hip joint - an anatomical study. Surg Radiol Anat. 1997;19(6):371–5.
- ^ Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43(8):859-63.
- ^ Auroy Y, Benhamou D, Bargues L, et al. Major complications of regional anesthesia in France: The SOS regional anesthesia hotline service. 2002;97:1274-80.
- ^ Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technic of lumbar plexus anesthesia: the “3-in-1 block”. Anesth Analg. 1973;53(6):989-96.
- ^ Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg. 1989;69(6):705-13.
- ^ Hebbard P, Ivanusic J, Sha S. Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia. 2011;66(4):300-5.
- ^ a b Desmet M, Vermeylen K, Van Herreweghe I, et al. A longitudinal supra-inguinal fascia iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg Anesth Pain Med.2017 May/Jun;42(3):327-33.
- ^ Tran DQ, Salinas FV, Benzon HT, Neal JM. Lower extremity regional anesthesia: essentials of our current understanding. Reg Anesth Pain Med. 2019; 44. Online ahead of print. doi: 10.1136/rapm-2018-000019.
- Dolan J, Williams A, Murney E, et al. Ultrasound guided fascia iliaca block: a comparison with the loss of resistance technique. Reg Anesth Pain Med. 2008;33:526–31.
- Carter, HV. 1918. Plate 823: The lumbar plexus and its branches. In: Gray, H. Anatomy of the Human Body, 20th Edition. Revised by Lewis, WH. Philadelphia and New York: Lea and Febiger.
- ^ Singh, Harsimran, Jones, David. Hourglass-Pattern Recognition Simplifies Fascia Iliaca Compartment Block. Reg Anesth Pain Med. 2013;38(5):467-8. doi:10.1097/AAP.0b013e3182a1f772.
- ^ Chin, Ki-Jinn. Ultrasound-Guided Fascia Iliaca Blocks, YouTube, 30 May 2020, youtube.com/watch?v=aAdvQf3Ck7I.
Leave a commentOrder by
Newest on top Oldest on top