Issue Brief: Medicare Policy Updates on Evaluation and Management Visits
Executive Summary
Over the past two years, the Centers for Medicare and Medicaid Services (CMS) has proposed and finalized several policies that will affect documentation, coding, and payment for certain evaluation and management (E/M) visits. Many of CMS’s final policies adopt recommendations from the AMA CPT Editorial Panel and the Relative Value Scale Update Committee (RUC), which reflect broad agreement across the House of Medicine. CMS has also finalized policies that seek to minimize site-of-service differentials for office visits provided in office versus hospital outpatient settings.
Medicare Physician Fee Schedule Updates to Office and Outpatient E/M Visits – Effective January 2021
In the calendar year (CY) 2020 Medicare Physician Fee Schedule (MPFS) final rule, CMS finalized several policies that affect payment for office and outpatient E/M visits starting in 2021. CMS largely left these policies intact in its CY 2021 MPFS final rule, with some key exceptions noted below.
Documentation Requirements and Selection of E/M Visit Level
Effective for office and outpatient E/M service furnished starting January 1, 2021, CMS finalized the following changes that adopt revisions to documentation requirements recommended by the CPT Editorial Panel for office and outpatient E/M visits. CMS believes these changes will reduce documentation burden, including:
- Discontinuation of use of history and physical as determinants for selecting code level
- Level selection and documentation requirements can be determined based on either Medical Decision Making (MDM) or time.
- MDM criteria have been modified to increase clarity and redefine data elements.
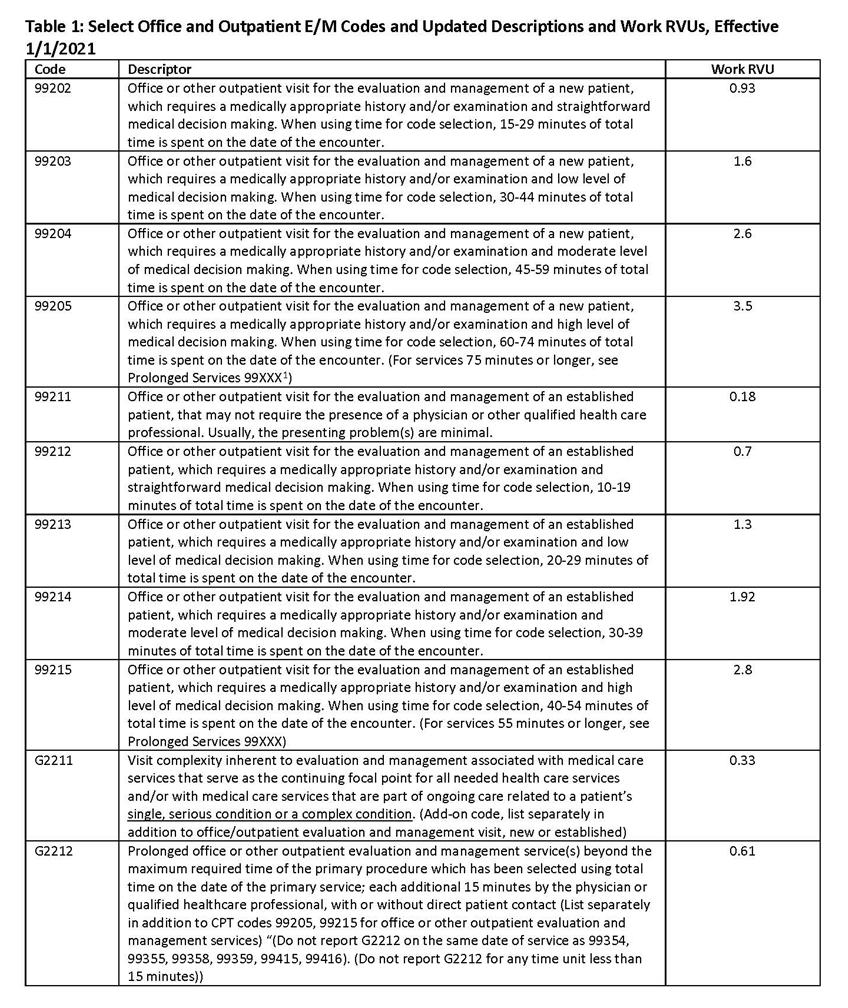
- Minimum time requirements are identified in Table 1 below for the listed codes.
Additional details on the MDM and time revisions, including guidance for level selection, are included on the AMA website.
Available Codes
CMS largely adopted the CPT Editorial Panel’s recommendations for coding office and outpatient E/M visits, including eliminating coding for Level 1 new patient visits. Additionally, CMS finalized the addition of a separate add-on G-code to address complexity for certain types of E/M services that reflect ongoing, longitudinal care, that CMS does not believe is already captured in E/M code values (G2211).[1] CMS provides additional detail on its expectations for use of G2211 in the preamble of the CY 2021 MPFS final rule. Select office and outpatient codes for 2021 are included in Table 1 below, and a full discussion of the 2021 CPT recommended changes are included on the American Medical Association (AMA) website.
At the same time, CMS finalized some deviations from the CPT Editorial Panel’s recommended changes regarding prolonged services. In the CY 2020 MPFS final rule, CMS originally adopted CPT code 99417[2] for prolonged services for time spent by the billing practitioner on the date of service, when selecting level based on time and exceeding the time associated with a level 5 visit. However, in the CY 2021 MPFS final rule, CMS updated this policy and instead adopted a modified version of the CPT prolonged service code (G2212; see Table 1), rather than 99417; this new code requires the maximum amount of time for a level 5 office/outpatient E/M visit to be exceeded by at least 15 minutes before the code can be billed. Additionally, in the CY 2020 MPFS final rule, CMS prohibited the use of two existing prolonged services codes, 99358 and 99359, in conjunction with office and outpatient E/M visits starting in 2021, given the Agency’s concerns about duplication with CPT’s prolonged services code and lack of clarity regarding the use of the code.
Payment
CMS has largely adopted RUC-recommended values for the office and outpatient E/M visits. Values were based on a cross-specialty survey, reflecting increases of between 0 to 46 percent in work RVUs for the E/M codes. Finalized work RVUs, as they will apply starting in 2021, are included in Table 1.
CMS estimates that the above changes would contribute to a net impact of -8.0 percent on total payments to anesthesiologists and a net impact of +7.0 percent for interventional pain management specialists under the MFPS for 2021, relative to total payments in CY 2020. [4] These estimates include the effects of a 10.2 percent reduction in the MPFS conversion factor for CY 2021, which CMS applied to meet statutory budget neutrality requirements.
Additional Information on Office and Outpatient E/M Changes
As noted above, CMS finalized the office and outpatient E/M changes to take place starting January 2021. Notably, the changes above apply strictly to E/M visits furnished in the office and outpatient setting; thus, existing documentation and coding guidelines for other settings will continue to apply into 2021 and beyond.
Policies Addressing Site-of-Service Differentials for Clinic Visits Furnished in Office versus Hospital Outpatient Settings
In the CY 2019 Medicare Outpatient Prospective Payment System (OPPS) final rule, CMS finalized a policy whereby all clinic visits (i.e. HCPCS G0463) furnished in an off-campus hospital outpatient provider-based department (PBD) would generally be paid at an amount intended to eliminate the site-of-service differential for clinic visits provided in an office versus in an off-campus outpatient hospital department. This policy reduced payments for certain off-campus hospital PBDs that were previously excepted from “site-neutralized” payments based on statute. CMS finalized that the payment reduction would be phased-in over two years, with the first half of the reduction scheduled for 2019 and the second half scheduled for 2020.
This policy was challenged by a lawsuit, with an initial District Court ruling against the CMS policy [5] and an appellate decision overturning the lower court ruling.[6] Subsequent to the CMS court victory, the plaintiffs petitioned for a rehearing. The request for rehearing was denied on October 16, 2020.[7] As part of CY 2021 rulemaking, CMS stated that it will consider whether changes are required in the future as the appellants have 90 days in which to seek review from the U.S. Supreme Court.
In the CY 2020 OPPS final rule, citing its appeal rights, CMS finalized that it will move forward with the second year of the phase-in, noting that it will evaluate the rulings and consider appealing the judgment. As such, even those excepted off-campus PBDs whose reduced payments were vacated by the court ruling will receive “site-neutralized” payments for 2020. While continuing uncertainty remains given potential further legal action, in CY 2021 rulemaking, CMS stated its intent to continue the policy in the CY 2021 and beyond.
[1] This code was formerly GPC1X. CMS assigned G2211 as the permanent code for this service in the CY 2021 MPFS final rule, as well as made small adjustments to the code descriptor. The final code descriptor is shown in Table 1.
[2] The code descriptor for 99417 (formerly 99XXX), which CMS did not finalize for 2021, is Prolonged office or other outpatient evaluation and management service(s) (beyond the total time of the primary procedure which has been selected using total time), requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service; each 15 minutes (List separately in addition to codes 99205, 99215 for office or other outpatient Evaluation and Management services) (Use 99XXX in conjunction with 99205, 99215) (Do not report 99XXX in conjunction with 99354, 99355, 99358, 99359, 99415, 99416) (Do not report 99XXX for any time unit less than 15 minutes).
[3] Here and throughout, references to 99XXX in code descriptors reflect original CPT coding, as finalized in 2019. See on the AMA website here. These references do not take into account the more recent assignment by the CPT Editorial Panel of code 99417 to this service, nor CMS’ final policy to replace 99417 with G2212.
[4] See Table 106 of the CY 2021 MPFS final rule.
[5] See American Hospital Association, et al. v. Azar et al., No. 1:18-cv-2084 (D.D.C. Dec. 27, 2018).
[6] See American Hospital Association, et al. v. Azar et al., No. 19-5352 (July 17, 2020).
[7] See American Hospital Association, et al. v. Azar et al., No. 19-5048 (October 16, 2020).