Ultrasound Guided Intercostal Nerve Steroid Injection
Authors
Shankar Hariharan, MD
Associate Professor
Department of Anesthesiology
Medical College of Wisconsin & Zablocki VA Medical Center
Milwaukee, WI
Commentary
Bernhard Moriggl, MD
Professor
University of Innsbruck
Innsbruck, Austria
Introduction
In the perioperative setting, intercostal nerve blocks have been in use for many decades.[1] By their constant location, they provide an easy target for access in interventions. Intercostal nerves have been blocked with local anesthetics, steroids and have also undergone neurolysis in the management of chronic chest wall pain originating from the nerves.[2-5] The causes for these types of pain range from trauma, cancer, post herpetic neuralgia, iatrogenic following thoracotomy or chest tube placement.[6]
Anatomy
The intercostal nerve originates from the ventral rami of the thoracic spinal nerve. It is a mixed nerve containing both sensory and motor fibers. The first intercostal nerve supplies the arm through a major communication with the brachial plexus and has no anterior cutaneous branch. The 12th intercostal nerve runs in the abdominal wall and is called the subcostal nerve. After exiting from the spine it is located between the pleura and the posterior intercostal membrane and subsequently traverses the membrane to lie deep to or in the internal intercostal muscle. They hug the lower border of the corresponding rib along with the vascular bundle. The collateral branch of the intercostal nerve runs along the upper border of the rib below. Besides the muscular branches to the intercostal muscles, latissmus dorsi, serratus anterior and the abdominal wall muscles there are sensory branches to the pleura, peritoneum, anterior and lateral chest and abdominal walls. At the angle of the rib, approximately 5–8 cm from the medial end of the rib, the inferior border of the rib becomes sharper. The lateral branch of the intercostal nerve pierces the external intercostal muscle at the axillary line and divides into anterior and posterior branches to supply the lateral side of the chest. The anterior branch exits near the midline and divides into medial and lateral branches to supply the anterior portion of the chest wall.[7-8]
Traditional Techniques
Both landmark and fluoroscopic guided techniques are utilized for the blockade of the intercostal nerve. With the patient prone, the appropriate rib is palpated lateral to the costal angle and the needle entry is designed to contact the lower border of the rib. From here it is walked off to slip beneath the rib and into the intercostal groove where it is advanced a couple of millimeters prior to injection and after negative aspiration for air and blood. The typical location of the pleura is just a few more millimeters deeper to the intercostal nerve. Thus the intercostal nerve block procedure poses a risk of pneumothorax which ranges from 0.073 % to 19%.[9-11] Being accompanied by the vascular bundle, the risk of intravascular injection or a hematoma is also a threat.[10]
The fluoroscopic guided technique is performed with the patient prone. The appropriate rib is identified under fluoroscopic AP view and the needle is entered in the inferior margin of the rib lateral to the costal angle. Following negative aspiration, a contrast injection is performed to ensure appropriate spread prior to local anesthetic / steroid injection.[2] As pleura cannot be visualized with fluoroscopy, the risk of pneumothorax exists.
Ultrasound Guided Technique
Usually a linear array transducer with frequency ranges from 5–13 MHz is utilized. The ribs are identified under sonography by their characteristic gently curved hyperechogenic surface outline and the acoustic shadow underneath them in a parasagittal view (perpendicular to the ribs). Between adjacent ribs, the intercostal muscles and pleura can be identified. The pleura appears as a hyperechoic line moving in and out of view with a gliding action during respiration. Initial scanning is performed in the transverse plane of the rib to identify the level. The location of the appropriate level is performed by scanning from the 12th rib (caudad) as it is short and then the transducer is moved upwards (cephalad) while counting the ribs and marking with a skin marker to reach the appropriate level. The angle of the rib, located approximately 6 cm from the spinous process, is the ideal location for intercostal nerve block as branching of the main nerve has not yet taken place.
Once the appropriate level is reached, the depth of field is adjusted to visualize the pleura. A longitudinal scan along the longitudinal axis of the rib may be performed when the rib will appear as a hyperechoic line spanning the entire screen. Once the rib is identified in this view, the transducer is moved caudad to slip into the intercostal space to visualize the musculature and the vessels. The nerve may be seen rarely with tilting of the transducer cephalad. Color flow Doppler is helpful for identifying the vessels.
Once the level, vessels and the depth to the pleura have been identified, injection may be performed in real time either in plane or out of plane. Lateral to the costal angle, the needle target is the internal intercostal muscle as the innermost internal intercostal is poorly defined. For the out of plane technique (the authors preferred technique), the transducer is placed longitudinal (parasagittal oblique) to capture a transverse view of the rib and from the midpoint of the transducer a 25 G 5 cm needle (shorter than the pleural depth) is introduced to the target avoiding the vessels and watching for tissue movement. Hydrolocalization is used to ensure correct location prior to the injectate (Figure 1). With the in plane technique, with the transducer in a parasagittal oblique plane to capture a transverse view of the rib, the needle is introduced from the inferior margin of the transducer, usually from the superior border of the rib below, to reach the target under real time ultrasound guidance.[12] As visualization of a 25 G needle may be difficult with this technique a larger needle may be chosen.
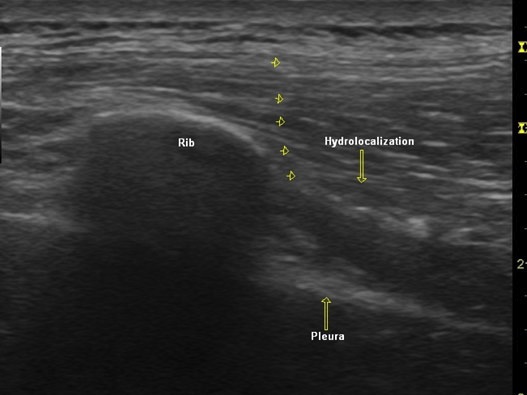 Figure 1. Parasagittal sonogram showing a transverse view of the rib, pleura and intercostal space. The arrowheads point to a 25 G needle inserted in an out of plane approach. Using a hydrolocalization technique, the spread of injectate is observed in the external intercostal muscle.
Figure 1. Parasagittal sonogram showing a transverse view of the rib, pleura and intercostal space. The arrowheads point to a 25 G needle inserted in an out of plane approach. Using a hydrolocalization technique, the spread of injectate is observed in the external intercostal muscle.
An alternative in plane approach is to align the transducer in line with the longitudinal axis of the designated rib, and then to slide down to the intercostal space to visualize the cross sectional view of all the muscle layers and pleura (Figure 2). The needle is then introduced from the medial edge of the transducer to reach the inner intercostal muscle. Hydrolocalization is recommended again once the external intercostal muscle is reached to protect against advancing too far and causing a pneumothorax. Subsequently the needle may be advanced further into the internal intercostal muscle prior to injection. Following the injection, it may safe to perform a safety check scan to visualize the pleura. If a pneumothorax occurs the normal gliding of the pleura with respiration becomes absent along with the absence of “comet tail” artifacts. The “Comet tail” artifacts appear as hyperechoic perpendicular lines in normal pleura.[13]
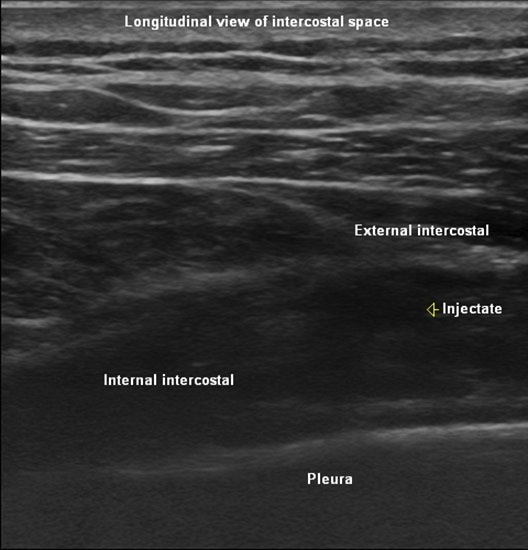
Figure 2. Longitudinal sonographic view with the transducer placed parallel to the ribs in the intercostal space showing the cross sectional view of the external and internal intercostal muscles besides the pleura. The injectate may be visualized in the internal intercostal muscle.
Literature Review
The earliest report of the use of ultrasound Doppler for intercostal nerve block was in 1988.[14] The use of ultrasound guidance for intercostal block was recommended from the personal experience in a review.[15]They recommend the out of plane technique with hydrolocalization to access the intercostal space. Another case report reported the use of ultrasound guidance for cryoablation of the intercostal nerve for post thoracotomy pain.[16] The authors performed the procedure with the patient in a lateral decubitus position. They approached from the superior border of the inferior rib. No complications have yet been reported with this technique. More recently there was a case series from 2013 that reviewed two patients with post-thoracotomy pain and one patient with intercostal neuralgia secondary to vertebral fractures; each of the patients from this case series reported decreased pain after ultrasound guided cryoablation.[17]
In the pediatric population ultrasound guided block is indicated for the reasons similar that the block is used for adult patients. Indications include pain following trauma, thoracic, or upper abdominal surgeries. In children the intercostal block is most placed at the posterior axillary line while the patient is in the semi-prone position.[18] Alternately the placement has been described with the patient in the lateral position and the block placed at the posterior axillary line.[19]
Shankar et al completed a retrospective review of 39 blocks from a single institution who received intercostal steroid injections for pain in the distribution of the intercostal nerves. This study compared blocks performed under either fluoroscopic guidance with contrast confirmation to ensure location within the neurovascular bundle or with the use of ultrasound guidance.[20] In each patient the pre-procedure visual analog scale (VAS), post-procedure VAS, and the duration of pain relief were compared between the two techniques. In this instance the median change in the VAS for the fluoroscopic guided blocks and ultrasound guided techniques were -5.000 and -4.000, respectively, and duration of pain relief with a median difference of 2 weeks. Ultimately the authors concluded that the relief was similar for the two blocks.
Bhatia et al compared intercostal blocks placed with ultrasound versus anatomic landmarks for accuracy and safety utilizing injections in cadavers in a 2-phase study.[21] In each phase of the study the type of injection was randomized and performed by a physician that was trained in both ultrasound and anatomic landmark techniques. In the first phase of the study there were 6 injections of dye injected with each injection that was followed by an anatomist blinded to the technique for the technique for dye injection. The second phase of the study involved 37 injections of contrast using both landmark and ultrasound techniques followed by evaluation of the spread of contrast on fluoroscopy. During of the evaluation of the first phase of the study staining of the intercostal nerve was found for 5 of 6 ultrasound-guided injections but in the anatomic landmark technique resulted in correct injection in 2 of 6 intercostal spaces. No intravascular injection was found on dissection with either of the guidance techniques. In the second phase of the study, ultrasound-guidance was associated with intercostal spread for 36 of the 37 injections but only in 26 of the 37 injections with landmark guidance.
In 2013 Ozkan et al described a randomized, double-blinded, controlled study which used ultrasound-guided intercostal nerve blocks in the 11th and 12th intercostal space for managing postoperative pain and tramadol use following percutaneous nephrolithotomy.[22] This study involved 40 patients that were randomized to either a intercostal nerve block using ultrasound and neurostimulation or a sham procedure where they had needle placement without injection. Following the percutaneous nephrolithotomy visual analog scale scores at all follow-up times were found to be significantly lower in the intercostal nerve block group than in the control group (p < 0.05) and the authors determined that this was a appropriate analgesia for this surgical procedure.
References
- Moore DC, Bridenbaugh LD. Intercostal nerve block: Indications, technique and complications. Anesth Analg 1962; 41:1-10.
- Cohen SP, Sireci A, Wu CL, Larkin TM, Williams KA, Hurley RW. Pulsed radiofrequency of the dorsal root ganglia is superior to pharmacotherapy or pulsed radiofrequency of the intercostal nerves in the treatment of chronic postsurgical thoracic pain. Pain Physician 2006;9:227-35.
- Green CR, de Rosayro M, Tait AR. The role of cryoanalgesia for chronic thoracic pain: results of a long-term follow up. J Natl Med Assoc 2002;94:716-720.
- Byas-Smith MG, Gulati A. Ultrasound-guided intercostal nerve cryoablation. Anesth Analg 2006;103:1033-5.
- Stolker RJ, Vervest AC, Groen GJ. The treatment of chronic thoracic segmental pain by radiofrequency percutaneous partial rhizotomy. J Neurosurg 1994;80:986-92.
- Williams EH, Williams CG, Rosson GD, Heitmiller RF, Dellon AL. Neurectomy for treatment of intercostal neuralgia. Ann Thorac Surg 2008;85:1766-70.
- Moore DC. Anatomy of the intercostal nerve: its importance during thoracic surgery. Am J Surg 1982;144:371-373.
- Davies F, Gladstone RJ, Stibbe EP. The anatomy of the intercostal nerves. J Anat 1932; 66(Pt 3):323-33.
- Shanti CM, Carlin AM, Tyburski JG. Incidence of pneumothorax from intercostal nerve block for analgesia in rib fractures. J Trauma 2001;51:536-9.
- Dangoisse M, Collins S, Glynn CJ. Haemothorax after attempted intercostal catheterisation. Anaesthesia 1994;49:961-3.
- Moore DC. Intercostal nerve block for postoperative somatic pain following surgery of thorax and upper abdomen. Br J Anaesth 1975;47 suppl: 284-6.
- Peng PWHBS, F.R.C.P.C., Narouze S. Ultrasound-guided interventional procedures in pain medicine: A review of anatomy, sonoanatomy, and procedures: Part I: Nonaxial structures. Reg Anesth Pain Med 2009;34:458-74.
- Reissig A, Kroegel C. Accuracy of transthoracic sonography in excluding post-interventional pneumothorax and hydropneumothorax: comparison to chest radiography. Eur J Radiol 2005;53:463-70.
- Vaghadia H, Jenkins LC. Use of a doppler ultrasound stethoscope for intercostal nerve block. Can J Anaesth 1988;35:86-9.
- Curatolo M, Eichenberger U. Ultrasound-guided blocks for the treatment of chronic pain. Techniques in Regional Anesthesia and Pain Management 2007;11:95-102.
- Byas-Smith MG, Gulati A. Ultrasound-guided intercostal nerve cryoablation. International Anesthesia Research Society 2006;103:1033-1035.
- Connelly NR, Malik A, Madabushi L, Gibson C. Use of ultrasound-guided cryotherapy for the management of chronic pain states. J Clin Anesth. 2013 Dec;25(8):634-6.
- Bhalla T, Sawardekar A, Dewhirst E, Jagannathan N, Tobias JD. Ultrasound-guided trunk and core blocks in infants and children. J Anesth. 2013 Feb;27(1):109-23.
- Jagannathan N, Suresh S. Truncal blocks in children. Techniques in Regional Anesthesia and Pain Management (2007) 11, 260-264.
- Shankar H, Eastwood D. Retrospective comparison of ultrasound and fluoroscopic image guidance for intercostal steroid injections. Pain Pract. 2010 Jul-Aug;10(4):312-7.
- Bhatia A, Gofeld M, Ganapathy S, Hanlon J, Johnson M. Comparison of anatomic landmarks and ultrasound guidance for intercostal nerve injections in cadavers. Reg Anesth Pain Med. 2013 Nov-Dec;38(6):503-7.
- Ozkan D, Akkaya T, Karakoyunlu N, Arik E, Ergil J, Koc Z, Gumus H, Ersoy H. Effect of ultrasound-guided intercostal nerve block on postoperative pain after percutaneous nephrolithotomy: prospective randomized controlled study. Anaesthesist. 2013 Dec;62(12):988-94.
Leave a commentOrder by
Newest on top Oldest on top