Postherpetic Neuralgia
Author
Honorio T. Benzon, MD
Professor
Department of Anesthesiology
Northwestern University Feinberg School of Medicine
Chicago, IL
Introduction
Herpes zoster and postherpetic neuralgia (PHN) are caused by reactivation of latent varicella zoster virus (VZV). After acute exposure to VZV, either through chicken pox or VZV vaccination, the VZV remains latent in the dorsal root ganglia. The major risk factors for reactivation and resultant herpes zoster are advanced age and immune compromise. Disease, age, and drug related compromise of cellular immunity also increase the incidence of herpes zoster. Other lesser risk factors include Caucasian race, psychological stress, and physical trauma.[1-2]
Pathophysiology
With reactivation, the latent virus in the dorsal root ganglia is allowed to replicate and spread through the sensory ganglia and the peripheral nerve. VZV may also spread into the neighboring spinal cord and to the systemic circulation. VZV replication provokes a cellular immune response which results in neuronal inflammation, hemorrhage and cell death. As the virus spreads to the dermis, a painful maculopapular dermatomal rash erupts. In the following 7-10 days, vesicles form and then crust over. Concomitantly, patients experience stabbing and burning dysesthesias as well as tingling and itching paresthesias, likely the result of acute neuronal inflammation and irritation. While acute herpes zoster is short-lived, the resulting dermatomal pain syndrome can become chronic in some patients. It is speculated that in PHN, demyelination and cell-body destruction occur in the central and peripheral nervous systems, resulting in long term neuropathic pain.
Clinical Features
Herpes zoster is an acute disease process which presents as a classic painful dermatomal rash. There may be pain 2-3 days before the lesions appear. This pre-herpetic pain occurs along the distribution of the involved dermatomes. The maculopapular rash appears, some in clusters, along 2-3 dermatomes. It may take up to two weeks for the lesions to heal. The pre-herpetic pain usually continues during the rash, may improve with healing of the lesions, or may continue as a postherpetic pain. The pain can be constant, intermittent, or stimulus dependent. Allodynia can be the most disabling aspect of PHN.
The risk factors for the development of PHN include the occurrence of pre-herpetic pain, increased herpetic lesions compared to minimal lesions, severe and poorly controlled pain during the acute stage, and advanced age.
Prevention
Antiviral Drugs
The prevention of postherpetic neuralgia (PHN) includes the use of a vaccine and several drugs during the acute phase of the disease. Antiviral agents are effective in reducing the course of the disease and in preventing PHN. Randomized controlled double blind trials have shown that initiation of antiviral therapy within 72 hours of the onset of rash reduce the acute pain and the duration of the postherpetic pain,[3-4] with acyclovir, famciclovir, and valacyclovir having similar efficacy. All three drugs are nucleoside analogues which disrupt viral DNA polymerase and limit VZV’s ability to replicate. Famciclovir was shown to be better than placebo[5] while valacyclovir and famciclovir are equally effective in decreasing the duration of postherpetic neuralgia.[6] Even with optimum preventive therapy, 20-30% of patients develop PHN.[7]
Vaccine
A new herpes zoster vaccine was developed to stimulate the immune system in immunocompetent individuals with the latent infection. This leads to a stronger defensive response if reactivation of the VZV occurs. A study on immunocompetent adults over 60 years of age with a history of chickenpox randomized the patients into zoster vaccine or placebo.[8] The use of a vaccine resulted in a 61% reduction in zoster burden of illness score (P<0.001), a 51% reduction in herpes zoster incidence (P<0.001), and a 66.5% reduction in the incidence of PHN (P<0.001).
Amitriptyline
Amitriptyline given during the acute stage of herpes zoster may decrease the incidence of PHN. Bowsher[9] showed, in a randomized, double-blind, placebo-controlled trial, that patients over 60 years of age who were given 25 mg amitriptyline daily within 48 hours of the rash, had 16% incidence of PHN compared to 35% in the patients who were given placebo.
Nerve Blocks
Most of the published studies on the role of nerve blocks to prevent or treat PHN are case series or retrospective studies.[10-12] Even the studies with a “control” group have problems in experimental design. In one study, patients with acute herpes zoster had either stellate ganglion blocks with bupivacaine or placebo.[13] There was better response in the bupivacaine group (9 out of 10 improved compared to 2 out of 10 in the saline group). Unfortunately, the investigators proceeded with bupivacaine stellate ganglion blocks in the patients who were initially given saline thus losing the “control” nature of the group.[13] Two studies used a historical controls. One study compared stellate ganglion blocks with a previously published thesis.[14] Another study compared the effects of stellate ganglion blocks, epidural local anesthetic with or without a steroid, or peripheral nerve blocks with a paper published several years earlier.[15] Finally, sympathetic blocks were done in both groups in another study, one group had the blocks before the skin eruptions while the other groups had the blocks after the eruptions.[16] In the studies noted,[14-16] the incidence of PHN was the same in the treatment and the “control” groups.
A retrospective study[17] showed that 100% of patients who had the sympathetic blocks (stellate, epidural, and intercostal) within 2 weeks of the onset of rash had complete pain relief compared to 92% when the blocks were performed between 2 weeks and one month of the acute herpes and 80% when the blocks were performed between one and 2 months. Although the studies that showed efficacy of the nerve blocks were not randomized or controlled,[16-18] it showed that the severity of acute pain was diminished by the nerve blocks. It is important to note that there is a relationship between the severity of pain of acute herpes and the incidence of PHN.[19]
There are two randomized and controlled studies on the effect of neuraxial blocks in the prevention of PHN and the results are contradictory. One study compared intravenous acyclovir for 9 days plus prednisolone for 21 days with epidural injections of 6-12 mL 0.25% bupivacaine every 6-8 hours or every 12 hours plus methylprednisolone 40 mg every 3-4 days by epidural catheter for a period ranging from 7 to 21 days.[20] The average number of epidural bupivacaine injections was 2.4. The incidence of pain after one year was 22% in the oral medication group and 1.6% in the epidural group. The incidence of abnormal sensations was 12 % in the medication group and 4% in the epidural group (Table 1).
Another study showed different results. In that study,[21] standard therapy (oral antivirals and analgesics) was compared with standard therapy plus one additional epidural steroid injection of 80 mg methylprednisolone and 10 mg bupivacaine. At 1-month follow-up, the percentage of patients who had pain in the epidural group was significantly less (48% versus 58%). However, the values were not significantly different at 3 month (21% versus 24%) and 6 months (15% versus 17%). It appears from these studies that epidural steroid and local anesthetic injections should be performed at least twice during the acute stage of herpes if it is to be effective in preventing PHN.
| Study Reference number | Duration of acute herpes/PHN | Treatment group | Control group(s) | Results |
|---|---|---|---|---|
| Type of Study | ||||
| Prevention of postherpetic neuralgia | ||||
| Pasqualucci20 P, R, C | < 7 days | Epidural methyl-prednisolone and local anesthetic injections (at least 2 injections) | IV acyclovir and oral prednisolone | Incidence of PHN at one year: 22% after medications and 1.6% after epidural |
| Van Wijck21 P, R, C | < 7 days | Standard treatment and one epidural Methyl-prednisolone and bupivacaine injection | Standard therapy (oral antivirals and analgesics) | Significantly less number of patients in the epidural group had pain at 1 month but not at 3 and 6 months |
| Treatment of postherpetic neuralgia | ||||
| Kikuchi60 P, R, C | PHN > 1 year | Intrathecal methyl-prednisolone and lidocaine | Epidural methyl- prednisolone and lidocaine | Relief in the intrathecal group |
| Kotani59 P, R, C, B | PHN ≥ 1 year | Intrathecal methyl-prednisolone and lidocaine once a week for up to 4 weeks | a) Intrathecal lidocaine b) No treatment | 90% of patients in intrathecal steroid group had good/excellent relief compared to 15% in the intrathecal lidocaine group |
| Catala58 P, R, C | PHN 3 months to 2 years | Blocks (stellate or paravertebral) twice a week to a maximum of 6 | IV lidocaine (3 mg/kg) for 2 hours for 15 consecutive days | At 12 month follow-up, better pain control in the nerve block group |
A non-randomized study showed that the combination of epidural injections with medical management decreases the pain of acute herpes zoster. Epidural injections of local anesthetic and steroid (bolus of 5-7 mL 0.25% bupivacaine and 40 mg methylprednisolone followed by an infusion of 2 mL/hour of 0.125% bupivacaine) and intravenous acyclovir (5 mg/kg three times a day) for seven days was noted to be more effective than intravenous acyclovir alone in shortening the days it took for the pain to significantly decrease.[22] It should be noted that the patients in the acyclovir group were patients who were treated six months earlier. In another study,[23] the same group of investigators compared epidural injections and oral famciclovir (250 mg a day) for seven days to their previous group of epidural injections and intravenous acyclovir.[22] They noted that the duration of pain (decrease in the intensity of pain from 100 to 50 or 100 to 10) was less in the epidural and famciclovir group but the total duration of pain (decrease in the intensity of pain from 100 to 0) was similar in both groups.[23] The use of historical controls in these studies makes it hard for someone to accept their results.
Treatment
Pharmacological Treatment
PHN is usually treated with antidepressants, anticonvulsants, opioids, or a combination of an anticonvulsant and an opioid. Antidepressants were commonly prescribed before the efficacy of anticonvulsants was established, the elderly patients with PHN also could not tolerate higher doses of the antidepressants. The combination of an anticonvulsant and an opioid was noted to be more effective than each drug alone (see below).
Antidepressants
Antidepressants are effective in PHN,[24] a meta-analysis study showed significant efficacy of TCAs in PHN with a number-needed-to-treat (NNT) of 2.6 (Table 2).[25] Amitriptyline has been widely used drug but it is poorly tolerated by the elderly especially it’s sedating and constipating effects. Nortriptyline is tolerated better than amitriptyline and is equally effective.[26] Desipramine[27] is also effective and can be prescribed if the patient experiences sedation with nortriptyline. The side effects of TCAs include sedation, tiredness, dizziness, dry mouth, constipation, urinary retention, weight gain, palpitations, and prolonged QT interval in the ECG.[28] The elderly are especially susceptible to the cardiac toxicity of TCAs and a baseline ECG is recommended.[29] Tricyclic antidepressants impair driving performance during the 1st week of treatment or dose escalation then returns to baseline.[30]
Table 2. Level of Evidence, Numbers-Needed-to Treat, Numbers-Needed to Harm, and Side Effects of Selected Drugs for Postherpetic Neuralgia
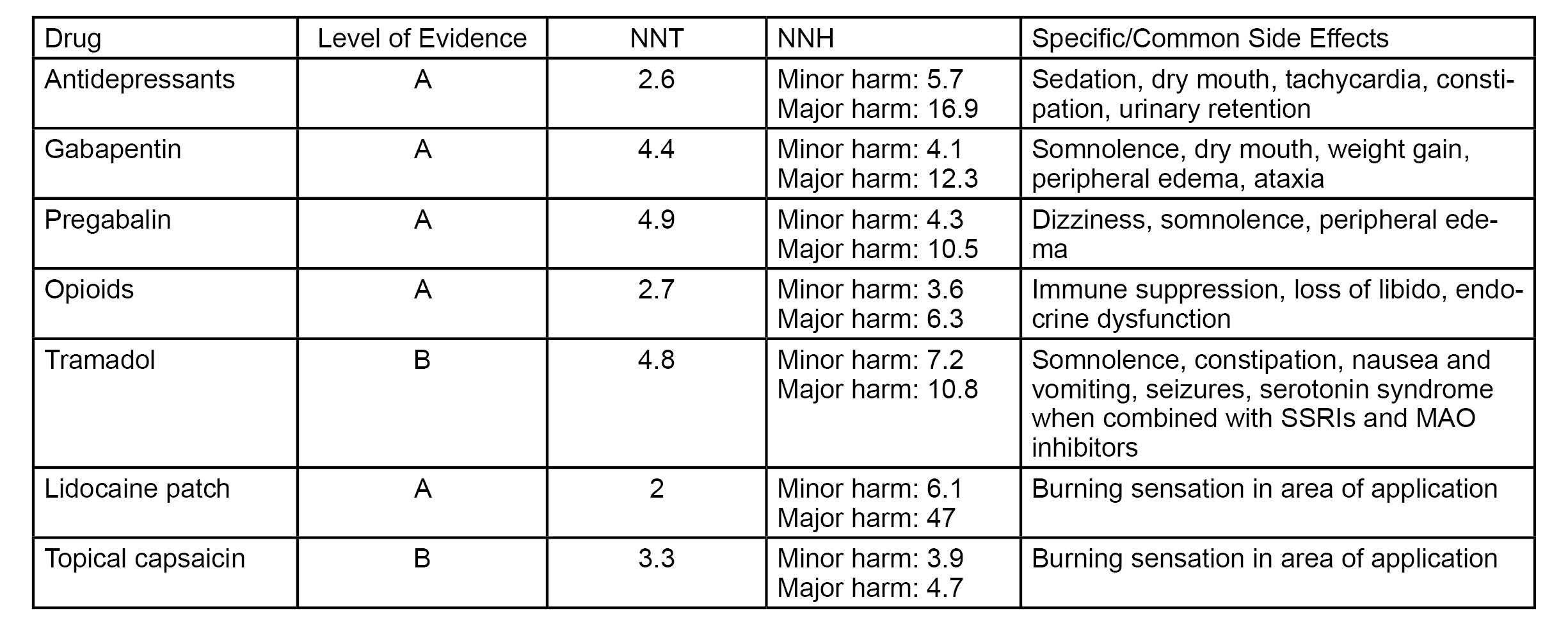
Anticonvulsants
The anticonvulsants gabapentin and pregabalin act on the alpha-2-delta subunit of the calcium channel decreasing the influx of calcium and preventing the release of glutamate, an excitatory neurotransmitter. Studies showed the efficacy of gabapentin PHN, in doses up to 2400 and 3600 mg per day.[31-32] The NNT of gabapentin is 4.4.37 Pregabalin, at doses of 150 to 600 mg per day, is an effective drug in the treatment of PHN.[33-35] The NNT of pregabalin is 4.9 while its NNHs are 4.3 and 6.3 for minor and major harms respectively. The side effects of gabapentin and pregabalin include somnolence, dizziness, fatigue, headache, dry mouth, peripheral edema, and weight gain (Table 2) and their doses should be decreased in patients with impaired renal function.
Opioids
Opioids are also effective in the treatment of PHN. Morphine infusion at 0.3 mg/kg over one hour was noted to be better than placebo and as effective as a lidocaine infusion.[36] Oxycodone, to a maximum dose of 30 mg twice a day, was noted to be more effective than placebo.[37] Opioids such as morphine (mean dose of 91 mg) or methadone (mean dose of 15 mg) reduced pain relief better than placebo.[38] In that study, the investigators noted a trend favoring opioids over nortriptyline or desipramine and more patients preferred the opioid over the two TCA drugs (54% versus 30%). The NNT of opioids is 2.7 while the NNH is 3.6 for minor harm and 6.3 for major harm. The less known side effects of opioids include immune suppression, loss of libido, and endocrine dysfunction. The driving performance of patients on stable doses of opioids is not affected[39-41] but patients who had dose increments greater than 30% within the previous two days showed worsening of their cognitive performance.[42]
The combination of an anticonvulsant and an opioid was noted to be more effective than either agent alone, the superior effect of the combination was attained with lower doses of each drug.[43]
Tramadol
Tramadol is also an effective drug for PHN.[44] The average dose of tramadol used in the study was 275.5 (SD, 89.7) mg per day. The NNT of tramadol is 4.8 and its side effects of tramadol include dizziness, somnolence, constipation, nausea and vomiting (Table 2).
If pain relief is the only criteria then antidepressants and opioids, including tramadol, should be prescribed before anticonvulsants. However, side effects, quality of life, addiction, and regulatory issues make the anticonvulsants the preferred initial treatment for neuropathic pain, specifically PHN.[45]
Local Anesthetics
Lidocaine, either given intravenously, orally, or topically, is effective in PHN. In a meta-analysis review of 19 studies on neuropathic pain (10 studies for intravenous lidocaine and 9 for mexiletine),[46] it was noted that intravenous lidocaine and mexiletine were superior to placebo and equal to morphine, gabapentin, amitriptyline, and amantadine. The median dose of intravenous lidocaine in the studies was 5 mg/kg over 30-60 minutes with the smallest dose at 1.5 mg/kg over one minute. The side effects of intravenous lidocaine are known to anesthesiologists. The median dose of mexiletine in the studies was 600 mg daily (range: 150-300 mg three times a day) with the highest dose at 675 mg three times a day.[46] The side effects of mexiletine involved mostly the gastrointestinal (nausea, vomiting, gastric pain, dry mouth) and central nervous systems (headache, dizziness, tiredness, shakiness, and sleep disturbance).
Lidocaine patch has been shown to be effective in several, prospective, randomized trials.[47-50] The highest blood level of lidocaine that was noted was 0.1 mcg/mL, this indicated minimal systemic absorption of the local anesthetic. The NNT for lidocaine patch is 2. Topical capsaicin has also been shown to be effective in PHN.[51-52] The NNT for topical capsaicin was noted to be 3.3. Capsaicin cream causes local irritation and burning and requires frequent usage to be effective.
NMDA Blocking Drugs
The NMDA-blocking agents such as ketamine have been shown to decrease the pain, allodynia and hyperpathia in 8 patients with PHN[53-54] and that the patients preferred the pain relief of subcutaneous ketamine over its psychotomimetic effects. Memantine is effective in diabetic neuropathy but not in PHN.[55-56]
Interventional Procedures

Figure 1. Lateral fluoroscopic view with needles placed at T5-T6 and T6-T7 interspaces.
Once the tips of the needles were barely inside the subarachnoid space, advancement of the needle was stopped as soon as the dura was entered and cerebrospinal fluid was aspirated.
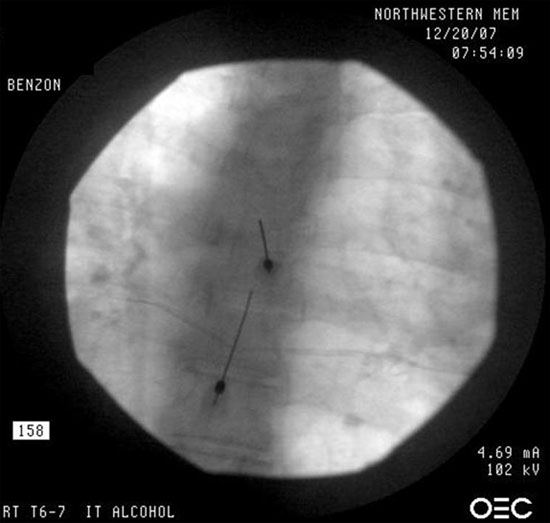
Figure 2. A postero-anterior view showing the needles inserted at the T5-T6 and T6-T7 vertebral levels.
Nerve Blocks
Nerve blocks still have a role in established PHN. A prospective case series of 22 patients showed that the combination of nerve blocks (epidural, intercostal, supraorbital, supratrochlear, and infraorbital) and amitriptyline resulted in greater than 50% relief of pain in 59% and acceptable pain relief in 73% of the patients.[57] In this study, the duration of the PHN was not stated. A randomized study[58] compared nerve blocks (stellate or paravertebral blocks) with intravenous lidocaine infusion (3 mg/kg over 2 hours on 15 consecutive days). At the 3 and 12-month follow-ups, the patients who had the sympathetic blocks experienced better pain control (Table 1).
Intrathecal steroid and local anesthetic injections were reported to be effective in some resistant cases of PHN. A randomized and blinded trial[59] showed that 90% of the patients who had up to 4 weekly intrathecal injections of 60 mg methylprednisolone acetate and 3 mL 3% lidocaine had a good or excellent global pain relief (Table 1). This was in contrast to 15% of the patients who had intrathecal injections of lidocaine only. Interleukin-8 decreased by 50% in the methylprednisolone-lidocaine group but not in the lidocaine-only group or in the no-treatment group. The epidural approach appears not to be as effective as the intrathecal approach.[60]
Spinal Cord Stimulation
Harke[61] reported 28 patients with intractable PHN of more than 2 years duration who responded to spinal cord stimulation (SCS). The efficacy of the SCS was proven by the reappearance of the pain when the stimulator was turned off, and pain relief when it was turned back on. Eight patients discontinued their SCS permanently after 3-66 months because of low pain levels or spontaneous improvements.
Intrathecal Alcohol
Lauretti[62] described several patients who responded to intrathecal alcohol. Benzon1 described a patient who did not respond or could not tolerate the side effects of the medications and had no relief from intrathecal steroid injections.1 The patient responded to intrathecal alcohol injections at T5-T6 and T6-T7 levels (see Figures 1 and 2). The patients of Lauretti[62] had pain relief that lasted 10-13 months while the patient of Benzon1 had relief continued relief at her one- year follow-up.
Evidence Based Treatment Recommendations
Benzon1 recommended the treatment of PHN based on levels of scientific evidence (Table 2).[63] The levels are evidence are:
- Level A: strong research-based evidence provided by generally consistent findings in multiple high quality randomized clinical trials (RCTs);
- Level B: moderate strong research-based evidence provided by generally consistent findings in one high quality randomized clinical trial (RCT) plus one or more low quality RCTs, or generally consistent findings in low-quality RCTs;
- Level C: limited or conflicting research-based evidence provided by one RCT (neither high or low quality) or inconsistent findings in multiple RCTs; and,
- Level D: no research-based evidence i.e, no RCTs.
Based on the above criteria, level A evidence supports the use of the following drugs in the treatment of PHN: antidepressants, anticonvulsants specifically gabapentin and pregabalin, opioids, and topical lidocaine. A combination of an anticonvulsant and an opioid is more effective than either drug given alone. Topical capsacin cream maybe effective but the magnitude of reduction in the patients’ pain scores may not be clinically important. If the pain of PHN cannot be controlled by pharmacological management or intrathecal methylprednisolone and local anesthetic then either intrathecal alcohol or spinal cord stimulations should be offered to the patient.
Summary
The use of antiviral medications during the acute stage of herpes zoster hastens the healing the lesions, decreases the intensity of the pain of acute herpes zoster, and reduces the duration of the postherpetic pain. Epidural steroid and local anesthetic injections given during the acute stage of herpes may decrease the incidence and severity of PHN. Antidepressants are effective in PHN but their side effects limit their widespread use. Anticonvulsants are effective in PHN and have minimal side effects. The combination of an anticonvulsant and an opioid is more effective than either drug given alone. Patients who do not respond to medical management may be offered intrathecal steroid injections. The choice between spinal cord stimulation and intrathecal alcohol depends on the experience and expertise of the physician and the preference of the patient.
References
- Benzon HT, Chekka K, Darnule A, Wille O, Chung B, Malik K. Evidence-based case report: Intrathecal alcohol for postherpetic neuralgia. Reg Anesth Pain Med 2009;34:514-521
- Whitley RJ. A 70-year-old woman with shingles. JAMA 2009;302:73-80
- Balfour HH, Bean B, Laskin OL, et al (and the Burroughs Wellcome Collaborative Acyclovir Study Group). Acyclovir halts progression of herpes zoster in immunocompromised patients. N Engl J Med 1983;308:1448-1453
- Wood MJ, Johnson RW, McKendricl MW, Taylor J, Mandal BK, Crooks J. A randomized trial of acyclovir for 7 days or 21 days with and without prednisolone for treatment of acute herpes zoster. N Engl J Med 1994;330:896-900
- Tyring SK, Barbarash RA, Nahlik JE, Cunningham A, Marley J, Heng M, Jones T, Rea T, Boon, R, Saltzman R. Famciclovir for the treatment of acute herpes zoster: Effects on disease and postherpetic neuralgia. Ann Int Med1995;123:89-96
- Tyring SK, Beutner KR, Tucker BA, Anderson WC, Crooks RJ. Antiviral therapy for herpes zoster. Arch Fam Med 2000;9:863-869
- Dworkin RH, Johnson RW, Breuer J, et al. Recommendations for the management of herpes zoster. Clin Infect Dis 2007;44:S1–26.
- Oxman MN, Levin MJ, Johnson GR, et al. (for the Shingles Prevention Study Group). A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 2005;325: 2271-2284
- Bowsher D. The effects of pre-emptive treatment of postherpetic neuralgia with amitriptyline: a randomized, double-blind, placebo-controlled trial. J Pain Symptom Manage 1997;13:327-331
- Kumar V, Krone K, Mathieu A. Neuraxial and sympathetic blocks in herpes zoster and postherpetic neuralgia: An appraisal of current evidence. Reg Anesth Pain Med 2004;454-461
- Ali NM. Does sympathetic ganglionic block prevent postherpetic neuralgia? Literature review. Reg Anesth 1995;20:227-233
- Wu CL, Marsh A, Dworkin RH. The role of sympathetic nerve blocks in herpes zoster and postherpetic neuralgia. Pain 2000;87:121-129
- Tenicella R, Lovasik D, Eaglstein W. Treatment of herpes zoster with sympathetic blocks. Clin J Pain 1985;1:63-67
- Rutgers MJ, Dirksen R. The prevention of postherpetic neuralgia: A retrospective review of patients treated in the acute phase of herpes zoster. Br J Clin Pract 1988;42:412-414
- Riopelle JM, Naraghi M, Grush KP. Chronic neuralgia incidence following local anesthetic and steroid for relief of pain secondary to herpes zoster. Arch Dermatol 1984;120:747-750
- Yanagida H, Suwa, K, Corssen G. No prophylactic effect of early sympathetic blockade on postherpetic neuralgia. Anesthesiology 1987;66:73-76
- Winnie AP, Hartwell PW. Relationship between time of treatment of acute herpes zoster with sympathetic blockade and prevention of post-herpetic neuralgia: Clinical support for a new theory of the mechanism by which sympathetic blockade provides therapeutic benefit. Reg Anesth 1993;18:277-282
- Hardy D. Relief of pain in acute herpes zoster by nerve blocks and possible prevention of post-herpetic neuralgia. Can J Anaesth 2005;52:186-190
- Schmader KE, Dworkin RH. Natural history and treatment of herpes zoster. J Pain 2008;9:S3-S9
- Pasqualucci A, Pasqualucci V, Galla F, et al. Prevention of postherpetic neuralgia: acyclovir and prednisolone versus epidural local anesthetic and methylprednisolone. Acta Anaesthesiol Scand 2000;44:910-918
- van Wijck AJM, Opstelten W, Moons KGM, et al. The PINE study of epidural steroids and local anaesthetics to prevent postherpetic neuralgia: a randomized controlled trial. Lancet 2006;367:219-224
- Hwang SM, Kang YC, Lee YB, Yoon KB, Ahn SK, Choi EH. The effects of epidural blockade on the acute pain in herpes zoster. Arch Dermatol 1999;135;1359-1364
- Ahn HJ, Lim HK, Lee YB, Hwang SM, Lee WS, Ahn SK, Choi EH. The effects of famciclovir and epidural blockade in the treatment of herpes zoster. J Dermatol 2001;28:208-216
- Max MB. Thirteen consecutive well-designed randomized trials show that antidepressants reduce pain in diabetic neuropathy and postherpetic neuralgia. Pain Forum 1995;4:248-253
- Hempenstall K, Nurmikko TJ, Johnson RW, A’Hern RP, Rice AS. Analgesic therapy in postherpetic neuralgia: A quantitative systematic review. PLoS Med 2005;2:e164
- Watson CP, Vernich L, Chipman M, Reed K. Nortriptyline versus amitriptyline in postherpetic neuralgia: a randomized trial. Neurology 1998;51:1166-1171
- Rowbotham MC, Reisner LA, Davies PS, Fields HL. Treatment response in antidepressant naive postherpetic neuralgia patients: Double-blind, randomized trial. J Pain 2005;6:741-746
- Wu CL, Raja SN. An update on the treatment of postherpetic neuralgia. J Pain 2008;9:S19-S30
- Sansone RA, Todd T, Meier BP. Pretreatment ECGs and the prescription of amitriptyline in an internal medicine clinic. Psychosomatics. 2002;43:250-251
- Ramaekers JG: Antidepressants and driver impairment: empirical evidence from a standard on-the-road test. J Clin Psychiatr 2003;64:20-29
- Rowbotham M, Harden N, Stacey B, Bernstein P, Magnus-Miller L. Gabapentin for the treatment of postherpetic neuralgia: A randomized controlled trial. JAMA 1998;280:1837-1842
- Rice AS, Maton S. Gabapentin in postherpetic neuralgia: A randomized double-blind, placebo-controlled study. Pain 2001;94:215-224
- Dworkin RH, Corbin AE, Young JP, Sharma U, LaMoreaux L, Bockbrader H, Garofalo ES, Poole RM. Pregabalin for the treatment of postherpetic neuralgia. Neurology 2003;60:1274-1283
- Sabatowski R, Galvez R, Cherry DA, Jacquot F, Vincent E, Maisonobe P, Versavel M. The 1008-045 Study Group. Pregabalin reduces pain and improves sleep and mood disturbances in patients with post-herpetic neuralgia: results of a randomised, placebo-
controlled clinical trial. Pain 2004; 109:26-35. - Freynhagen R, Strojek K, Griesling T, Whalen E, Balkenohl M. Efficacy of pregabalin in neuropathic pain evaluated in a 12-week, randomised, double-blind, multicentre, placebo-controlled trial of flexible- and fixed-dose regimens. Pain 2005;115:254-263
- Rowbotham MC, Reisner-Keller LA, Fields HL. Both intravenous lidocaine and morphine reduce the pain of postherpetic neuralgia. Neurology 1991;41:1024-1028
- Watson CP, Babul N. Efficacy of oxycodone in neuropathic pain: a randomized trial in postherpetic neuralgia. Neurology 1998;50:1837-1841
- Raja SN, Haythornthwaite JA, Papagallo M, Clark MR, Travison TG, Sabeen S, Royall RM, Max MB. Opioids versus antidepressants in postherpetic neuralgia: A randomized, placebo-controlled trial. Neurology 2002;59:1015-1021
- Byas-Smith MG, Chapman SL, Reed B, Cotsonis G. The effect of opioids on driving and psychomotor performance in patients with chronic pain. Clin J Pain 2005;21:345-352
- Vainio A, Ollila J, Matikainen E, Rosenberg P, Kalso E: Driving ability in cancer patients receiving long-term morphine analgesia. Lancet 1995;346:667-670
- Sabatowski R, Schwalen S, Rettig K, Herberg KW, Kasper SM, Radruch L: Driving ability under long-term treatment with transdermal fentanyl. J Pain Symptom Manage 2003;25:38-47
- Bruera E, Macmillan K, Hanson J, MacDonald RN: The cognitive effects of the administration of narcotic analgesics in patients with cancer pain. Pain 1989;39 :13-16
- Gilron I, Bailey JM, Tu D, Holden RR, Weaver DF, Houlden RL. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med 2005;352:1324-1334
- Boureau F, Legallicier P, Kabir-Ahmadi M. Tramadol in post-herpetic neuralgia: A randomized double-blind, placebo-controlled trial. Pain 2003;104:323-331
- Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Algorithm for neuropathic pain: an evidence-based proposal. Pain 2005;118:289-305
- Tremont-Lukats IW, Challapalli V, McNicol ED, Lau J, Carr DB. Systematic review and meta-analysis: Systemic local anesthetics for neuropathic pain. Anesth Analg 2005;101:1739-1749
- Rowbotham, MC, Davies PS, Verkempinck C, Galer BS. Lidocaine patch: Double-blind controlled study of a new treatment method for postherpetic neuralgia. Pain 1996;65:39-44
- Galer BS, Rowbotham MC, Perander J, Friedman E. Topical lidocaine patch relieves postherpetic neuralgia more effectively than a vehicle topical patch: Results of an enriched enrollment study. Pain 1999;80:533-538
- Meier T, Wasner G, Faust M, Kuntzer T, Ochsner F, Hueppe M, Bogousslavsky J, Baron R. Efficacy of lidocaine patch 5% in the treatment of focal neuropathic pain syndromes: A randomized double-blind placebo-controlled study. Pain 2003;106:151-158
- Galer BS, Jensen MP, Ma T, Davies PS, Rowbotham MC. The lidocaine patch 5% effectively treats all neuropathic pain qualities: results of a randomized double-blind, vehicle-controlled, 3-week efficacy study with use of the neuropathic pain scale. Clin J Pain 2002;18:297-301
- Bernstein JE, Korman NJ, Bickers DR, Dahl MV, Miilikan LE. Topical capsaicin treatment of chronic postherpetic neuralgia. J Am Acad Dermatol 1989;21:265-270
- Watson CP, Tyler KL, Bickers DR, Millikan LE, Smith S, Coleman E. A randomized vehicle-controlled trial of topical capsaicin in the treatment of postherpetic neuralgia. Clin Ther 1993;15:510-526
- Hocking G, Cousins MJ. Ketamine in chronic pain management: An evidence-based review. Anesth Analg 2003;97:1730-1739
- Eide PK, Jorum E, Stubhaug A, Bremmes J, Breivik H. Relief of postherpetic neuralgia with the N-methyl-D-aspartic acid receptor antagonist ketamine: a double-blind, cross-over comparison with morphine and placebo. Pain 1994;58:347-354
- Eisenberg E, Kleiser A, Dortort A, Haim T, Yarnitsky D. The NMDA (N-methyl-D-aspartate) receptor antagonist memantine in the treatment of postherpetic neuralgia: a double-blind placebo-controlled study. Eur J Pain 1998;2:321-327
- Sang CN, Booher S, Gilron I, Parada S, Max MB. Dextromethrophan and memantine in painful diabetic neuropathy and postherpetic neuralgia: efficacy and dose-response trials. Anesthesiology 2002;96:1053-1061
- Dureja GP, Bhalla AP. Multimodality regimen for the management of postherpetic neuralgia. The Pain Clinic 1992;5:15-19
- Catala E, Ferrandiz M, Aliaga L, Serra R,Castro MA, Villar LJM. Intravenous lidocaine compared with sympathetic blocks as treatment for post-herpetic neuralgia. Pain Clin 1994;7:205-210
- Kotani N, Kushikata T, Hashimoto H, Kimura F, Muraoka N, Yodono M, Asai M, Matsuki A. Intrathecal methylpredisolone for intractable postherpetic neuralgia. N Engl J Med 2000;343:1514-1519
- Kikucki A, Kotani N, Sato, T, Takamura K, Sakai I, Matsuki A. Comparative therapeutic evaluation of intrathecal versus epidural methylprednisolone for long-term analgesia in patients with intractable postherpetic neuralgia. Reg Anesth Pain Med 1999;24:287-293
- Harke H, Gretenkort P, Ladleif HU, Koester P, Rahman S. Spinal cord stimulation in postherpetic neuralgia and in acute herpes zoster pain. Anesth Analg 2002;94:694-700
- Lauretti GR, Trevelin WR, Frade LP, Lima CPR. Spinal alcohol neurolysis for intractable thoracic postherpetic neuralgia after test bupivacaine spinal analgesia. Anesthesiology 2004;101:244-247
- Malik K, Benzon HT. Radiofrequency applications to dorsal root ganglia: a literature review. Anesthesiology 2008;109-527-542
Leave a commentOrder by
Newest on top Oldest on top