How I Do It: Ultrasound-Guided Ankle Block
Cite as: Sehmbi H., Shah UJ., Uppal V. How I do it: ultrasound-guided ankle block. ASRA News. 2021;46. https://doi.org/10.52211/asra050121.028.
Introduction
Commonly performed for foot surgery,1 the ankle block offers several advantages including preservation of proximal motor function allowing the ability to ambulate compared to a proximal sciatic block and a low risk of serious complications compared to a spinal or a sciatic block.2,3 The administration of an ankle block often represents a simpler and safer alternative to general anesthesia in high-risk patients or when the provision of a spinal anesthetic is challenging (eg, previous back surgery) or contraindicated (eg, coagulopathy).4 As opposed to the landmark-based technique, ultrasound guidance overcomes inter-individual anatomical variation of nerves5 or obscured landmarks (eg, swollen inflamed ankle), improves block success,6,7 expedites block onset times, and reduces the amount of local anesthetic required. In this article, we review the practical aspects associated with the provision of ultrasound-guided ankle blocks and advantages related with this technique.
Preparation
In our clinical practice, we perform ultrasound-guided ankle blockade using a small footprint, high-frequency linear transducer (6-13 MHz) in a transverse plane, providing a cross-sectional view for all nerves. Essential equipment includes sterile probe cover with ultrasound gel, a hypodermic (25G) or a short bevel 22G block needle, sterile gloves, an assistant for positioning, local anesthetic injection, and sedation. After applying appropriate monitoring, supplemental oxygen, and an established IV access, sedation generally consists of 2 mg of midazolam and/or 50-100 mcg of fentanyl. Administration is titrated to ensure patient comfort throughout the procedure. Aseptic technique is observed, and the ergonomics are considered such that the operator can comfortably visualize the ultrasound screen by looking straight ahead (ie, the operator stands at the foot end, and the ultrasound machine is positioned in direct line of vision on ipsilateral or contralateral side). Skin infiltration is provided via the administration of 1% lidocaine when using a short-bevel needle for the block but is not required when using a hypodermic needle.
Pertinent Anatomy
The foot is innervated by 4 branches of the sciatic nerve, including the superficial peroneal, the deep peroneal, the tibial, and the sural nerves and the terminal branch of the femoral nerve (i.e., saphenous nerve) (Figure 1). The deep peroneal and the tibial nerves are deep, while the rest are superficial nerves (Figure 2).8 The origin, course, and relationship to various nerve structures are depicted in Figure 3.
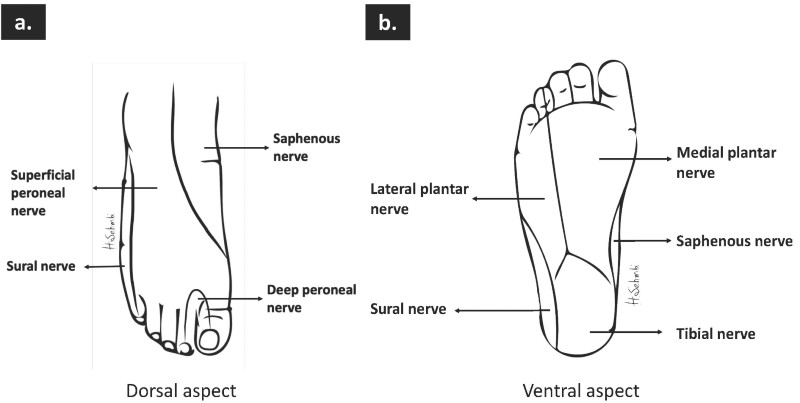
Figure 1. Cutaneous innervation of the foot (a) plantar surface (b) dorsal surface.
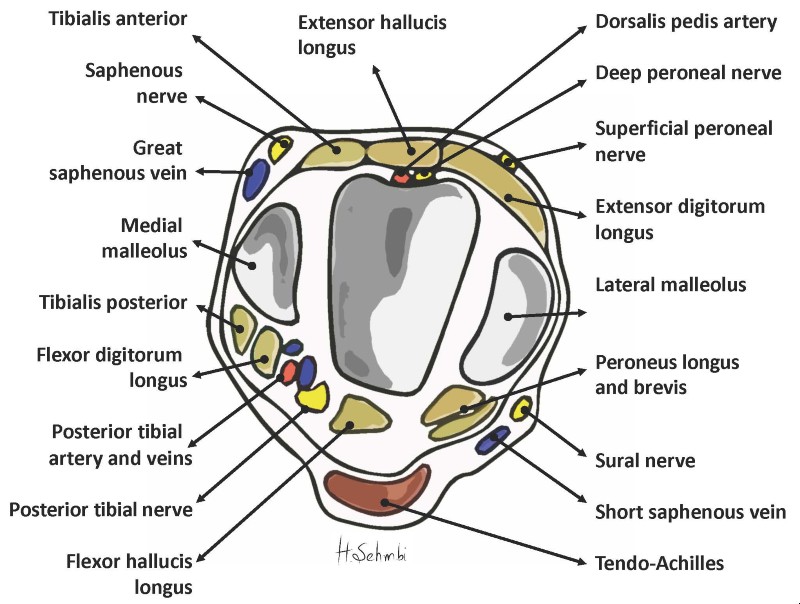
Figure 2. The relationship of the tibial nerve to the tendons at the level of the medial malleolus.
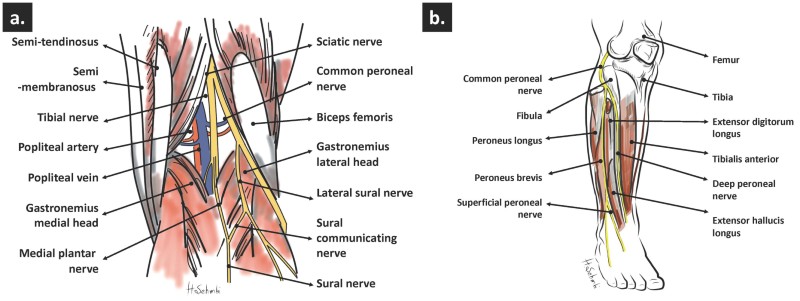
Figure 3. Origin and course of (a) tibial and sural nerve and (b) superficial and deep peroneal nerve.
Procedure
The following paragraphs provide details of the performance of the 5 nerves required for a complete ankle block. Clinical pearls are summarized at the end of article.
Tibial nerve (L4, L5, S1-3)
The patient is semi-recumbent or supine, and the ipsilateral hip is externally rotated, as shown (Figure 4a). A linear transducer is placed transversely, obtaining a scan of the tibial nerve (hyperechoic oval) proximal to medial malleolus, showing the tendons of the tibialis anterior and flexor digitorum profundus anterior to the nerve and gastrocnemius-soleus posterior to it (Figure 4b). The posterior tibial artery and the tendon of flexor hallucis longus lie deep to the nerve, often with two small veins on either side of the artery. The needle is introduced in-plane (or out-of-plane), proximal to the medial malleolus to approach near the tibial nerve (Figure 4c). Entry into the fascial sheath containing the nerve and subsequent local anesthetic injection (5-10 ml 0.5% ropivacaine) produces a characteristic circumferential spread around the tibial nerve (Figure 4d).
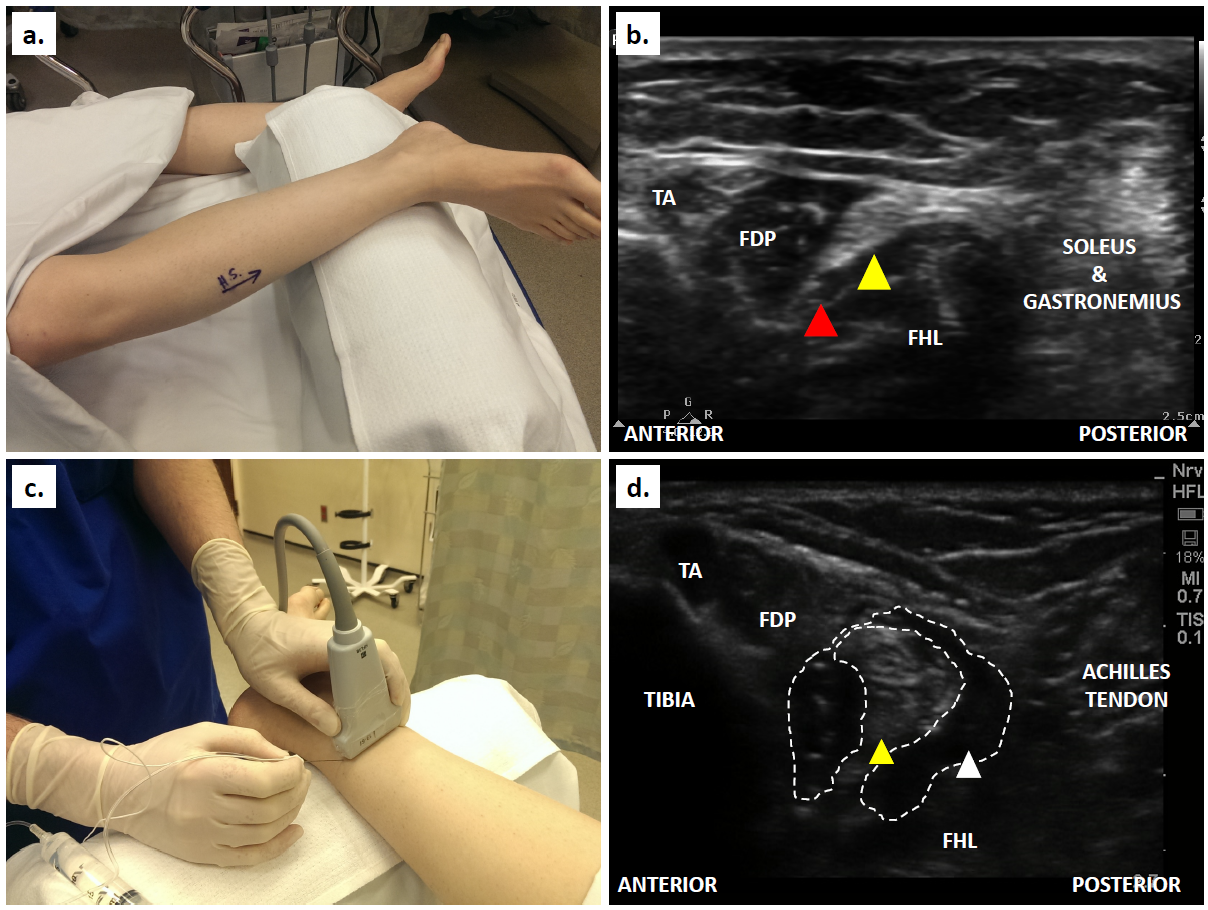
Figure 4. (a) Patient position for tibial nerve scanning at the medial malleolus; (b) Ultrasound scan of the structures slightly proximal to the medial malleolus; (c) Transverse placement of transducer and in-plane needling proximal to medial malleolus; (d) Ultrasound appearance of the tibial nerve post-injection. (TA - tibialis anterior, FDP - flexor digitorum profundus, FHL - flexor hallucis longus. Yellow arrowhead denotes tibial nerve; red arrowhead denotes posterior tibial artery; white arrowhead denotes local anesthetic spread around the nerve.)
Deep peroneal nerve (deep fibular nerve) (L4, L5, S1)
The leg is extended and placed on a bolster in a neutral position (Figure 5a). A linear transducer is placed transversely just above the intermalleolar line to identify the anterior tibial artery, which is seen as a pulsatile anechoic structure on the surface of the tibia (hyperechoic white curve) [Figure 5b]. The deep peroneal nerve is identified as a hyperechoic structure medial to the artery (Figure 5c). The needle is introduced in-plane from medial to lateral (or out-of-plane) to approach adjacent to the nerve (Figure 5d). Local anesthetic (2-4 ml 0.5% ropivacaine) is injected around the nerve.
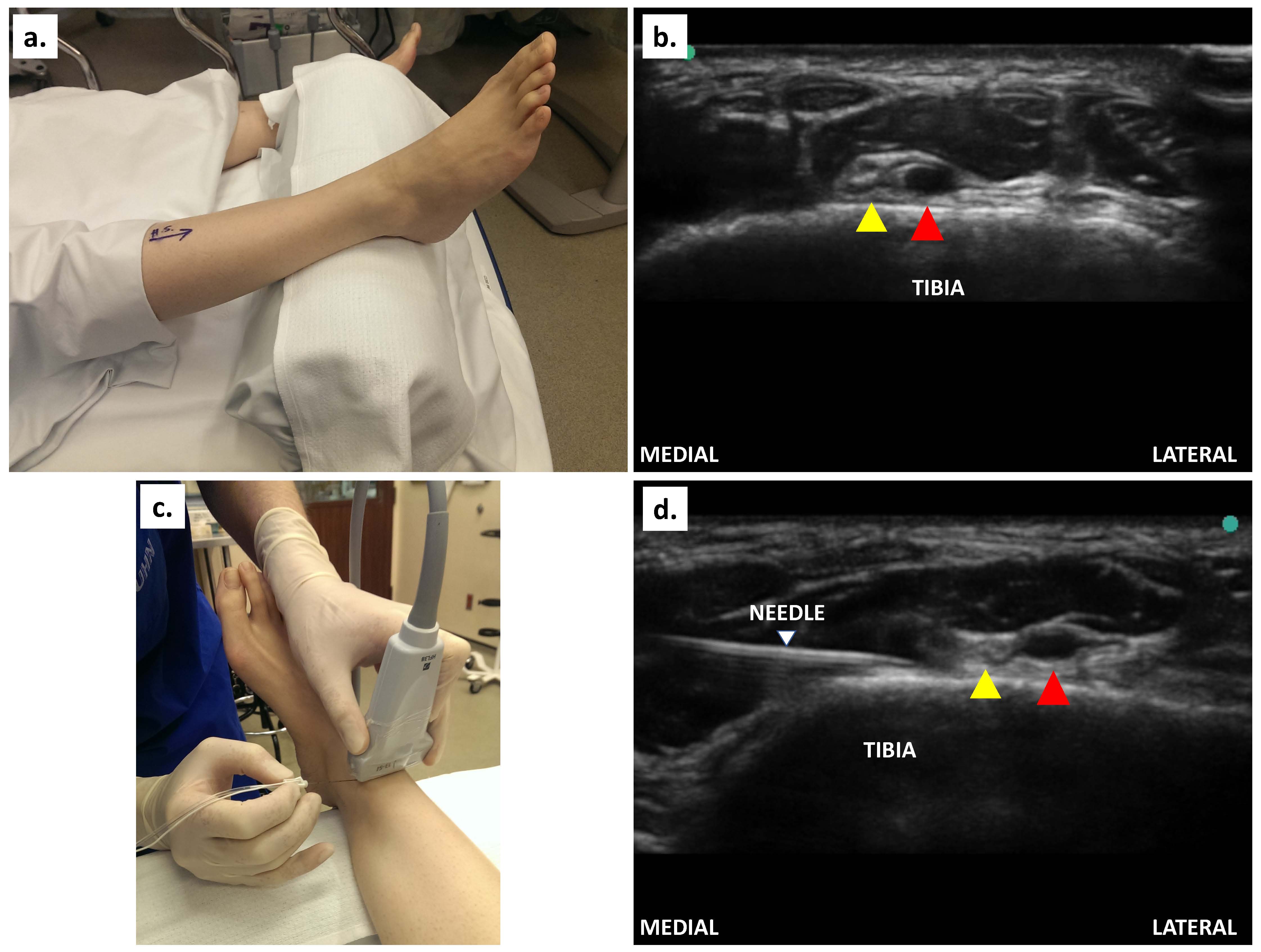
Figure 5. (a) Patient position for deep peroneal nerve block; (b) Ultrasound scan of the structures slightly proximal to the intermalleolar line; (c) Transverse placement of transducer and in-plane needling proximal to the intermalleolar line; (d) In-plane injection to block the nerve. (Yellow arrowhead denotes deep peroneal nerve; red arrowhead denotes anterior tibial artery; white arrowhead denotes the needle.)
Optional advanced (small nerves) ultrasound-guided blocks
The next section describes the ultrasound-guided techniques of three superficial nerves (superficial peroneal, saphenous, and sural nerves).
Superficial peroneal nerve (superficial fibular nerve) (L5, S1, S2)
The patient is positioned supine or semi-lateral with the hip rotated internally to expose the lateral aspect of the leg (Figure 6a). A linear transducer is placed transversely just above the lateral malleolus to identify the fibula. The superficial peroneal nerve is situated superficially between the peroneus brevis (PB) and the extensor digitorum longus (EDL) as a triangular hyperechoic shadow (Figure 6b) under the crural fascia (an oval hyperechoic structure).9 The EDL is anterior to the nerve, while the PB is posterior to the nerve. The needle is introduced in-plane (or out-of-plane), from anterior to posterior direction (Figure 6c), to approach adjacent to the superficial peroneal nerve. Local anesthetic (5-6 ml 0.5% ropivacaine) is sufficient for an effective block (Figure 6d).
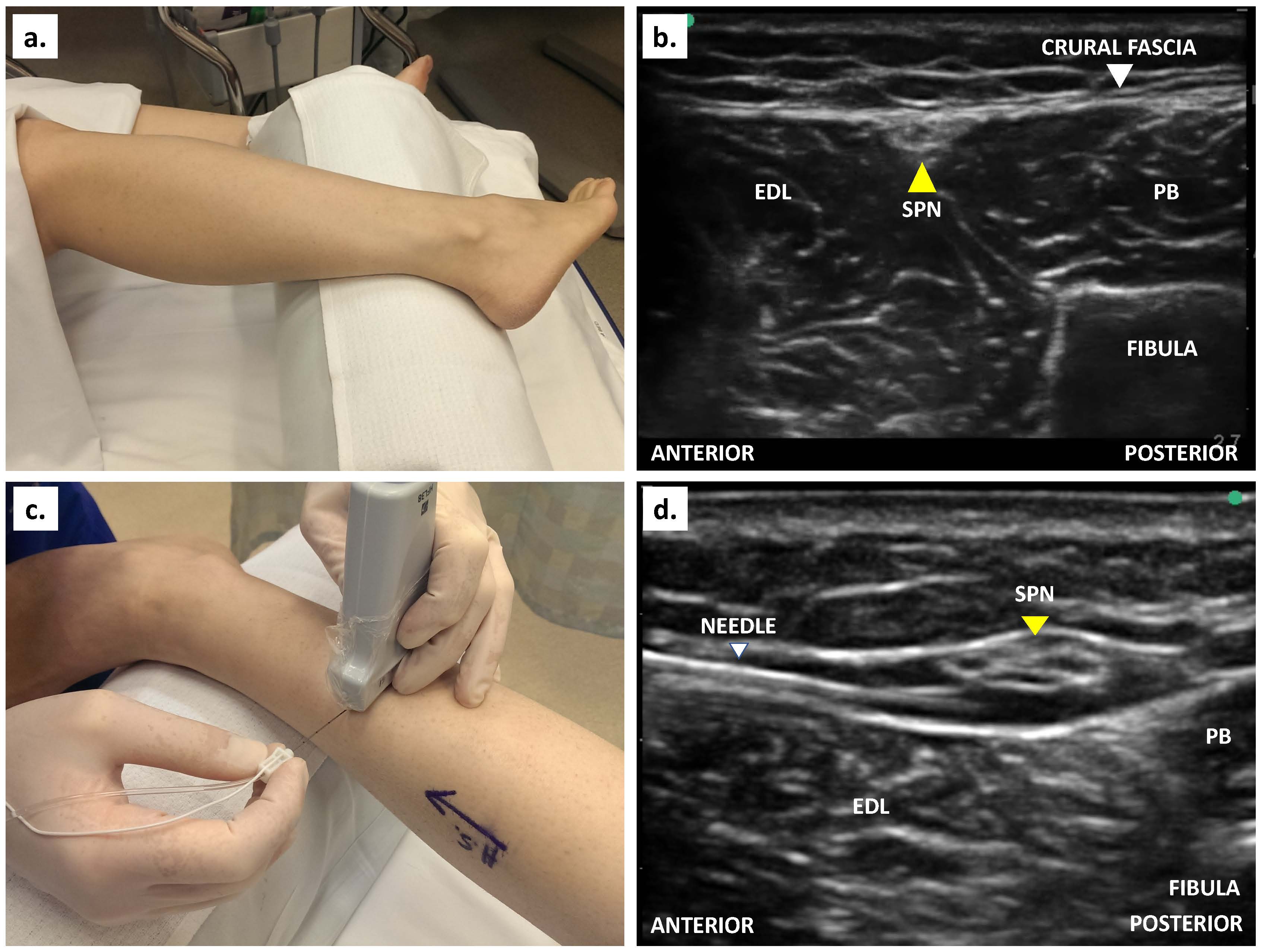
Figure 6. (a) Patient position for superficial peroneal nerve block;(b) Ultrasound scan of the structures slightly proximal to the intermalleolar line; (c) Transverse placement of transducer and in-plane needling proximal to the intermalleolar line (d) In-plane injection to block the nerve. (PB - peroneus brevis, EDL - extensor digitorum longus, SPN - superficial peroneal nerve. Yellow arrowhead denotes superficial peroneal nerve.)
Sural nerve (S1, S2)
The patient is positioned with the knee flexed and internal rotation at the hip, making the posterolateral aspect of the leg accessible. A linear transducer is placed transversely above the lateral malleolus, identifying the peroneus brevis anteriorly and the Achille's tendon posteriorly. The sural nerve (hyperechoic oval) is located anterior to the Achilles tendon (Figure 7a). The needle is introduced in-plane from anterior to posterior (or out-of-plane), proximal to the lateral malleolus (Figure 7b) to advance adjacent to the nerve and local anesthetic (2-4 ml 0.5% ropivacaine) is injected (Figure 7c).
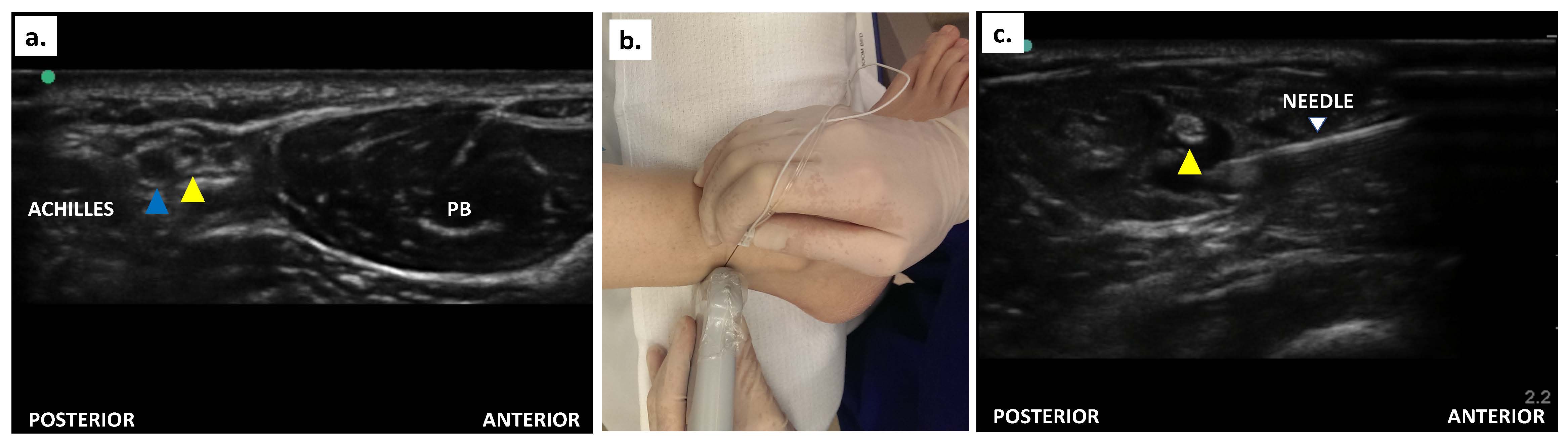
Figure 7. (a) Ultrasound scan of the sural nerve (yellow arrowhead) and short saphenous vein (blue arrowhead) just proximal to the lateral malleolus; (b) Patient positioning, transducer orientation, and needling; (c) In-plane needling to block sural nerve (yellow arrowhead) block.
Saphenous nerve (L2, L3, L4)
The hip is externally rotated. A linear transducer is placed transversely above the medial malleolus to identify the great saphenous vein with the saphenous nerve anterior to it (hyperechoic oval) (Figure 8a). Application of a tourniquet would enhance the appearance of the vein. The needle is introduced in-plane from posterior to anterior (or out-of-plane), proximal to the medial malleolus to approach the saphenous nerve (Figure 8b).10 Local anesthetic (2-4 ml 0.5% ropivacaine) is injected (Figure 8c).

Figure 8. (a) Ultrasound scan of the saphenous vein and nerve proximal to the medial malleolus; (b) In-plane needling for saphenous nerve block; (c) Ultrasound-guided in-plane approach to the saphenous nerve block. (Yellow arrowhead denotes saphenous nerve; blue arrowhead indicates excellent saphenous vein.)
Alternate Approach to Block Superficial Nerves
Ultrasound-guidance is most beneficial for the tibial and deep peroneal nerve blocks. Should one wish to use the landmark technique for the other nerves, the superficial peroneal and saphenous nerves can be anesthetized by subcutaneous infiltration of 10-15 ml local anesthetic anteriorly between medial and lateral malleoli. This can be achieved by using a single anterior injection entry point. Similarly, 4-5 ml of subcutaneous infiltration between lateral malleolus and Achilles tendon provides adequate sural nerve coverage.
Please note that ankle block does not cover the tourniquet pain around the thigh or the calf; therefore, it is only suitable as an analgesic block and perhaps surgical anesthesia for surgeries of short duration.
Conclusion
Ultrasound-guided ankle block enhances the block's reliability, safety, and overall success rate. It also helps to minimize the local anesthetic volume required, thus permitting bilateral ankle block performance. It can easily be performed in most patients for selected surgeries and allows for early ambulation while providing pain relief.
Clinical Pearls
- Compared to a landmark-based ankle block, an ultrasound-guided ankle block is usually done more proximally to the ankle joint as the malleolar prominences hinder appropriate transducer-skin contact.
- We recommend starting with the tibial nerve, as this is a larger nerve and benefits from a longer "soak" time. We advocate a proximal block of the tibial nerve because a distal block may lead to a medial calcaneal branch's sparing. Flexing and extending the great toe generates a “sea-saw” movement of the nerve on the flexor hallucis longus, helping to identify it.
- Care should be exercised not to inject deep into the periosteum as subperiosteal injections are painful. An out-of-plane approach may be easier to perform.
- The superficial peroneal nerve can be blocked either shallow (distal-leg) or deep (mid-leg) to the crural fascia. However, a distal injection can result in missing one of the branches (intermediate or medial branch).11 Therefore, we favor a more proximal injection before the division of the nerve.
- The sural nerve may be omitted if the surgical site is confined to the medial of the foot. If the nerve cannot be easily identified, a perivenous injection may be performed within the fascial compartment. An out-of-plane approach may be easier to perform.
- The saphenous nerve divides into several articular branches proximal to the ankle. Therefore, while a block at or above ankle sufficiently blocks the distal foot, a proximal block (at distal tibia) is needed to provide analgesia for ankle joint surgery itself.12 Application of a tourniquet at mid-calf can help to identify the great saphenous vein in cases where it is not easily visible.
- Keep it simple. Ultrasound-guidance is most beneficial for the tibial and deep peroneal nerve blockage. Skin infiltration on the anterior aspect of the intermalleolar line will block saphenous and superficial peroneal nerves. Infiltration between the lateral malleolus and Achilles tendon will block the sural nerve.
Herman Sehmbi, MBBS, MD, EDRA, EDAIC, MSc (Clinical Trials), is an assistant professor in the department of anesthesia at Western University in London, ON, Canada.

Ushma Jitendra Shah, MBBS, FRCA, EDRA, EDAIC, is an assistant professor in the department of anesthesia at Western University, London, ON, Canada.
Vishal Uppal MBBS, FRCA, EDRA, MSc (Clinical Trials), is an associate professor in the department of anesthesia, perioperative medicine, and pain management at Dalhousie University, Nova Scotia Health Authority and Izaak Walton Killam Health Centre in Halifax, NS, Canada.
References
- Tryba M. Ankle block: A safe and simple technique for foot surgery. Curr Opinion Anesthesiology. 1997;10:361-365. https://journals.lww.com/co-anesthesiology/abstract/1997/10000/ankle_block__a_safe_and_simple_technique_for_foot.16.aspx.
- McLeod DH, Wong DH, Vaghadia H, Claridge RJ, Merrick PM. Lateral popliteal sciatic nerve block compared with ankle block for analgesia following foot surgery. Can J Anaesth. 1995;42:765-9. https://doi.org/10.1007/BF03011173.
- Migues A, Slullitel G, Vescovo A, Droblas F, Carrasco M, Turenne HP. Peripheral foot blockade versus popliteal fossa nerve block: A prospective randomized trial in 51 patients. J Foot Ankle Surg. 2005;44:354-357. https://doi.org/10.1053/j.jfas.2005.07.005.
- Kilicaslan A, Topal A, Erol A, Borazan H, Bilge O, Otelcioglu S. Ultrasound-guided multiple peripheral nerve blocks in a superobese patient. Case reports in anesthesiology 2014;2014:896914. https://doi.org/10.1155/2014/896914.
- Marsland D, Dray A, Little NJ, Solan MC. The saphenous nerve in foot and ankle surgery: Its variable anatomy and relevance. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons 2013;19:76-9. https://doi.org/10.1016/j.fas.2012.10.007.
- Redborg KE, Antonakakis JG, Beach ML, Chinn CD, Sites BD. Ultrasound improves the success rate of a tibial nerve block at the ankle. Reg Anesth Pain Med. 2009;34:256-260. https://doi.org/10.1097/AAP.0b013e3181a343a2.
- Redborg KE, Sites BD, Chinn CD et al. Ultrasound improves the success rate of a sural nerve block at the ankle. Reg Anesth Pain Med. 2009;34:24-28. https://doi.org/10.1097/AAP.0b013e3181933f09.
- Purushothaman L, Allan AG, Bedforth N. Ultrasound-guided ankle block. Continuing Education in Anaesthesia, Critical Care & Pain 2013;13:174-178. https://doi.org/10.1093/bjaceaccp/mkt009.
- Ting PH, Antonakakis JG, Scalzo DC. Ultrasound-guided common peroneal nerve block at the level of the fibular head. J Clin Anesth. 2012;24:145-7. https://doi.org/10.1016/j.jclinane.2011.06.010.
- Tubbs RS, Loukas M, Shoja MM, Apaydin N, Oakes WJ, Salter EG. Anatomy and potential clinical significance of the vastoadductor membrane. Surg Radiol Anat. 2007;29:569-73. https://doi.org/10.1007/s00276-007-0230-4.
- de Leeuw PAJ, Golanó P, Sierevelt IN, van Dijk CN. The course of the superficial peroneal nerve in relation to the ankle position: Anatomical study with ankle arthroscopic implications. Knee Surg Sports Traumatol Arthrosc. 2010;18:612-617. https://doi.org/10.1007/s00167-010-1099-z.
- Eglitis N, Horn J-L, Benninger B, Nelsen S. The importance of the saphenous nerve in ankle surgery. Anesth Analg. 2016;122:1704-1706. https://doi.org/10.1213/ANE.0000000000001168.
Conflicts of Interest: The authors declare that they have no conflicts of interest. All authors have read and approved the manuscript.
All images reproduced with permission from Dr. Herman Sehmbi.

Leave a commentOrder by
Newest on top Oldest on top