Perioperative Management of Patients on Buprenorphine for Opioid Use Disorder
Cite as: Selvamani BJ, Kral L, Swaran Singh T. Perioperative management of patients on buprenorphine for opioid use disorder. ASRA Pain Medicine News 2022;47. https://doi.org/10.52211/asra020123.010.
Background
Opioid use disorder (OUD) is a chronic disease involving misuse of both prescription and illicit opioids. Medication treatment of OUD (MOUD) has been shown to improve outcomes such as increased retention in treatment and decreased mortality and morbidity.1 Buprenorphine (BUP) is a Schedule III opioid that has been shown to be effective for the treatment of OUD.1-4 Several BUP formulations exist with the sublingual and injectable preparations approved for OUD, while the buccal and transdermal preparations are approved for chronic pain. In this article, we will focus on the perioperative management of patients on BUP for OUD.
Based on the current evidence, the authors recommend against routine BUP discontinuation in the perioperative period.
With widespread use of MOUD, anesthesiologists are encountering more patients on BUP presenting for elective as well as emergent surgical procedures. Controversies exist regarding appropriate perioperative management due to the concern that high affinity, long half-life, and partial agonism of BUP at the mu-opioid receptor will interfere with the optimal management of acute postoperative pain in these patients.1 The Treatment Improvement Protocol (TIP) guidelines released by the U.S. Center for Substance Abuse Treatment (CSAT) in 2004 stated that “While patients are taking opioid pain medications, the administration of BUP generally should be discontinued.”2 This recommendation and other published case reports of inadequate pain control in patients on BUP led to the practice of discontinuation of BUP in the perioperative period, which, in turn, introduced management complexities and risks to patients such as relapse and illicit opioid use.
Significance
OUD has reached epidemic proportions in the past two decades resulting in a huge economic burden. In 2017, the U.S. Department of Health and Human Services (HHS) declared OUD a public health emergency. In 2020, opioids were involved in a staggering 68,630 overdose deaths, representing 74.8% of all drug overdose deaths.3 MOUD saves lives.4 Starting BUP is one of the most effective ways to save lives with the number of doses needed to treat to prevent one death being fewer than 3.4 Interrupting BUP therapy may lead to OUD relapse with devastating consequences such as overdose and death.5,6
Buprenorphine Pharmacology
Buprenorphine is a high-affinity, long-acting, partial agonist at the mu-opioid receptor and antagonist at the kappa opioid receptor. Due to its tight binding and low intrinsic activity at the mu-opioid receptor, it is beneficial regarding opioid craving and withdrawal and poses low risks for accidental overdose and respiratory depression. BUP is 30 times more potent than morphine and provides effective analgesia at low to moderate doses.8 When used for analgesia, splitting the BUP dose to three to four times daily is preferred because the analgesic half-life is shorter than the half-life of the drug.9 Owing to its kappa receptor antagonism, BUP also has been shown to be beneficial in the treatment of refractory depression.10 In addition, BUP exerts agonist activity at the delta opioid receptor, the effects of which are not fully understood.
Dilemma in the Perioperative Period
Acute pain management in patients on BUP for OUD is inherently complex with multiple factors (eg, surgery type, anticipated postoperative pain, opioid tolerance, daily BUP dose, feasibility of regional blocks) at play. A literature review yielded mixed results, with some publications advocating for BUP discontinuation well in advance of the planned surgery in anticipation of difficult to treat postoperative pain.11 These recommendations are based on receptor availability studies and case reports of difficult-to-treat pain on patients maintained on BUP.12,13 However, evidence indicates that adequate analgesia could be achieved in BUP-maintained patients in combination with other opioids. Kornfeld et al described a case series of 5 patients maintained on sublingual BUP who underwent 7 major surgeries; adequate pain control was achieved with a combination of BUP, local anesthetics, and full-dose opioids.14 In a retrospective cohort study of 51 patients on either BUP or methadone, no significant correlation was noted between the first 24-hour patient-controlled analgesia (PCA) opioid requirements and preoperative BUP or methadone dose. Patients who did not receive baseline BUP on the day of surgery required longer duration of PCA and higher opioids, whereas patients maintained on BUP required fewer IV breakthrough opioids in the first 24 hours postoperatively.15 Another retrospective cohort study investigating 273 pregnant women who underwent cesarean section delivery did not find any significant difference in postoperative opioid requirements between patients maintained on BUP or methadone.16
An editorial by Lembke et al suggested tapering the BUP dose to 12 mg in the 2-3 days prior to surgery if patients are taking a higher than 12 mg daily dose.17 A review by Quaye and Zhang recommended continuing a BUP home dose for minor procedures and a tapering to 8 mg daily for major procedures.18
Greenwald et al showed conserved availability of mu-opioid receptors at varied doses of BUP (71%-85% at 1 mg, 36%-55% at 4 mg, 20%-35% at 8 mg, 9%-20% at 16 mg, 4%-15% at 24 mg, and 2%-12% at 32 mg).19 These findings are similar to the results of a study by Comer et al estimating mu-opioid receptor availability (21%-31% at 2 mg, 11%-22% at 8 mg and 6%-12% at 32 mg).20 However, the optimal dose of BUP in the perioperative period has not been studied.
The Substance Abuse and Mental Health Services Administration updated its guidelines in 2018 to recommend that most patients continue BUP in the perioperative period due to an increased risk of relapse with discontinuation.21 A recent
systematic review found no evidence favoring discontinuation of BUP in the perioperative period, especially for doses of less than 16 mg daily.22 In another systematic review, Goel et al suggested that the discontinuation of BUP and
introduction of full mu agonist in the perioperative period may be a risk factor for OUD exacerbation.23 A recent review recommended continuing BUP without dose reduction.24 This was supported by a multisociety expert panel in
2021, which recommended that BUP should not be routinely discontinued in the perioperative setting. The panel also concluded that BUP can be initiated in untreated patients with OUD in the perioperative setting to decrease the risk of OUD recurrence
and death from overdose.25
Recommendations Regarding Perioperative Management
This article presents an algorithm detailing the perioperative management of patients on BUP for OUD (Figure 1). Based on the current evidence, the authors recommend against routine BUP discontinuation in the perioperative period. Receptor occupancy studies
show that availability of mu opioid receptors decreases with increasing BUP dosage, which can make pain control challenging with full opioid agonists. Therefore, it may be prudent to consider dose reduction in patients taking high-dose BUP to a total
daily dosage of 16 mg or less to best optimize mu opioid receptor availability and pain control when moderate-to-severe pain is anticipated. Such decisions should involve thorough discussion with the patient, acute pain service, and addiction medicine
service. Multimodal analgesia techniques, including regional blocks, non-pharmacological interventions, opioids, and non-opioid analgesics, should be used as appropriate to optimize analgesia in all patients. Finally, the patient’s outpatient
BUP prescribing provider should be informed of any dose changes and additional prescription opioids upon discharge.
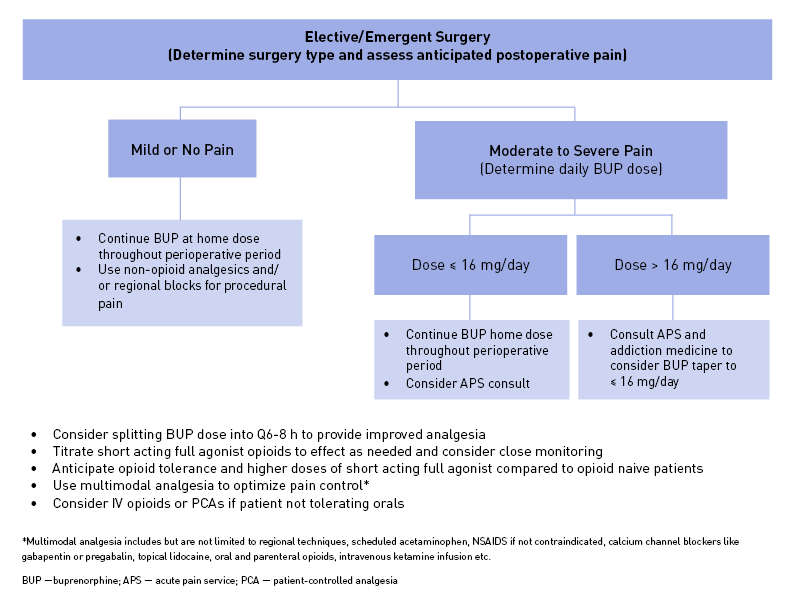
Figure 1: Perioperative Buprenorphine Management Algorithm
Conclusion
There is no convincing evidence that optimal analgesia cannot be achieved with patients maintained on BUP for OUD. However, evidence suggests that discontinuation of BUP is associated with increased rates of relapse and illicit opioid use, leading to poorer outcomes. Therefore, we recommend against routine discontinuation of BUP in the perioperative period. Dose reduction may aid with optimizing postoperative pain control in patients who are on high maintenance doses of BUP and, in this scenario, in which a taper was required as a part of perioperative management. Good communication must be established with the patient’s BUP provider so that an appropriate plan is in place to continue BUP on discharge and titrate BUP dose back to baseline as soon as safely possible.

Breetha Janani Selvamani, MBBS, MD, is a regional anesthesia and acute pain fellow at the University of Iowa Hospitals and Clinics in Iowa City.

Lee Kral, MD, PharmD, BCPS, CPE, is a clinical associate professor in the department of anesthesiology at the University of Iowa Hospitals and Clinics in Iowa City.

Tejinder Singh Swaran Singh, MBBS, MD, FRCA, is a clinical associate professor and the pain medicine fellowship director at the University of Iowa Hospitals and Clinics in Iowa City.
References
- Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 2017;357:j1550. https://doi.org/10.1136/bmj.j1550
- Fudala PJ, Bridge TP, Herbert S, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. New Engl J Med 2003;349(10):949–58. https://doi.org/10.1016/j.drugalcdep.2012.12.010
- Mattick RP, Breen C, Kimber J, et al. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2014;(2):1-85. https://doi.org/10.1002/14651858.CD002207.pub4
- Center for Substance Abuse Treatment Clinical Guidelines for the Use of Buprenorphine in the Treatment of Opioid Addiction. Treatment Improvement Protocol (TIP) Series 40. DHHS Publication No. (SMA) 04-3939. Rockville, MD: Substance Abuse and Mental Health; 2004.
- CDC/NCHS, National Vital Statistics System, Mortality. CDC WONDER, Atlanta, GA: US Department of Health and Human Services, CDC; 2021. https://wonder.cdc.gov/. (Accessed July 10, 2022)
- National Academies of Sciences, Engineering, and Medicine. Medications for opioid use disorder save lives. Washington, DC: The National Academies Press, 2019.
- Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med 2018;169:137-45. https://doi.org/10.7326/M17-3107
- Bentzley BS, Barth KS, Back SE, et al. Discontinuation of buprenorphine maintenance therapy: perspectives and outcomes. J Subst Abuse Treat 2015;52:48-57. https://doi.org/10.1016/j.jsat.2014.12.011
- Williams AR, Samples H, Crystal S, et al. Acute care, prescription opioid use, and overdose following discontinuation of long-term buprenorphine treatment for opioid use disorder. Am J Psychiatry 2020;177(2):117-24. https://doi.org/10.1176/appi.ajp.2019.19060612
- Heit HA, Gourlay DL. Buprenorphine: new tricks with an old molecule for pain management. Clin J Pain 2008;24(2):93-7. https://doi.org/10.1097/AJP.0b013e31815ca2b4
- Vadivelu N, Mitra S, Kaye AD, et al. Perioperative analgesia and challenges in the drug-addicted and drug-dependent patient. Best Pract Res Clin Anaesthesiol 2014;28(1):91-101. https://doi.org/10.1016/j.bpa.2014.02.003
- Lalanne L, Ayranci G, Kieffer BL, et al. The kappa opioid receptor: from addiction to depression, and back. Front Psychiatry 2014;5:170. https://doi.org/10.3389/fpsyt.2014.00170
- Anderson TA, Quaye ANA, Ward EN, et al. To stop or not, that is the question: acute pain management for the patient on chronic buprenorphine. Anesthesiology 2017;126(6):1180-6. https://doi.org/10.1097/ALN.0000000000001633
- McCormick Z, Chu SK, Chang-Chien GC, et al. Acute pain control challenges with buprenorphine/naloxone therapy in a patient with compartment syndrome secondary to McArdle’s disease: a case report and review. Pain Med 2013;14(8):1187-91. https://doi.org/10.1111/pme.12135
- Huang A, Katznelson R, de Perrot M, et al. Perioperative management of a patient undergoing Clagett window closure stabilized on Suboxone® for chronic pain: a case report. Can J Anaesth 2014;61(9):826-31. https://doi.org/10.1007/s12630-014-0193-y
- Kornfeld H, Manfredi L. Effectiveness of full agonist opioids in patients stabilized on buprenorphine undergoing major surgery: a case series. Am J Ther 2010;17(5):523-8. https://doi.org/10.1097/MJT.0b013e3181be0804
- Macintyre PE, Russell RA, Usher KAN, et al. Pain relief and opioid requirements in the first 24 hours after surgery in patients taking buprenorphine and methadone opioid substitution therapy. Anaesth Intensive Care 2013;41(2):222-30. https://doi.org/10.1177/0310057X1304100212
- Vilkins AL, Bagley SM, Hahn KA, et al. Comparison of post-cesarean section opioid analgesic requirements in women with opioid use disorder treated with methadone or buprenorphine. J Addict Med 2017;11(5):397-401. https://doi.org/10.1097/ADM.0000000000000339
- Lembke A, Ottestad E, Schmiesing C. Patients maintained on buprenorphine for opioid use disorder should continue buprenorphine through the perioperative period. Pain Med 2019;20(3):425-8. https://doi.org/10.1093/pm/pny019
- Quaye AN-A, Zhang Y. Perioperative management of buprenorphine: solving the conundrum. Pain Med 2019;20(7):1395-1408. https://doi.org/10.1093/pm/pny217
- Greenwald MK, Comer SD, Fiellin DA. Buprenorphine maintenance and mu-opioid receptor availability in the treatment of opioid use disorder: implications for clinical use and policy. Drug Alcohol Depend 2014;144:1-11. https://doi.org/10.1016/j.drugalcdep.2014.07.035
- Comer SD, Walker EA, Collins ED. Buprenorphine/naloxone reduces the reinforcing and subjective effects of heroin in heroin-dependent volunteers. Psychopharmacology 2005;181:664-75. https://doi.org/10.1007/s00213-005-0023-6
- SAMHSA. Medications for opioid use disorder. Treatment Improvement Protocol (TIP) Series 63, Full Document. HHS Publication No. (SMA) 19- 5063FULLDOC. Rockville, MD; 2018.
- Goel A, Azargive S, Lamba W. The perioperative patient on buprenorphine: a systematic review of perioperative management strategies and patient outcomes. Le patient en période périopératoire sous buprénorphine: revue systématique des stratégies de gestion périopératoire et de l’évolution des patients. Can J Anaesth 2019;66:201-17. https://doi.org/10.1007/s12630-018-1255-3
- Goel A, Azargive S, Weissman JS, et al. Perioperative pain and addiction interdisciplinary network (pain) clinical practice Advisory for perioperative management of buprenorphine: results of a modified Delphi process. Br J Anaesth 2019;123:e333–42. https://doi.org/10.1016/j.bja.2019.03.044
- Buresh, M., Ratner, J., Zgierska, A. et al. Treating perioperative and acute pain in patients on buprenorphine: narrative literature review and practice recommendations. J Gen Intern Med 2020;35:3635-43. https://doi.org/10.1007/s11606-020-06115-3
- Kohan L, Potru S, Barreveld AM, et al. Buprenorphine management in the perioperative period: educational review and recommendations from a multisociety expert panel. Reg Anesth Pain Med 2021;46(10):840-59. https://doi.org/10.1136/rapm-2021-103007
Leave a commentOrder by
Newest on top Oldest on top