How We Do It: Ultrasound-Guided Thoracic Paravertebral Block, feedback
This article originally appeared in ASRA News, Volume 13, Number 1, pp 10-12 (February 2013).
Author
David Webb, MD, Lucien Catania, MD, Mario Montoya, MD, Jacques E Chelly, MD, PhD, MBA
Division of Acute Interventional Perioperative Pain and Regional Anesthesia
University of Pittsburgh Department of Anesthesiology
Pittsburgh, PA
To the Editor:
We read with interest the excellent article by Dr. Myles Conroy published in the August 2012 ASRA News titled, “How I Do It: Ultrasound-guided Thoracic Paravertebral Blockade.” The author provided a comprehensive discussion of thoracic paravertebral block (TPVB), which included an informative and descriptive overview of surface anatomy and sonoanatomy, relationship to the thoracic spine, and a detailed discussion including ultrasound-guided visual images of two techniques, the transverse and parasagittal approaches.[1] In this letter, we present how we perform an ultrasound-guided thoracic paravertebral block to further expand on Dr. Conroy’s article with the intention to initiate and cultivate collegial dialogue.
When performing an ultrasound-guided transverse in-plane approach, the author states that the needle insertion point should be at least 2 cm lateral to the tip of the transverse process to allow an insertion angle adequate for needle visualization. Utilizing ultrasound guidance, the needle is inserted in-plane and directed medially between the transverse process and pleura. The tip of the needle then traverses the superior costo-transverse ligament and enters the paravertebral space where local anesthetic is deposited. In support of this approach, the author referenced an article by Dr. Manoj Karmakar related to TPVB, which states, “A number of ultrasound-guided approaches to the paravertebral space have been advocated, and no particular approach has been proven superior.”[2] After performing an extensive evaluation of the current literature and an institutional retrospective review of our data utilizing ultrasound guided thoracic paravertebral blocks, we believe there is evidence to support a superior technique. We advocate the use of an ultrasound-guided parasagittal in-plane approach as opposed to the transverse in-plane technique when performing TPVB.
The University of Pittsburgh Medical Center (UPMC) Acute Interventional Perioperative Pain Service (AIPPS) performed 30,937 blocks in 2010-11, including 8,637 TPVB. In our institution, TPVBs are performed for postoperative pain control following abdominal, thoracic, and urological surgical procedures. TPVBs are performed using either a blind classic or an ultrasound-guided approach. In this regard, we are presently evaluating if the use of ultrasound guidance provides more effective analgesia than the blind approach. If post-operative analgesia is required for more than 24 hrs, a continuous TPVB is indicated. Ropivacaine 0.5% is our local anesthetic of choice (5 ml per level in the case of single PVBs or 5 ml through the introducer needle followed by 10 ml via the PVB catheter in the case of a continuous block). Using contrast dye, we have previously demonstrated that the administration of 10 ml of local anesthetic in the paravertebral space may distribute 1-2 segments above and between 3-5 segments below the level of the injection (Fig.1).[3]
/webb_1.jpg?sfvrsn=17244e31_1)
Figure 1. X-Ray of the thoracic paravertebral space at the level of T5, demonstrating multi-level distribution of 10 ml of injected contrast dye
Contrary to Dr, Conroy, we advocate the use of the parasagittal in-plane approach when performing TPVB. We have found this approach to be highly efficacious, readily reproducible with minimal complications, and unlikely to produce systemic side effects since epidural spread is reduced. Dr. Conroy notes that, in his experience, the parasagittal in-plane approach is more difficult to perform than the transverse in-plane approach. He attributes this to the necessarily steep angle required for insertion of the needle, which results in poor visualization of the needle tip as it is guided into the paravertebral space posterior to the pleura. At our institution, the parasagittal in-plane approach has been our sole technique over the past 8 years, and we do not find the approach to be particularly difficult. We believe that with experience and proper technique, adequate needle visualization can be achieved
Evidence
In previously-published reports and in Dr.Conroy’s article, it is well-established that the transverse approach can result in epidural blockade, secondary to the documented spread of the local anesthetic solution into the epidural space.[4,5] The clinical presentation associated with epidural blockade may include numerous adverse systemic symptoms, which manifest clinically as significant hypotension, lower extremity weakness, and bradycardia. The incidence of epidural spread while performing ultrasound-guided TPVB with a “latero-medial” direction of the needle has been reported up to 30%,[4] and, in one series, as high as 70%.[5] This is in sharp contrast to the reported incidence of hypotension (4%) and epidural or intrathecal spread (1%) with the blind, nerve stimulator-guided perpendicular technique.[6] The increased incidence of systemic symptoms observed with the transverse approach is most likely related to epidural spread, which we believe is due to the “latero-medial” introduction and guidance of the needle utilized in this approach. When the needle is advanced latero-medially to the paravertebral space, it also becomes aligned directly with the neural foramen, which is an anatomic point of entry into the epidural space. With this orientation, the needle tip and/or the catheter can inadvertently enter the epidural space. An alternative mechanism, resulting in epidural spread can occur if the jet of local anesthetic diffuses, or if the multiport catheter passes through the neural foramen, thus entering the epidural space. This can occur even if the needle is properly placed in the paravertebral space.
With the parasagittal technique, the neural foramen is approached perpendicularly, making epidural spread unlikely. Using a blind technique, Naja et al. reported a 4% incidence of epidural spread.[7] Chelly et al. have advocated in favor of the parasagittal approach to reduce the risk of epidural spread when performing ultrasound-guided TPVB. Since the needle is advanced under direct visualization, and the spread of the local anesthetic can be monitored, this approach may reduce complications and provide increased safety when performing TPVB.[8,9]
Parasagittal Ultrasound-Guided Technique
The patient is placed in a sitting position. The relevant skin landmarks, including thoracic spinous processes, are identified and marked. A point 2-2.5 cm lateral to the tip of the spinous processes is measured and marked. After proper preparation and disinfection of the area, a 2-5 MHz low frequency curvilinear array transducer (a 10 MHz high frequency linear array transducer may be used for higher thoracic levels) is placed parallel to the spinous process. The transverse process (TP), the costo-transverse ligament (CTL) and the pleura (P) are identified. “Tilting” of the probe may allow for better visualization of the costo-transverse ligament and pleura. Skin and the planned trajectory of the block needle are infiltrated with 1% lidocaine (5 ml) under ultrasound-guidance. An 18-gauge Tuohy tip needle

Figure 2. Positioning of the ultrasound probe and the needle with in-plane parasagittal approach
connected to extension tubing is inserted at the cephalic end of the transducer (Fig. 2). Using an in-plane technique, the needle is directed towards the CTL. The passage of the needle through the CTL is associated with a tactile “pop”(Fig. 3A). After aspiration is negative for blood, 5-7 ml of ropivacaine 0.5% is injected slowly into the space. If the needle is appropriately located within the PVB space, the administration of local anesthetic will result in a multi-level (2 or more) distribution, with uniform anterior displacement of the pleura (Fig. 3B). If the deposition of local anesthetic is not administered in the TPVB space, the spread is limited to a single level (Fig. 4A, 4B). If a continuous infusion of local anesthetics is desired, a 20-gauge multi-port catheter is introduced through the Tuohy needle and placed 4-5 cm beyond the tip of the needle. For the past 3 years, we have administered lidocaine 0.25% for bilateral continuous TPVBs, and bupivacaine 0.0625% for single continuous TPVB. The infusion rate is initiated at 7 ml/hr per catheter, with a max of 10 ml/hr if desired. A nurse-administered bolus of 3 ml every hour per catheter as needed for breakthrough pain completes the orders.
/webb_3a.jpg?sfvrsn=874a4535_1)
/webb_3b.jpg?sfvrsn=990d3f29_1)
Figure 3. A) Ultrasound scan of the thoracic paravertebral space at the level of T8/T9. Note the needle tip positioned within the paravertebral space. B) deposition of local anesthetic, resulting in uniform, multi-level depression of the pleura; TP=transverse process; LA=local anesthetic; CTL=costo-transverse ligament; P=pleura.
/webb_4a.jpg?sfvrsn=7d87b1bc_1)
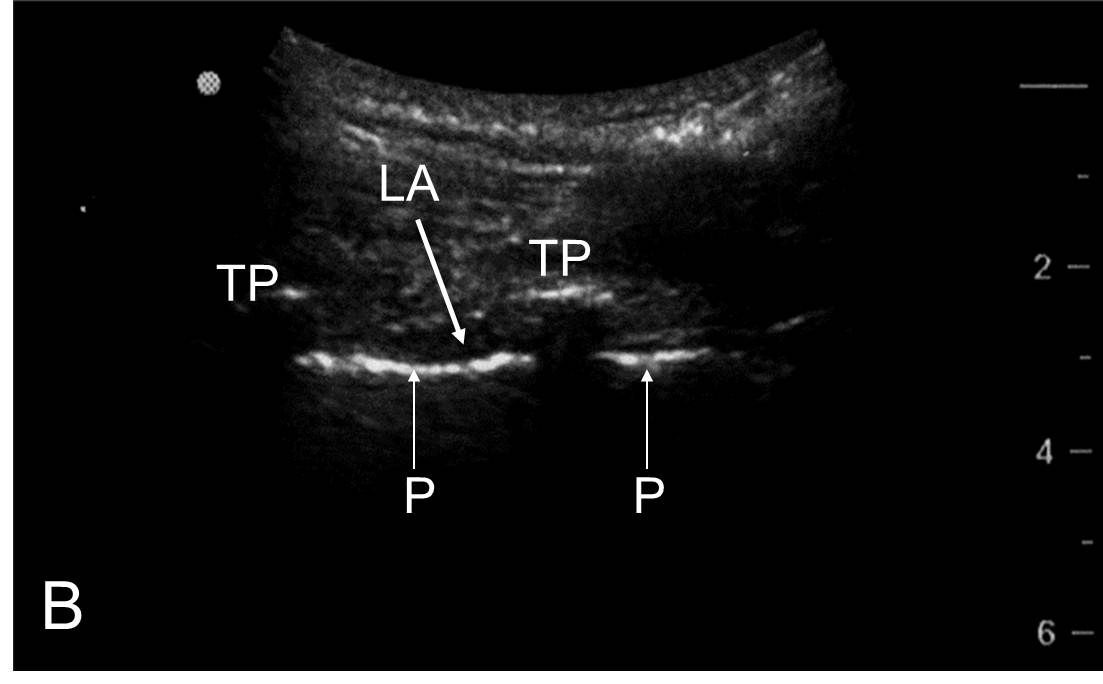
Figure 4. A) Ultrasound scan of the thoracic level T8/T9. B) deposition of local anesthetic, resulting in a single level depression of the pleura, demonstrating an injection outside the paravertebral space; TP=transverse process; LA=local anesthetic; CTL=costo-transverse ligament; P=pleura.
Conclusion
Based upon our experience, we believe the parasagittal in-plane approach minimizes the risk of epidural spread and its associated deleterious systemic effects because needle orientation is perpendicular to the axis of the neural foramen. Therefore, we recommend this as the standard approach when performing ultrasound-guided TPVB.
References
- Conroy, M: How I Do It: Ultrasound-guided Thoracic Paravertebral Blockade. ASRA News 2012;August:14-16.
- Karmakar M. Ultrasound-guided thoracic paravertebral block. Techniques Reg Anes Pain Med 2009;13:142-149.
- Matusic BP, Anthikad F, Ben-David B, Chelly JE. Imaging of Continuous Paravertebral Catheters. Anesthesiology 2006;105:A1147.
- Luyet, C, Eichenberger U, Greif R, Vogt A, Szucs Farkas Z, Moriggl B. Ultrasound-guided paravertebral puncture and placement of catheters in human cadavers: an imaging study. Br J Anaesth. 2009;102:534-539.
- Purcell-Jones G, Pitcher CE, Justins DM. Paravertebral somatic nerve blocks: a clinical radiographic, and computed tomographic study in chronic pain patients. Anesth Analg 1989;68:32-39.
- Lonnqvist PA, MacKenzie J, Soni AK, et al. Paravertebral blockade. Failure rate and complications. Anaesthesia 1995;50:813-815.
- Naja Z and Lonnqvist PA. Somatic Paravertebral Nerve Blockade. Incidence of failed block and complications. Anaesthesia 2001;56:1181-1201
- Chelly JE, Fanelli A. Frequent epidural spread can be prevented when performing an ultrasound guided approach to the paravertebral space. Br J Anaesth 2009 [E-pub June 16, 2009]. http://bja.oxfordjournals.org/content/102/4/534.abstract/href/href/reply#brjana_el_4448
- Fanelli, A, Montoya, M, Ghisi, D. Ultrasound-Guided Thoracic Paravertebral Block: Classic Approach. In: Bigeleisen PE, Orebaugh SL, Moayeri N, Groen GJ, Breneman SM, Chelly JE. Ultrasound-Guided Regional Anesthesia and Pain Medicine: Techniques and Tips. Philadelphia, PA: Lippincott Williams & Wilkins, 2009.
Leave a commentOrder by
Newest on top Oldest on top