How I Do It: External Oblique Intercostal Plane Block
Cite as: White L, Kerr M, Bright M. How I do it: external obliqueintercostal plane block. ASRA Pain Medicine News 2023;48. https://doi.org/10.52211/asra050123.004.
Introduction
In recent years, fascial plane blocks have grown in popularity with surgeons, patients, and anesthesiologists due to their simplicity, analgesic efficacy, and favorable safety profile. The number of new fascial plane blocks continue to rise exponentially. One of the most promising is the external oblique intercostal (EOI) plane block. This novel superficial plane block was first described by Hamilton and colleagues in 2019.1,2 The proposed benefit of this block was to provide analgesia for upper abdominal surgery. Since its initial description, numerous case reports and small cohort studies have demonstrated successful use in laparoscopic and open upper abdominal surgeries, including pancreatoduodenectomy, gastrostomy, cholecystectomy, and bariatric surgery.3-7
Anatomy
The anterolateral upper abdominal wall receives innervation from the ventral rami of spinal nerves T6 - T10. As these nerves course from their neuraxial origin to the midline, they give off two key branches – the lateral cutaneous and anterior cutaneous branches of the intercostal nerves. These branches run within specific fascial planes allowing them to be targeted by previously well described techniques, such as the serratus anterior plane block and rectus sheath block, respectively. The EOI plane block aims to target both branches with a single injection.
The external oblique is a thin, broad muscle that spans both the lower thorax and abdomen (Figure 1A). It originates on the external surfaces of ribs 5-12 where it also forms digitations with the serratus anterior and latissimus dorsi muscles. As it courses anteriorly from the midclavicular line, it forms an extensive aponeurosis, which eventually becomes part of the anterior rectus sheath. Spinal nerves T6 – T9 emerge from the costal margin into the plane between the internal oblique and transversus abdominis (Figure 1B). They then enter the lateral border of the rectus sheath to eventually pierce the muscle and terminate as the anterior cutaneous branches.8
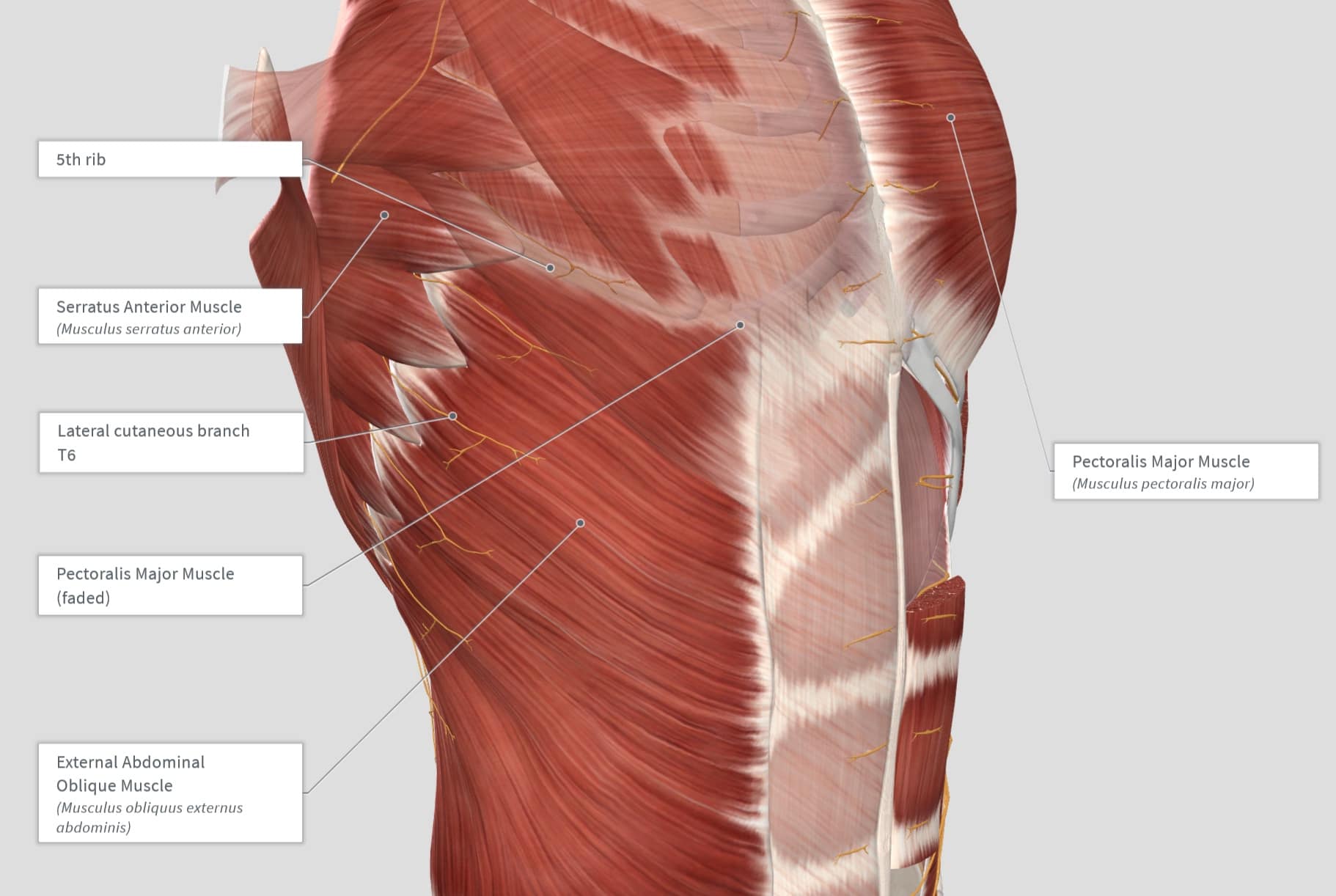
Figure 1A. Showing the relationship between the external oblique, pectoralis major, and the serratus anterior muscles.
Reproduced with permission from Complete Anatomy.
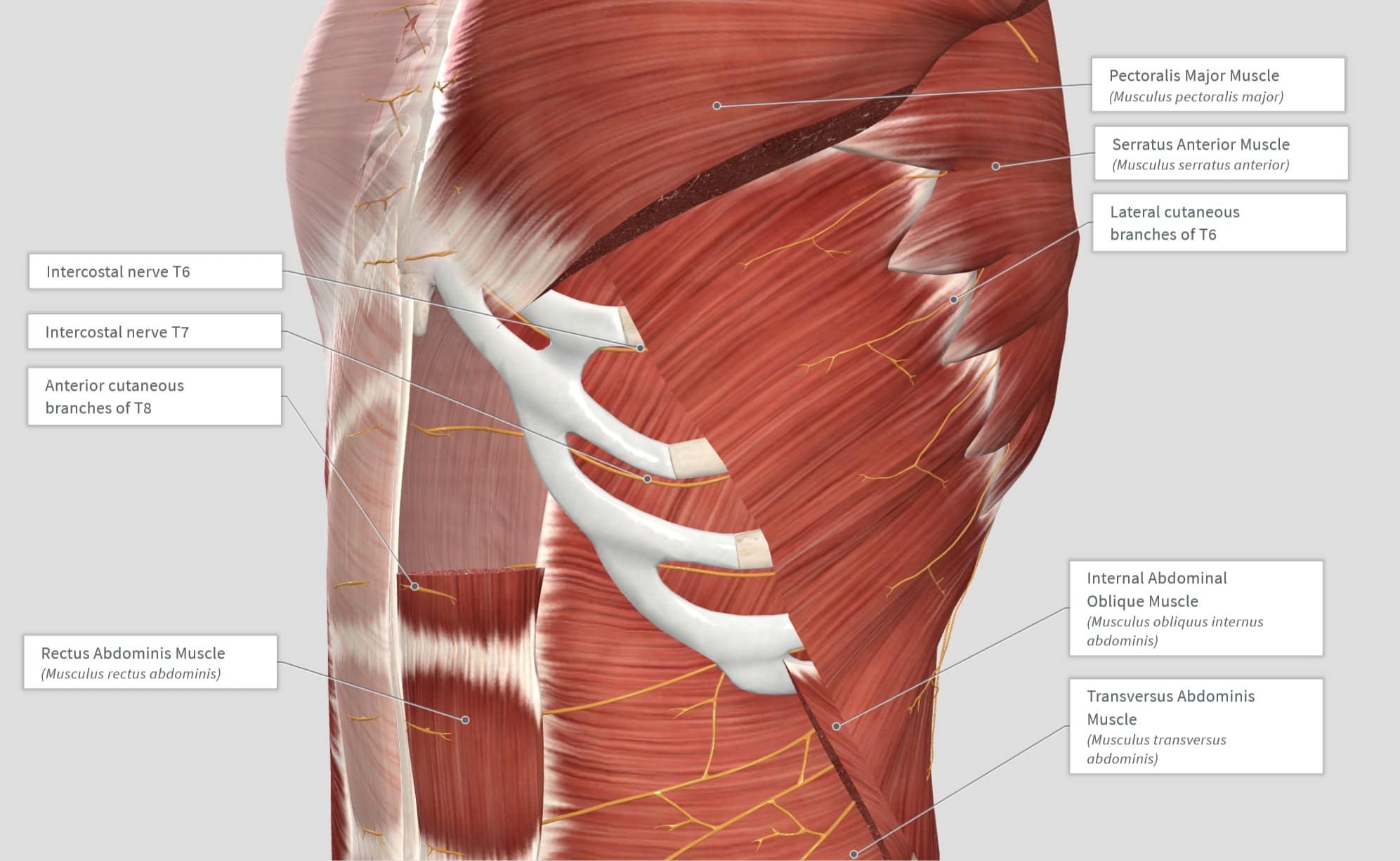
Figure 1B. Note the emergence of the lateral cutaneous branches at the interdigitation of the external oblique and serratus anterior muscle. Also note the course of the intercostal nerve as it passes inferior to the costal margin to then breach anteriorly through the rectus abdominis muscle to terminate as the anterior cutaneous branches.
Reproduced with permission from Complete Anatomy.
A common source of confusion when discussing the anatomy of the EOI plane block is how an injection below the external oblique muscle could spread posterior to the rectus abdominis muscle and thus anesthetize the anterior cutaneous branches. As the internal oblique aponeurosis also forms a layer of the anterior sheath, it may be thought that this would act as a diffusion barrier to direct local spread anteriorly. However, above the costal margin there is a deficiency in the posterior sheath, and the muscle epimysium lies directly on the costal cartilages with an intervening layer of fatty tissue, which provides a potential path for diffusion of local anaesthetic.9 We would draw the reader’s attention to the exceptional figure provided by Elsharkawy et al in their supplementary material that depicts the various fascial layers involved during the transition from lower thorax to upper abdomen.6
The improved spread of local anesthetics in the EOI block is also beneficial when compared to transversus abdominis plane (TAP) and rectus sheath (RS) blocks.
Elsharkawy et al recently demonstrated that an injection within the EOI plane resulted in spread of dye deep to the serratus anterior and pectoralis major muscles with respective staining of the lateral and anterior cutaneous branches.6 It should be noted that this is distinctly different from the recently described external oblique muscle plane block, which occurs superficial to the external oblique muscle at the costal margin and lateral abdomen.10 The external oblique muscle plane block appears only to contain the lateral intercostal branches. Unlike the external oblique muscle plane block, the target site for the EOI plane block is performed cephalad to the costal margin, deep to the external oblique muscle, and superficial to the intercostal muscle/rib.
Indications
The EOI plane block has several proposed advantages compared to existing plane blocks targeting the upper abdomen. The EOI plane block may provide improved pain scores and opioid requirements compared to the erector spinae plane block, which may be attributed to its coverage of nerves arising from the anterior and lateral branches of intercostal nerves.5 The improved spread of local anesthetics in the EOI block is also beneficial when compared to transversus abdominis plane (TAP) and rectus sheath (RS) blocks. TAP blocks fail to reliably block the lateral cutaneous branches of the intercostal nerves that cover the upper abdominal wall,12,13 while the utility of rectus sheath blocks is limited to midline incisions.11 As the EOI plane block is superficial, it can be safely performed in anticoagulated patients. Additionally, the EOI can be performed quickly in supine patients without the need to alter the patient’s position, which may not be possible in frail or unwell patients. Finally, the EOI block is performed well away from the surgical field with less potential for disruption to ultrasound images by carbon dioxide insufflation compared with TAP and RS blocks as well as its distance away from surgical dressings and drains. Each of these factors make it an ideal choice for patients undergoing surgery in the upper abdomen, regardless of body habitus. A summary of published and ongoing studies for the EOI block are summarized in Table 1.
Table 1: Available Evidence for the use of an external oblique intercostal plane block.
| Study Year | Number of Patients | Study Type | Setting | Marker of Successful Blockade | Clinical Effect |
| Coşarcan5 2022a | 15 EOI 39 no block 44 TAP + RS 15 ESPB | Retrospective Cohort | Bariatric surgery | Analgesic effect |
|
| Coşarcan14 2022b | 3 EOI | Case Series | Open liver surgery, laparoscopic liver surgery, and laparoscopic bariatric surgery | Analgesic effect |
|
| Elsharkawy5 2021 | 22 EOI | Case Series | Open or laparoscopic gastric, colorectal, liver, and renal surgery | Sensory blockade |
|
| Kuşderci15 2022 | 5 EOI | Case Series | Rescue analgesia for laparoscopic upper abdominal surgery | Sensory blockade and analgesic effect | Pain scores dropped below 3 within 30 minutes post block for all patients |
| Liotiri3 2022 | 4 EOI | Case Series | Step down analgesia post TEA for open pancreatic surgery | Analgesic effect | All patients remained opioid- free for the four-day duration of EOI catheter placement |
| Meneghetti4 2022 | 1 EOI | Case Study | Open gastrostomy | Analgesic effect |
|
| O’Donovan7 2022 | 1 EOI | Case Study | Open cholecystectomy | Analgesic effect |
|
| Ruggiero16 2022 | 1 EOI | Case Study | Abdominoplasty | Analgesic effect | No rescue analgesia required in 24 hours |
| Strumia16 2022 | 1 EOI | Case Study | Rescue analgesia for an open pancreatectomy | Sensory blockade and analgesic effect |
|
| White17 2022 | 2 EOI | Case Series | Laparoscopic cholecystectomy and rescue analgesia for an open distal pancreatectomy | Sensory blockade and analgesic effect |
|
| Registered Trials | Number of Patients | Study Type | Comparator | Setting | Outcome Measures |
| NCT05632991 | 80 | RCT | Subcostal TAP block | Laparoscopic cholecystectomy |
|
| NCT05444945 | 80 | RCT | Control | Laparoscopic cholecystectomy |
|
| NCT05614921 | 60 | RCT | Wound infiltration | Laparoscopic sleeve gastrectomy |
|
| NCT05536557 | 80 | RCT | Sham block | Laparoscopic cholecystectomy |
|
| NCT05592522 | 80 | RCT | OSTAP block | Bariatric surgery |
|
| NCT05272280 | 80 | RCT | ESP block | Laparoscopic cholecystectomy |
|
| NCT05502159 | 60 | RCT | M-TAPA block | Laparoscopic cholecystectomy |
|
| NCT05432557 | 60 | RCT | Subcostal TAP block | Supra-umbilical surgical incisions |
|
OME= oral morphine equivalent, ESP = erector spinae plane, RCT = randomized controlled trial, M-TAPA = modified thoracoabdominal plane block, OSTAP = oblique subcostal transversus abdominis plane block, TEA = thoracic epidural analgesia
Sonoanatomy, Positioning, and Technique
When performing this block, it is expected that the EOI plane will be found at less than 4cm deep in all patients regardless of body habitus.14 For this reason a high-frequency, linear probe can be used on all patients. The patient is positioned supine with the ipsilateral arm abducted. The suggested starting point for scanning is at the anterior axillary line at the level of the xiphoid process, which should place the probe at the sixth rib. Immediately superficial to the sixth rib is the junction between the serratus anterior muscle and the external oblique muscle (Figures 1A and 1B). The external oblique muscle can then be traced inferiorly to a subcostal view, and the probe rotated in a transverse orientation to find the traditional subcostal transversus abdominus muscle plane view. If this approach is hindered by dressings or anatomical disruption, another means to confirm the appropriate location is to translate the probe laterally to visualize the junction between the serratus anterior and external oblique. Following confirmation of the external oblique muscle, the EOI plane is then identified deep to the external oblique muscle and superficial to the internal intercostal muscle/rib (Figure 2A). Often the seventh rib is more superficial compared to the sixth rib. To create a downhill needle trajectory from cephalad to caudad, the caudad part of the probe can be rotated laterally.
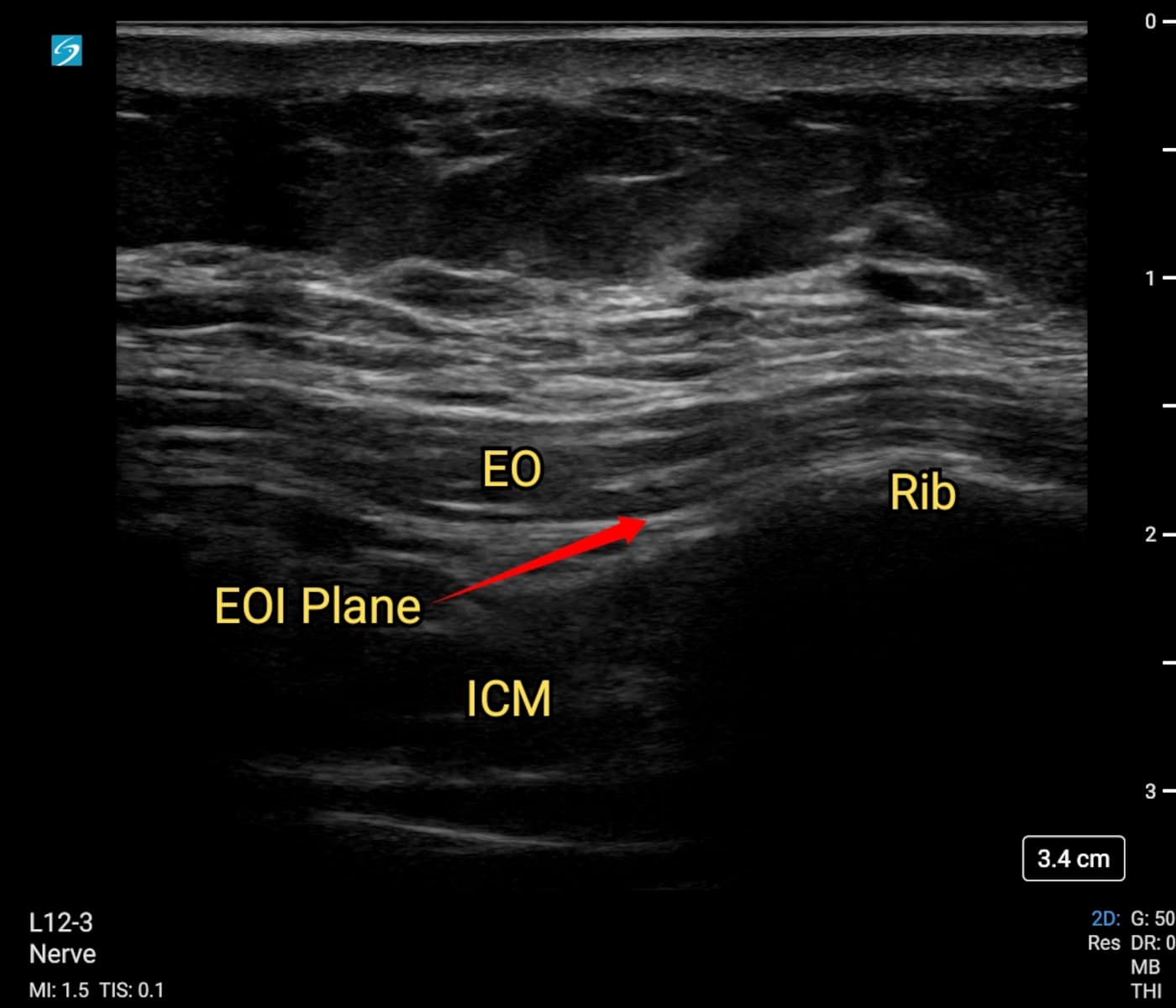
Figure 2A. Note the intended target is just caudal to the rib. If hydrodissection of the EOI plane proves difficult, this allows an intentional “overshoot” of the needle into the intercostal muscles. The needle is then withdrawn slowly with gentle pressure applied to the syringe. There is often a sudden opening of the space as the needle tip removes out of the muscle and into the appropriate plane.
EO = external oblique muscle, ICM = intercostal muscle
Needle Trajectory
Following local anesthetic infiltration subcutaneously, the needle is inserted from a cephalad to caudad direction. A shallow, less than 45-degree angle of needle approach is suggested to allow for hydro dissection of the plane under low injection pressures. Care is taken to hydro dissect and progress the needle tip within the EOI plane (Figure 2B). Intramuscular injection can be readily identified by localized swirling or pooling of injectate and a lack of planar spread beyond the seventh and eighth ribs (Figure 2C). A catheter can then be placed in this plane several centimeters beyond the needle tip.
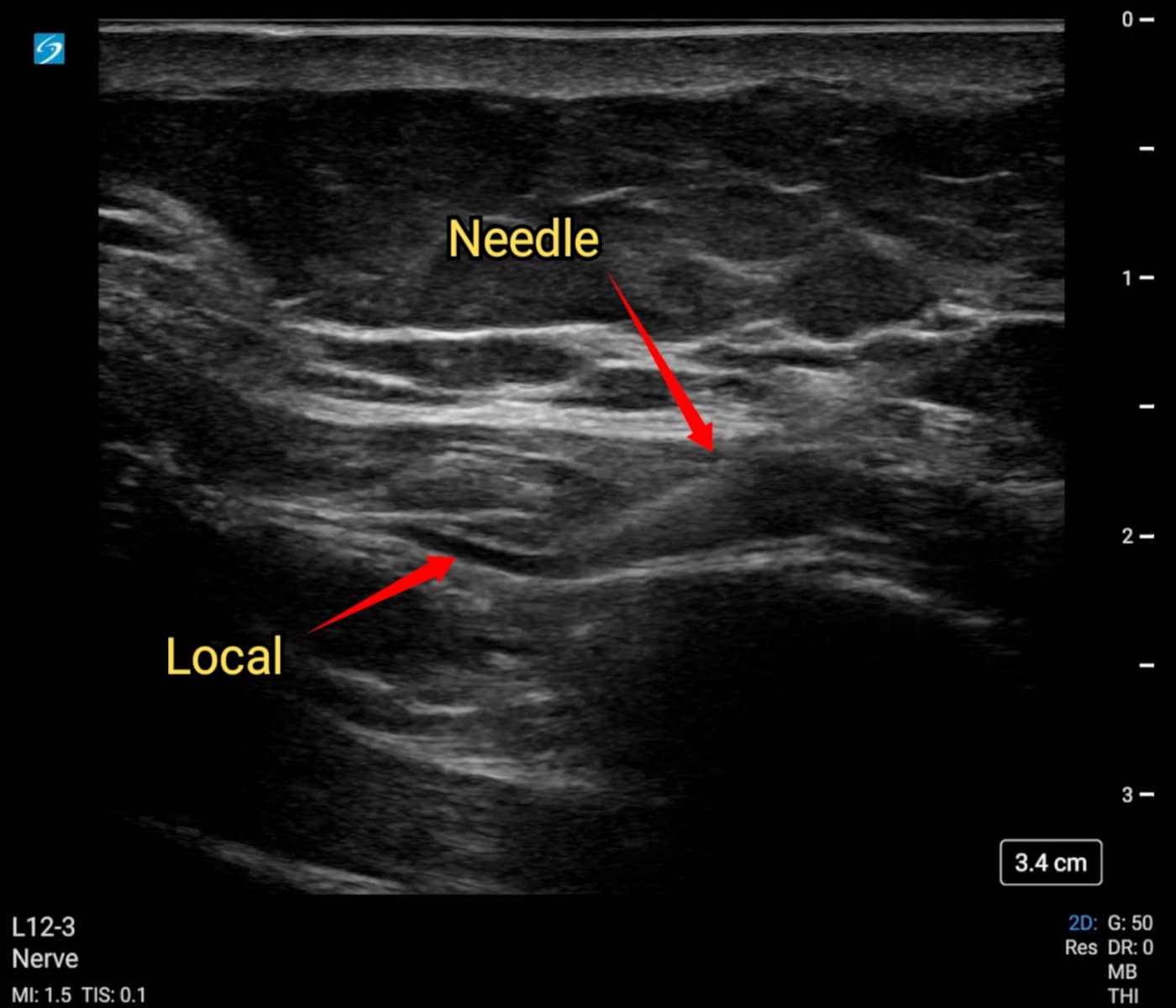
Figure 2B. The needle has entered just caudal to the sixth rib. Once the appropriate plane has been identified and opened, the needle can be repositioned to facilitate further hydrodissection and expansion of the external oblique intercostal (EOI) plane.
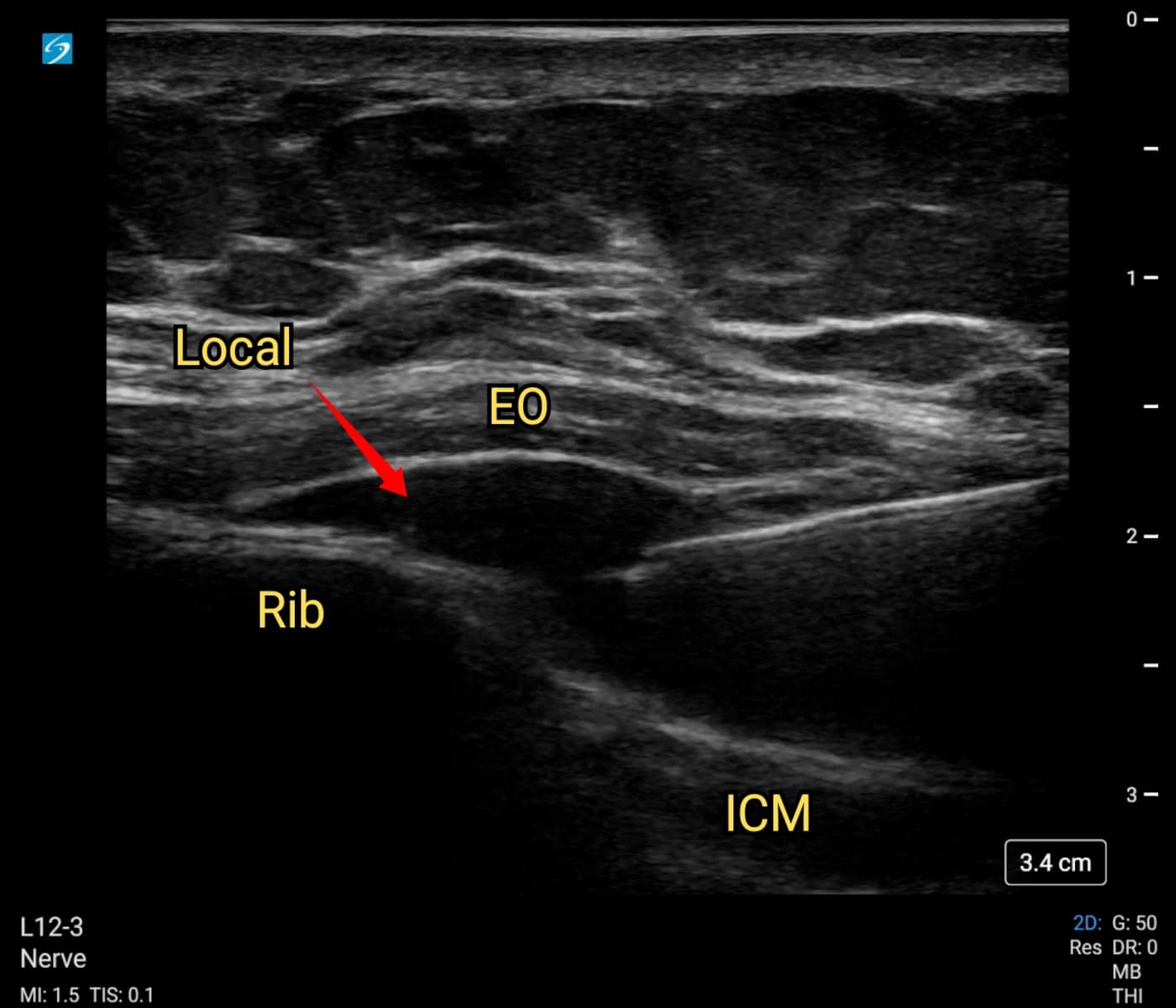
Figure 2C. Note the repositioning of the needle towards the seventh rib.
EO = external oblique muscle, ICM = intercostal muscle
Choice of Local Anesthetic
The EOI plane block is a fascial plane block that requires larger local anesthetic volumes. The initial cadaver studies used dye volumes of 22-30 mL.2,6 In our practice we recommend 15-30 mL of a long-acting local anesthetic as an initial bolus on each side. For infusion we use a 10 to 15 mL programmed intermittent bolus of 0.2% ropivacaine every two to three hours based on patient size and comorbidities.
Complications
Currently there is no safety data specific to the EOI plane block. However, the EOI plane block is part of the interfascial plane block family.
Clinical Pearls
- Once the EOI plane is identified, rotation of the caudad portion of the probe laterally will result in a downhill needle trajectory.
- Correct identification of the target plane is signaled by hydrodissection beyond the seventh and eighth ribs.
- When placing a catheter, after confirmation of negative aspiration, a small volume of air (0.5 to 2mL) can be injected for tip placement confirmation using ultrasound.
Conclusion
Our article has outlined the anatomy and techniques in performing the EOI plane block. Like other interfascial plane blocks, it has the advantages of being simple to perform, even on patients with coagulation issues. It is typically used for surgical incisions on the anterolateral abdominal wall spanning T6 to T10-11 dermatomes. There need to be high-quality studies other than case reports or cohort studies to properly evaluate the efficacy of this interfascial plane block.
Leigh White BSc(Hons), MBBS, Grad Dip (ClinUS), FANZCA, is a consultant anaesthetist in the Department of Anaesthesia and Perioperative Medicine at Sunshine Coast University and a senior lecturer in the Griffith University School of Medicine, both inBirtinya, QLD, Australia
Michael Kerr, BSc, MBBS, Grad CIR (ClinUS), FANZCA, is a consultant anaesthetist, in the Department of Anaesthesia and Acute Pain Management at QEII Jubilee Hospital in Coopers Plains, QLD, Australia.
Matthew Bright, BMedSc(Hons I), MD, is an anaesthetic registrar in the Department of Anaesthesia and Perioperative Medicine at Princess Alexandra Hospital in Woolloongabba, and an associate lecturer in the University of Queensland School of Medicine in St Lucia, both in QLD, Australia.
References
- Hamilton DL, Manickam BP. Is a thoracic fascial plane block the answer to upper abdominal wall analgesia? Reg Anesth Pain Med 2018;43:891-2. https://doi.org/10.1097/AAP.0000000000000838
- Hamilton DL, Manickam BP, Wilson MAJ, et al. External oblique fascial plane block. Reg Anesth Pain Med 2019:rapm-2018-100256. https://doi.org/10.1136/rapm-2018-100256
- Liotiri D, Diamantis A, Sioka E, et al. B28 the external oblique intercostal plane block as part of enhanced recovery after pancreatic surgery: a case series. Reg Anesth Pain Med 2022;47:A97-8. https://doi.org/10.1136/rapm-2022-ESRA.103
- Meneghetti F, De Padova D, Behr AU. B225 the answer to the dilemma of the upper abdominis wall analgesia? The application of multimodal anaesthesia in a frail patient: a case report. Reg Anesth Pain Med 2022;47:A191-2. https://doi.org/10.1136/rapm-2022-ESRA.299
- Cosarcan SK, Yavuz Y, Dogan AT, et al. Can postoperative pain be prevented in bariatric surgery? Efficacy and usability of fascial plane blocks: a retrospective clinical study. Obes Surg 2022;32:2921-9. https://doi.org/10.1007/s11695-022-06184-9
- Elsharkawy H, Kolli S, Soliman LM, et al. The external oblique intercostal block: anatomic evaluation and case series. Pain Med 2021;22:2436-42. https://doi.org/10.1093/pm/pnab296
- O’Donovan B, Martin B. The novel use of an external oblique nerve catheter after open cholecystectomy. Cureus 2021;13(2):e13580. https://doi.org/10.7759/cureus.13580
- Rozen WM, Tran TMN, Ashton MW, et al. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat 2008;21(4):325-33. https://doi.org/10.1002/ca.20621
- Karmakar MK, Soh E, Chee V, et al. Acknowledgments. In: Karmakar MK, Soh E, Chee V, et al. Atlas of Sonoanatomy for Regional Anesthesia and Pain Medicine. New York, NY: McGraw-Hill Education; 2018.
- Ohgoshi Y, Kawagoe I, Ando A, et al. Novel external oblique muscle plane block for blockade of the lateral abdominal wall: a pilot study on volunteers. Can J Anaesth 2022;69(10):1203-10. https://doi.org/10.1007/s12630-022-02310-4
- Onwochei DN, Borglum J, Pawa A. Abdominal wall blocks for intra-abdominal surgery. BJA Educ 2018;18(10):317-22. https://doi.org/10.1016/j.bjae.2018.07.002
- Borglum J, Jensen K, Christensen AF, et al. Distribution patterns, dermatomal anesthesia, and ropivacaine serum concentrations after bilateral dual transversus abdominis plane block. Reg Anesth Pain Med 2012;37(3):294-301. https://doi.org/10.1097/AAP.0b013e31824c20a9
- Barrington MJ, Ivanusic JJ, Rozen WM, et al. Spread of injectate after ultrasound-guided subcostal transversus abdominis plane block: a cadaveric study. Anaesthesia 2009;64(7):745-50. https://doi.org/10.1111/j.1365-2044.2009.05933.x
- Coşarcan S, Doğan A, Erçelen Ö, et al. B338 analgesic contribution of external oblique intercostal block: three different surgeries and three spectacular effect. Reg Anesth Pain Med 2022;47:A246. https://doi.org/10.1136/rapm-2022-ESRA.412
- Kuşderci H, Tulgar S, Genç C, et al. B337 external oblique fascial plane block may be a good option as a rescue analgesic method in laparoscopic upper abdominal surgeries. Reg Anesth Pain Med 2022;47:A245-6. https://doi.org/10.1136/rapm-2022-ESRA.411 J Anesth Analg Crit Care https://doi.org/10.1186/s44158-022-00070-7
- Ruggiero A, Strumia A, Costa F, et al. B346 more intrafascial, less intravenous: external oblique intercostal block for rescue analgesia after pancreatoduodenectomy. Reg Anesth Pain Med 2022;47:A250-1. https://doi.org/10.1136/rapm-2022-ESRA.420
- White L, Ji A. External oblique intercostal plane block for upper abdominal surgery: use in obese patients. Br J Anaesth 2022;128(5):e295-7. https://doi.org/10.1016/j.bja.2022.02.011


