Curb Your Enthusiasm: The RAPTIR Could Bite
What is RAPTIR?
A posterior or retroclavicular approach to an infraclavicular brachial plexus block was first described by Hebbard and Royse[1] in a letter to the editor in 2007. However, results from the first clinical study of the technique were not published until 2015 by Charbonneau and colleagues.[2] It has subsequently been popularized as the retroclavicular approach to the infraclavicular region (RAPTIR) block.[3]
Infraclavicular blocks are also associated with less tourniquet pain, more complete musculocutaneous nerve block than single injection axillary block, and decreased time to perform when compared to multiple injection axillary block.
The technique is performed with the patient supine and the arm adducted. A high-frequency linear ultrasound transducer is placed inferiorly to the clavicle just medially to the coracoid process in the parasagittal plane such that the axillary vessels and cords of the brachial plexus are viewed in cross-section (Figure 1).[1],[2] In this short axis view, the lateral cord appears in the anterocranial position, posterior cord in the posterocranial position, and median cord in the posterocaudal position (dependent on probe orientation and anatomic variation).[4] A needle insertion point is chosen in the supraclavicular fossa, between the clavicle and trapezius, so that the needle will pass behind the clavicle and enter the ultrasound image nearly parallel to the transducer (or perpendicular to the beam) (Figure 2).[1],[2] A long (80-100mm) needle is required given the distance from the supraclavicular fossa to the axillary artery. Because of the generally superior needle visualization achieved via a small angle of incidence of the needle relative to the ultrasound probe, an echogenic needle is generally not necessary.[5] A volume of 25-40ml of local anesthetic is then injected to achieve perivascular spread.[2],[6]
Why is RAPTIR Becoming More Popular?
A recent systematic review including 25 randomized trials and 1,948 patients found no differences in success rate between supraclavicular, infraclavicular, or axillary brachial plexus blocks.[7] Infraclavicular block advantages include the ability to place a secure catheter and a decreased incidence of diaphragmatic paresis when compared to supraclavicular blocks.[2],[8],[9] Infraclavicular blocks are also associated with less tourniquet pain, more complete musculocutaneous nerve block than single injection axillary block, and decreased time to perform when compared to multiple injection axillary block.[10] However, needle visualization is often poor because of the steep angle of insertion with the conventional approach (Figures 3 and 4).[11] The median angle of insertion is 50 degrees (ranging from 33–60) and is made worse in obese patients, with the angle of insertion correlating with body mass index.[11] The RAPTIR block was developed to overcome this needle visualization challenge.[1]
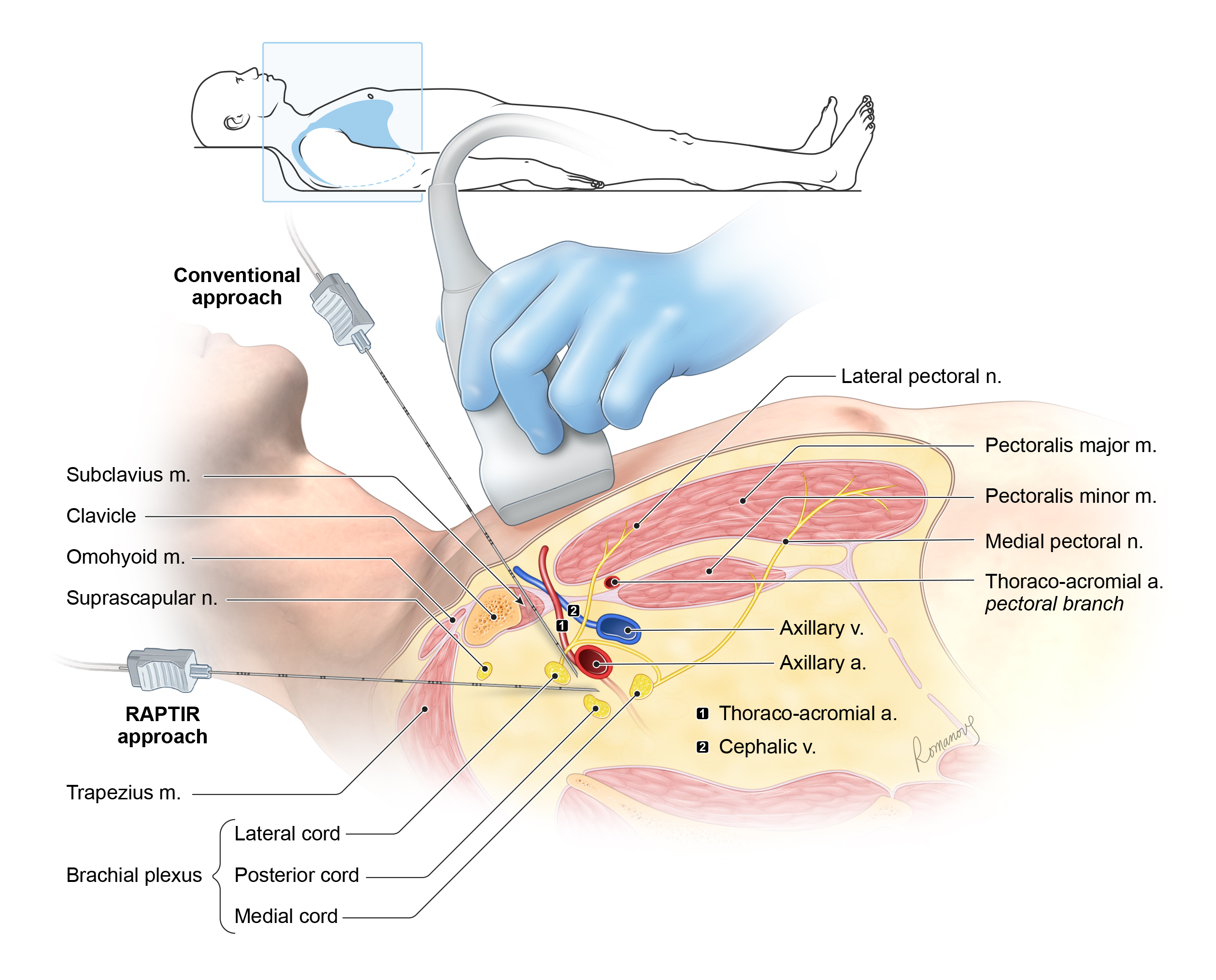
Figure 1: Needle insertion for conventional and retroclavicular approaches and related anatomic structures.
A randomized trial comparing the conventional (coracoid) infraclavicular block to the RAPTIR block confirmed that needle shaft and tip visualization were significantly better with the RAPTIR technique, with similar success rates and patient satisfaction.[6] It also found that block performance time and paresthesias encountered during block placement were reduced when using the RAPTIR approach.[6] This may be because the lateral cord is commonly located in the needle path of a conventional infraclavicular block.[12]
The horizontal needle path of the RAPTIR block prevents that problem and avoids both the pectoral branch of the thoracoacromial artery and the cephalic vein (Figure 4).[12] The position of the needle relative to the clavicle is also advantageous for patients with limited range of shoulder motion or those with a painful upper extremity injury.[12],[13] Whereas arm abduction improves needle angle and visualization in the conventional infraclavicular block, arm adduction improved needle insertion in the RAPTIR block.[5],[14] For this reason, RAPTIR has been advocated as a pain control option for patients in the emergency department with upper extremity injury.[13]
RAPTIR compares favorably to the supraclavicular approach, and a recent randomized controlled trial demonstrated similar success rates, pain control, and patient satisfaction.[15] Performance time for the RAPTIR was statistically longer. However, the absolute difference for performance time was less than 2 minutes and was therefore considered to not be clinically relevant.[15]
|
|
How Does the RAPTIR Bite?
Despite those advantages, the RAPTIR block is not without potential drawbacks. The major concern with the retroclavicular path is that the needle passes through an acoustic shadow behind the clavicle. Previously published cadaveric studies have demonstrated that the suprascapular nerve and suprascapular vein are vulnerable to injury because they are located along the needle trajectory of a RAPTIR block and in the clavicle’s acoustic shadow.[16] Neuromuscular stimulation during needle advancement through the acoustic window and monitoring for external rotation of the shoulder (supraspinatus and infraspinatus muscle stimulation) may reduce the incidence of inadvertent nerve injury.[16]
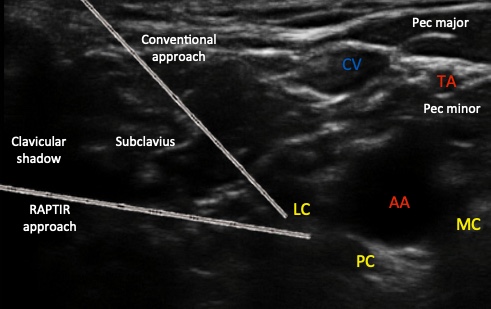 Figure 4: Ultrasound
image showing needle insertion for conventional and retroclavicular approaches and related anatomical structures. AA = axillary artery, CV = cephalic vein, LC = lateral cord, MC = medial cord, PC = posterior cord, TA = thoracoacromial artery
Figure 4: Ultrasound
image showing needle insertion for conventional and retroclavicular approaches and related anatomical structures. AA = axillary artery, CV = cephalic vein, LC = lateral cord, MC = medial cord, PC = posterior cord, TA = thoracoacromial artery
Infraclavicular brachial plexus blocks (whether conventional or retroclavicular) are classified as high risk for bleeding because of their noncompressible position under the clavicle and are not recommended for anticoagulated patients.[17] Additionally, because of the acoustic shadow casting a blind spot, pain physicians may advance the needle further than expected before locating it with the ultrasound transducer. That past pointing could result in nerve or vascular puncture or even pneumothorax. We recommend that the distance from the intended needle insertion point to the edge of the ultrasound transducer be measured externally once the optimal image has been obtained. Mark the needle shaft at that distance from the tip by grasping the shaft between index and thumb (Figure 5). Advance the needle past that point only once the tip is visualized in the ultrasound image.[5] Given that the needle path is horizontal and directed posteriorly to the axillary artery, spread to the lateral cords manifesting as a long onset time or may be reduced in the distribution of musculocutaneous nerve with RAPTIR, compared to conventional infraclavicular approach.[6]
 Figure 5: Measurement
of clavicle thickness before needle insertion for RAPTIR (retroclavicular approach to the infraclavicular region)
Figure 5: Measurement
of clavicle thickness before needle insertion for RAPTIR (retroclavicular approach to the infraclavicular region)
One cadaver dissection showed less dye surrounding the medial and lateral cords than the posterior cord when using a retroclavicular approach.[18] However, as mentioned previously, a randomized trial found similar rates of sensory and motor block success, surgical success, supplementation, and analgesic use.[6] To maximize perivascular spread during a retroclavicular approach, we suggest using our 5-6-7 technique.[5] Advance the needle past the 6-o’clock point to the axillary artery as viewed in the ultrasound image. At 5-o’clock (posterocaudal) position, deposit 25% of the local anesthetic. Withdraw the needle and deposit 50% of the local anesthetic at the 6-o’clock position and 25% at the 7-o’clock position (Figure 6).
Another potential problem is obtaining an optimal ultrasound image in a position that allows for the needle to pass easily behind the clavicle. The contour of the clavicle is highly variable, increasing the difficulty of a retroclavicular approach in a subset of patients with an acutely angulated clavicle, although the overall block performance time is not significantly different.[6],[19],[20] We suggest placing the patient’s arm in an adducted position with slight downward traction to improve clavicle orientation.[5]
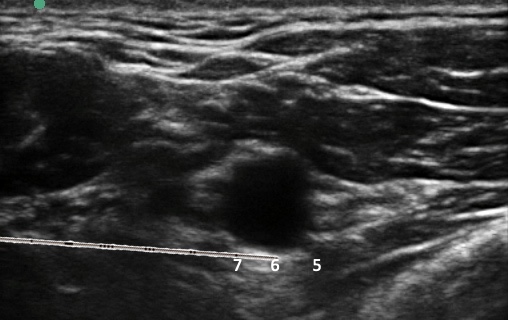 Figure 6: Ultrasound
image showing 5-6-7 technique (positions) to maximize perivascular spread during RAPTIR (retroclavicular approach to the infraclavicular region)
Figure 6: Ultrasound
image showing 5-6-7 technique (positions) to maximize perivascular spread during RAPTIR (retroclavicular approach to the infraclavicular region)
Finally, cadaveric studies have demonstrated the potential for a posterior cord injury with RAPTIR. Although the posterior cord is visible posteriorly to the axillary artery, in three of six cadaver dissections the posterior cord or its components were punctured by the needle.[16] We suggest hydrodissection of the posterior cord away from the axillary artery to allow needle passage. We also suggest using a neuromuscular stimulator and a low-pressure injection technique to minimize the chance of intraneural injection.[21],[22]
Conclusion
Over the past few years, the RAPTIR block has seen rapidly growing enthusiasm. Although the approach offers some advantages to the conventional infraclavicular technique, it also carries some unique risks. We recommend that this relatively new technique should be used selectively rather than as a wholesale adoption above other methods of infraclavicular and other approaches to brachial plexus blockade, with the benefits and risks of the technique being considered in the context of patient habitus and comorbidities.
Specifically, the RAPTIR approach is well suited for patients where the needle insertion angle is expected to be steep because of a thick chest wall, limited range of shoulder motion, or securing an indwelling catheter.[23] The approach is less well suited for those with highly angulated clavicles, full supraclavicular fossae, and thin chest walls. Further research is needed, and we look forward to the results of a multicenter, randomized, noninferiority trial comparing conventional (coracoid) infraclavicular blocks to the RAPTIR method.[24]
Acknowledgement
We would like to thank the Department of Anesthesia, Perioperative Medicine, and Pain Management at Dalhousie University, Nova Scotia Health Authority, in Halifax, Nova Scotia, Canada, for its support by providing us a $500 grant for the medical illustrations in this article.
References
- Hebbard P, Royse C. Ultrasound guided posterior approach to the infraclavicular brachial plexus. Anaesthesia 2007;62:539. Available at: https://doi.org/10.1111/j.1365-2044.2007.05066.x.
- Charbonneau J, Frechette Y, Sansoucy Y, Echave P. The ultrasound-guided retroclavicular block: a prospective feasibility study. Reg Anesth Pain Med 2015;40:605–609.
- Smit J, Tang R, Vaghadia H, Sawka A. The ultrasound-guided retroclavicular block comparison with a novel subpectoral approach. Reg Anesth Pain Med 2016;41:290. Available at: https://doi.org/10.1097/AAP.0000000000000335.
- Sauter AR, Smith HJ, Stubhaug A, Dodgson MS, Klaastad Ø. Use of magnetic resonance imaging to define the anatomical location closest to all three cords of the infraclavicular brachial plexus. Anesth Analg 2006;103:1571–1573.
- Uppal V, Kalagara HKP, Sondekoppam RV. Tips and tricks to improve the safety of the retroclavicular brachial plexus block. Am J Emerg Med 2018;36:1107–1108.
- Kavrut Ozturk N, Kavakli AS. Comparison of the coracoid and retroclavicular approaches for ultrasound-guided infraclavicular brachial plexus block. J Anesth 2017;31:572–578.
- Albrecht E, Mermoud J, Fournier N, Kern C, Kirkham KR. A systematic review of ultrasound-guided methods for brachial plexus blockade. Anaesthesia 2016;71:213–227.
- Koscielniak-Nielsen ZJ, Frederiksen BS, Rasmussen H, Hesselbjerg L. A comparison of ultrasound-guided supraclavicular and infraclavicular blocks for upper extremity surgery. Acta Anaesthesiol Scand 2009;53:620–626.
- Petrar SD, Seltenrich ME, Head SJ, Schwarz SKW. Hemidiaphragmatic paralysis following ultrasound-guided supraclavicular versus infraclavicular brachial plexus blockade: a randomized clinical trial. Reg Anesth Pain Med 2015;40:133–138.
- Chin K, Alakkad H, Adhikary S, Singh M. Infraclavicular brachial plexus block for regional anaesthesia of the lower arm. Cochrane Database Syst Rev 2013;8. Available at: https://doi.org/10.1002/14651858.CD005487.pub3.
- Kalagara HKP, Uppal V, McKinlay S, MacFarlane AJR, Anderson K. Effect of body mass index on angle of needle insertion during ultrasound-guided lateral sagittal infraclavicular brachial plexus block. J Clin Anesth 2015;27:375–379. https://doi.org/10.1016/j.jclinane.2015.03.039
- Sutton EM, Bullock WM, Gadsden J. The retroclavicular brachial plexus block additional advantages. Reg Anesth Pain Med 2015;40:733–734.
- Luftig J, Mantuani D, Herring AA, Nagdev A. Ultrasound-guided retroclavicular approach infraclavicular brachial plexus block for upper extremity emergency procedures. Am J Emerg Med 2017;35:773–777.
- Auyong DB, Gonzales J, Benonis JG. The Houdini clavicle: arm abduction and needle insertion site adjustment improves needle visibility for the infraclavicular nerve block. Reg Anesth Pain Med 2010;35:403–404.
- Grape S, Pawa A, Weber E, Albrecht E. Retroclavicular vs supraclavicular brachial plexus block for distal upper limb surgery: a randomised, controlled, single-blinded trial. Br J Anaesth 2019;122:518–524.
- Sancheti SF, Uppal V, Sandeski R, Kwofie MK, Szerb JJ. A cadaver study investigating structures encountered by the needle during a retroclavicular approach to infraclavicular brachial plexus block. Reg Anesth Pain Med 2018;43:752–755.
- Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy. Reg Anesth Pain Med 2018;43:263–309.
- Beh ZY, Hasan MS, Lai HY, Kassim NM, Md Zin SR, Chin KF. Posterior parasagittal in-plane ultrasound-guided infraclavicular brachial plexus block—a case series. BMC Anesthesiol 2015;15:1–7.
- Beh ZY, Hasan MS, Lai HY. Ultrasound-guided retroclavicular block (aka posterior approach infraclavicular block): anatomical variation of the clavicle limits block feasibility. Reg Anesth Pain Med 2016;41:658–659.
- Huang JI, Toogood P, Chen MR, Wilber JH, Cooperman DR. Clavicular anatomy and the applicability of precontoured plates. J Bone Jt Surg 2007;89:2260–2265.
- Klein SM, Melton MS, Grill WM, Nielsen KC. Peripheral nerve stimulation in regional anesthesia. Reg Anesth Pain Med 2012;37:383–392.
- Tsui BCH, Li LXY, Pillay JJ. Compressed air injection technique to standardize block injection pressures. Can J Anesth 2006;53:1098–1102.
- Uppal V, Sancheti SF, Kwofie MK, Szerb JJ. Novel approaches to the brachial plexus in the infraclavicular space: filling up the tool box. Reg Anesth Pain Med 2019. Available at: https://doi.org/10.1136/rapm-2018-100238.
- Langlois PL, Gil-Blanco AF, Jessop D, et al. Retroclavicular approach vs infraclavicular approach for plexic bloc anesthesia of the upper limb: study protocol randomized controlled trial. Trials 2017;18:1–9.
 Figure
2: Needle insertion for RAPTIR (retroclavicular approach to the infraclavicular region)
Figure
2: Needle insertion for RAPTIR (retroclavicular approach to the infraclavicular region) Figure 3: Needle insertion for conventional ultrasound-guided infraclavicular brachial plexus block (coracoid approach)
Figure 3: Needle insertion for conventional ultrasound-guided infraclavicular brachial plexus block (coracoid approach)
Leave a commentOrder by
Newest on top Oldest on top