Point-of-Care Ultrasound (POCUS) and COVID-19
Cite as: Kalagara H., Panzer OP., Haskins S. Point-of-care ultrasound (POCUS) and COVID-19. ASRA News. 2021;46. https://doi.org/10.52211/asra050121.022
COVID-19 is a disease caused by infection with SARS-CoV-2, a virus that affects multiple organ systems with numerous disease manifestations. COVID-19 has a specific tropism for the lower respiratory tract, and the most common presentation of this disease is viral pneumonia. Computed tomography (CT) is the definitive test for diagnosing COVID-19 pneumonia at any phase, as it is more sensitive than the reverse transcriptase polymerase chain reaction (RT-PCR) test. However, both CT and RT-PCR can be challenging to perform due to limited access or resources. Therefore, bedside assessment with point-of-care ultrasound (POCUS) has been increasingly utilized to aid in diagnosis and management. We will briefly cover the most common POCUS exam findings for COVID-19 using lung ultrasound (LUS) and cardiac ultrasound (FoCUS) (Table 1). Of note, when performing a comprehensive POCUS exam, deep venous thrombosis (DVT) assessment is also recommended due to the pro-thrombotic state induced by the COVID-19 infection.
Table 1. POCUS Protocol in COVID-19: Includes Cardiac, Lung, and Vascular Ultrasound Assessments3
| POCUS | Structure | Assessment | Disease |
|---|---|---|---|
| Cardiac (FoCUS) | LV | Size and function | Myocarditis Cardiomyopathy Heart failure |
| RV | Size and function | Pulmonary embolism | |
| Pericardium | Effusion | Tamponade | |
| Valves | Stenosis and regurgitation | Valvular | |
| Lungs (LUS) | 12 zone exam | Pleura A and B lines Parenchyma Effusion | Pneumonia, PTX ARDS Pneumonia Pulmonary edema |
| Vascular | IVC | Volume status | Hypovolemia Fluid overload |
| Veins | 2-point compression | DVT |
Table Legend: LV = left ventricle, RV = right ventricle, PTX = pneumothorax, ARDS = adult respiratory distress syndrome, IVC = inferior vena cava, DVT = deep venous thrombosis
Lung Ultrasound in COVID-19
CT of the chest in COVID-19 typically shows bilateral ground-glass opacities most commonly involving the posterior lobes. However, repeat CT exams are not feasible in all locations and situations due to the risk of transportation, radiation effects, cost, and risk of infection for health care professionals (HCP). Therefore, LUS offers a unique advantage over the CT. LUS is more portable and can be performed at the bedside with no radiation. LUS is also simple, rapid, low-cost, repeatable, and highly accurate. Findings on LUS have been shown to correlate with CT findings as long as the disease process extends to the pleural line.
Viral pneumonia caused by COVID-19 most commonly presents as a patchy concentration of B lines (representing increased alveolar fluid content), abnormalities in the pleural line, and the appearance of subpleural consolidations. Small pleural effusions can be seen, but large effusions are uncommon. A large pleural effusion should raise suspicion for bacterial infections or other pulmonary pathologies such as congestive heart failure or pulmonary edema. Nonetheless, either condition can co-exist with COVID-19.
The changes of LUS findings are helpful in the triage, risk stratification, classification of disease severity, monitoring of the disease progression, and potential confirmation of disease when RT-PCR testing is unavailable. Compared to a chest x-ray (CXR), LUS is more sensitive in detecting lung lesions located close to the pleura, and abnormalities appear earlier than on CXR. Although it is outside the scope of these recommendations, we note that LUS plays a beneficial role in the intensive care unit management of a COVID-19 patient. Specifically, it can help assess treatment responsiveness, aid ventilator management, monitor lung recruitment maneuvers, evaluate for endotracheal tube migration, and assess for a pneumothorax following procedures.
Performing Lung Ultrasound
A high-frequency, phased-array, or curvilinear probe can be used, preferably in the lung mode setting. Comprehensive scanning of all lung zones should be performed using the 12-zone technique, as pathology is often patchy and diffuse. This technique divides each hemithorax into anterior, lateral, and posterior zones, with each zone further subdivided into superior and inferior sections. Longitudinal scanning should be performed in all 12 zones systematically, emphasizing posterior and inferior lung zones for COVID-19. Transverse scanning is recommended in the areas of specific interest for further clear visualization of the pathology.
Dedicated ultrasound machines or portable ultrasound devices are preferred to decrease cross-infection rate, and proper donning, doffing of personal protective equipment (PPE) are essential when performing LUS in COVID-19. All extra materials should be removed from ultrasound machines and covered with disposable covers and separate gel packets. Cleaning of the equipment should be performed thoroughly per institution and machine guidelines. Limit the number of HCP involved with the LUS exam. The most experienced clinician should perform the LUS to minimize the time of exposure during scanning. It is recommended to standardize practice by saving and archiving the images and writing reports to be interpreted by experts and to monitor the disease progression.
The characteristic COVID-19 LUS findings are:
- B-Lines and interstitial syndrome (Figure 1A)
Early disease: focal B-lines
Severe Disease: diffuse confluent B-lines (light beam), multilobar distribution
- Pleural line abnormalities (Figure 1B)
Irregularities, unsmooth, thickening, and fragmentation
- Subpleural consolidations (Figure 1C)
Associated with B-lines
Presence of air bronchograms
- Small subpleural effusions (Figure 1D)
Video 1 - LUS: Multiple B lines with small effusion
Video 2 - LUS: Confluent B lines with thickened irregular pleural line
Video 3 - LUS: B lines with small peripheral infiltrate
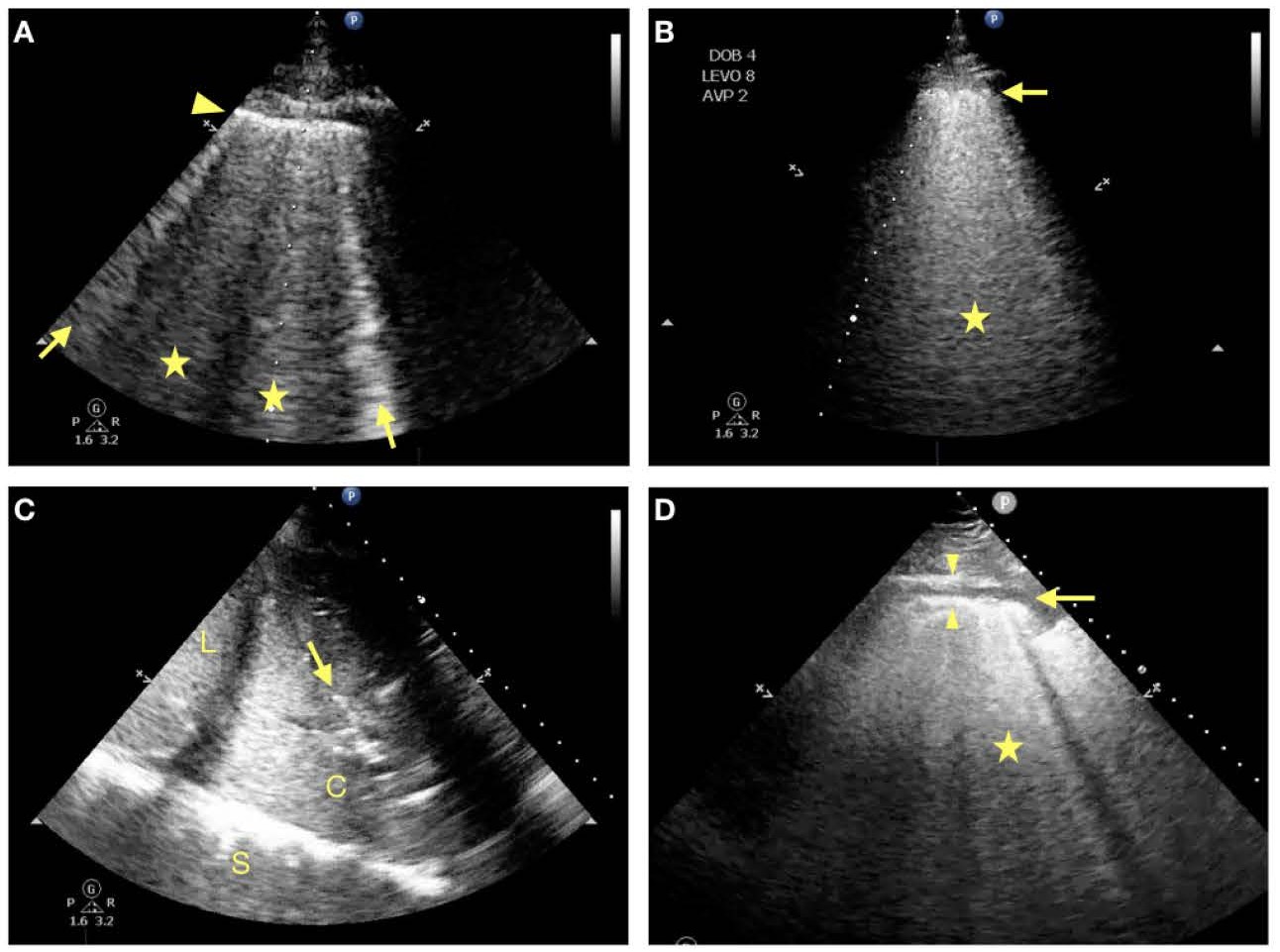
Figure 1. Lung ultrasound findings in COVID-19 patients
1A: This image shows ubiquitous single B-lines (arrows). In areas of worsening damage, the B-lines start to coalesce and form broader ring down artifacts (stars). The pleural line (arrow head) from which the B-lines originate appears continuous but already thickened compared to a normal lung. More than 3 B-lines per ultrasound window are considered abnormal. This is a typically found in the early stages of COVID-19.
1B: In an advanced stage of COVID-19 ARDS confluent B-lines (star) with a thickened and fragmented pleural line are common. This correlates to ground glass opacities found on CT scan.
1C: This image is taken from the lateral and basal thorax. It shows the liver (L) and a consolidated lung (C) with a white line inside the consolidation. This line represents an airbronchogram (arrow). If the line thickens and lengthens during inspiration, the airbronchogram is dynamic and is often found in a pneumonia or infectious process.
1D: COVID-19 lungs often present with small subpleural effusions (horizontal arrow) adjacent to infiltrated lung tissue, that appear as a dark (anechoic) layer separating the parietal (arrow head down) from the visceral pleura (arrow head up), which is the origin of multiple B-lines (star).
Limitations
LUS is operator-dependent and cannot detect disease further away from the pleural line. Similar to all POCUS exams, the findings should not be interpreted in isolation but should add to the individual patient's full clinical context.
Focused Cardiac Ultrasound (FoCUS) for COVID-19
POCUS for assessing patients with COVID-19 not only involves pulmonary assessment but should also include cardiac evaluation given that the virus has the potential to affect multiple organ systems. For example, COVID-19 can cause myocarditis presenting as myocardial dysfunction and pericardial effusion. Additionally, due to an increased incidence of hypoxemia and thrombotic events, right ventricular (RV) failure and massive pulmonary embolism can be seen. Of note, a significant decline in right heart function is a poor prognostic indicator in COVID-19. FoCUS can also be utilized to detect any pre-existing cardiac or valvular disease and to assess for significant changes in cardiac function.
Performing FoCUS
The cardiac phased array probe should be used to obtain the four basic views. These views include the parasternal long-axis view (PLAX), parasternal short-axis view (PSAX), apical 4-chamber view (A4C), subcostal 4-chamber view (SC4C), and subcostal inferior vena cava view (SC IVC). Ideally the FOCUS exam is started with the subcostal view (SC4C and SC IVC) as it can often provide sufficient information, especially since the other views (A4C, PLAX, and PSAX) are sometimes obscured given the hyperinflated lung (high positive end-expiratory pressure ventilation). See Table 2 for the clinical indication and associated pathology. (Videos 4-6).
Table 2. Cardiac and Inferior Vena Cava assessment with FoCUS in COVID-19
| FoCUS View | Clinical Indication | Pathology |
| PLAX (Figure 2C) | Myocardial function, valvular disease, pericardial effusion | Myocardial dysfunction, aortic stenosis, underfilling |
| PSAX (Figure 2D) | Myocardial function, pericardial effusion, hemodynamics | Myocardial dysfunction (RWMA), underfilling, massive PE, tamponade |
| A4C (Figure 2B) | Myocardial function, valvular disease, pericardial effusion | Cardiomyopathy, tamponade, myocardial dysfunction, PE, RVF |
| SC4C (Figure 2A) | Myocardial function, valvular disease, pericardial effusion | PE, tamponade |
| SC IVC | Volume status | Hypovolemia, fluid overload |
Table Legend: RWMA = Regional Wall Motion Abnormalities, PE = Pulmonary Embolism, RVF = Right Ventricular Failure
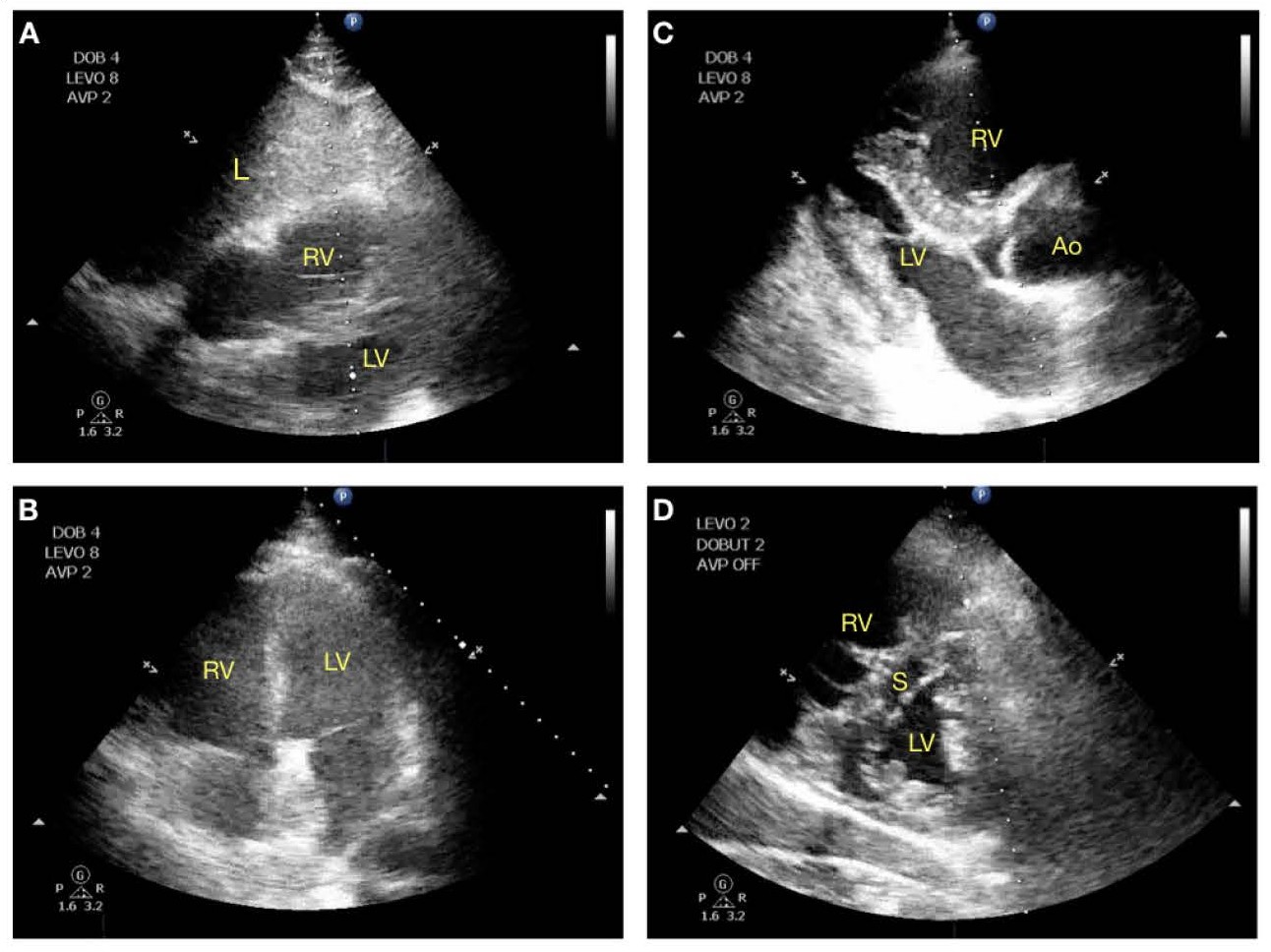
Figure 2: Cardiac ultrasound findings in COVID-19 patients
2A: Subcostal four-chamber view (SC4C) with the liver (L) topmost. The RV is most anterior and inferior in the mediastinum and is seen right underneath the liver and appears dilated. No pericardial effusion is seen.
2B: Apical 4 chamber view (A4C) with the RV to the left side of the screen. The RV appears to be dilated and larger than the LV.
2C: Parasternal long axis view (PLAX) with a markedly dilated RV outflow tract and a small LV cavity.
2D: Parasternal short axis view (PSAX). In RV failure from elevated afterload, the septum (S) starts to bulge into the LV cavity during end systole to early diastole, the so called “D-Sign” as the LV ventricle changes its shape from a donut to a “D”.
Video 4 - FoCUS: A4C view showing dilated right ventricle (RV)
Video 5 - FoCUS: PSAX view showing dilated RV and bulging of septum (`D` sign)
Video 6 - FoCUS: SC4C view showing dilated RV
As with LUS, all aseptic and PPE precautions should be taken while performing FoCUS. The most experienced clinician should perform the FoCUS exam to minimize the time of exposure during scanning. It is recommended to standardize practice by saving and archiving the images and writing reports to be interpreted by experts and to monitor the disease progression.
Limitations
FoCUS is operator-dependent and is more challenging to perform than LUS. Additionally, patient positioning (prone) or significant pulmonary pathology can make certain views challenging or impossible to obtain. As aforementioned, all findings should be interpreted in the context of the individual patient's full clinical presentation.
Vascular Ultrasound in COVID-19
Volume responsiveness assessment in a mechanically ventilated patient and right atrial pressure estimation in a spontaneously breathing patient can be performed in the subcostal inferior vena cava (IVC) view by measuring the IVC diameter and its respiratory variations with IVC diameter less than 1.5 cm and total collapse being considered as hypovolemic. If the transverse diameter of the IVC is equal to or more than 2 cm, it can be considered as fluid overload state. Note that IVC assessment can be primarily affected by right heart pathology and should always be assessed in correlation with the RV. Additionally, if there is acute RV dysfunction, this could be a manifestation of the hypercoagulable state seen in COVID-19 patients. Therefore, assessment for DVT in the lower extremities and other veins, especially in sedated, ventilated, and immobile patients, is indicated.
POCUS Training During COVID-19
POCUS training during the COVID-19 pandemic has enhanced the role of non-traditional means to provide both didactic and hands-on training opportunities due to the need for social distancing and limitations regarding PPE. Online didactic materials have become a fundamental means to provide education. Simulation has served as a means to practice scanning without unnecessarily exposing a healthy model or patient to respiratory pathogens.
Conclusions
POCUS can now be considered a modern century stethoscope that enables diagnosis and continuous care of COVID-19 patients, at times eliminating the need for extensive investigations like CXR, CT, and complete ECHO examinations. With the introduction of handheld/portable ultrasound devices, POCUS applications can be more widely used for perioperative, emergency, and intensive care management of COVID-19 patients.
Hari Kalagara, MD, is an assistant professor in the Anesthesiology Department at Mayo Clinic in Jacksonville, FL.
Oliver P.F. Panzer, MD, is an associate professor in the Anesthesiology Department at Columbia University College of Physicians and Surgeons in New York.
Stephen Haskins, MD, is an assistant professor in the Anesthesiology Department at the Hospital for Special Surgery in New York.
References
- Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. NEJM. 2020;382:1708–20. https://doi.org/10.1056/NEJMoa2002032.
- Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020;296:E32–40. https://doi.org/10.1148/radiol.2020200642.
- Johri AM, Galen B, Kirkpatrick JN, Lanspa M, Mulvagh S, Thamman R. ASE statement on point-of-care ultrasound (POCUS) during the 2019 novel coronavirus pandemic. J Am Soc Echocardiography. 2020;33:670–3. Available at: https://www.asecho.org/wp-content/uploads/2020/04/POCUS-COVID_FINAL2_web.pdf. Accessed August 24, 2020.
- Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-NCoV). Radiology. 2020;295:202–7. https://doi.org/10.1148/radiol.2020200230.
- Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein D, Mathis G, Kirkpatrick A, et al. International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:557–91. https://doi.org/10.1007/s00134-012-2513-4.
- Peng QY, Wang XT, Zhang LN. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020;46:849–50. https://doi.org/10.1007/s00134-020-05996-6.
- Volpicelli G, Lamorte A, Villén T. What’s new in lung ultrasound during the COVID-19 pandemic. Intensive Care Med. 2020;46:1445–8. https://doi.org/10.1007/s00134-020-06048-9.
- Smith MJ, Hayward SA, Innes SM, Miller ASC. Point-of-care lung ultrasound in patients with COVID-19 – a narrative review. Anaesthesia. 2020;75:1096–104. https://doi.org/10.1111/anae.15082.
- Canadian Point of Care Ultrasound Society. Disinfecting protocols for COVID-19. https://www.cpocus.ca/covid-19/disinfecting-protocols/. Published October 25, 2020. Accessed August 24, 2020.
- Lichtenstein DA. Current misconceptions in lung ultrasound: a short guide for experts. Chest. 2019;156:21–5. https://doi.org/10.1016/j.chest.2019.02.332
- Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–55. https://doi.org/10.1161/CIRCULATIONAHA.120.0469411
- Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5:751–3. https://doi.org/10.1001/jamacardio.2020.1105.
- Haskins SC, Tanaka CY, Boublik J, Wu CL, Sloth E. Focused cardiac ultrasound for the regional anesthesiologist and pain specialist. Reg Anesth Pain Med. 2017;42:632-44. https://doi.org/10.1097/AAP.0000000000000650.
- Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am College Cardiol. 2020;75:2950–73. https://doi.org/10.1016/j.jacc.2020.04.031.



Leave a commentOrder by
Newest on top Oldest on top