How I Do It: Costoclavicular Brachial Plexus Block
Cite as: Sivakumar RK, Karmakar MK. How I do it: costoclavicular brachial plexus block. ASRA News 2021;46. https://doi.org/10.52211/asra110121.069
Costoclavicular brachial plexus block (CCBPB) is a proximal infraclavicular brachial plexus block (ICBPB) technique where local anesthetic (LA) is injected between the cords of the brachial plexus at the costoclavicular space (CCS) (Figure 1 and 2).1–3 The procedure produces ipsilateral sensory-motor blockade of the terminal nerves of the brachial plexus,2,4–7 providing surgical anesthesia or analgesia for upper-extremity surgery.2,4,7–9 CCBPB was first described by Karmakar and colleagues1 as a means to overcome some of the limitations of a lateral sagittal ICBPB.1 This article briefly outlines our current understanding and how we perform a CCBPB.
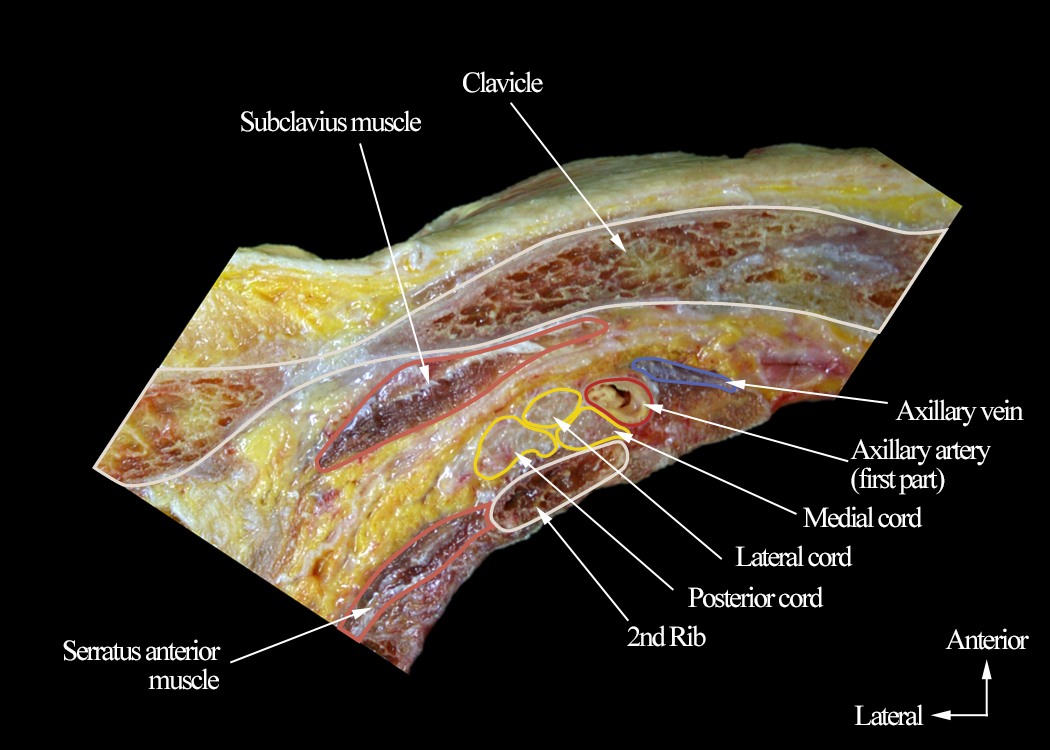
Figure 1. Transverse cadaver anatomic section through the right costoclavicular space showing the arrangement and relations of the cords of the brachial plexus
The anatomy is presented from caudal to cranial (caudocranial view). Note how the three cords of the brachial plexus are clustered together lateral to the axillary artery and lying on top of the second rib.
(Used with permission from the Department of Anesthesia and Intensive Care of the Chinese University of Hong Kong, https://usgraweb.hk.)
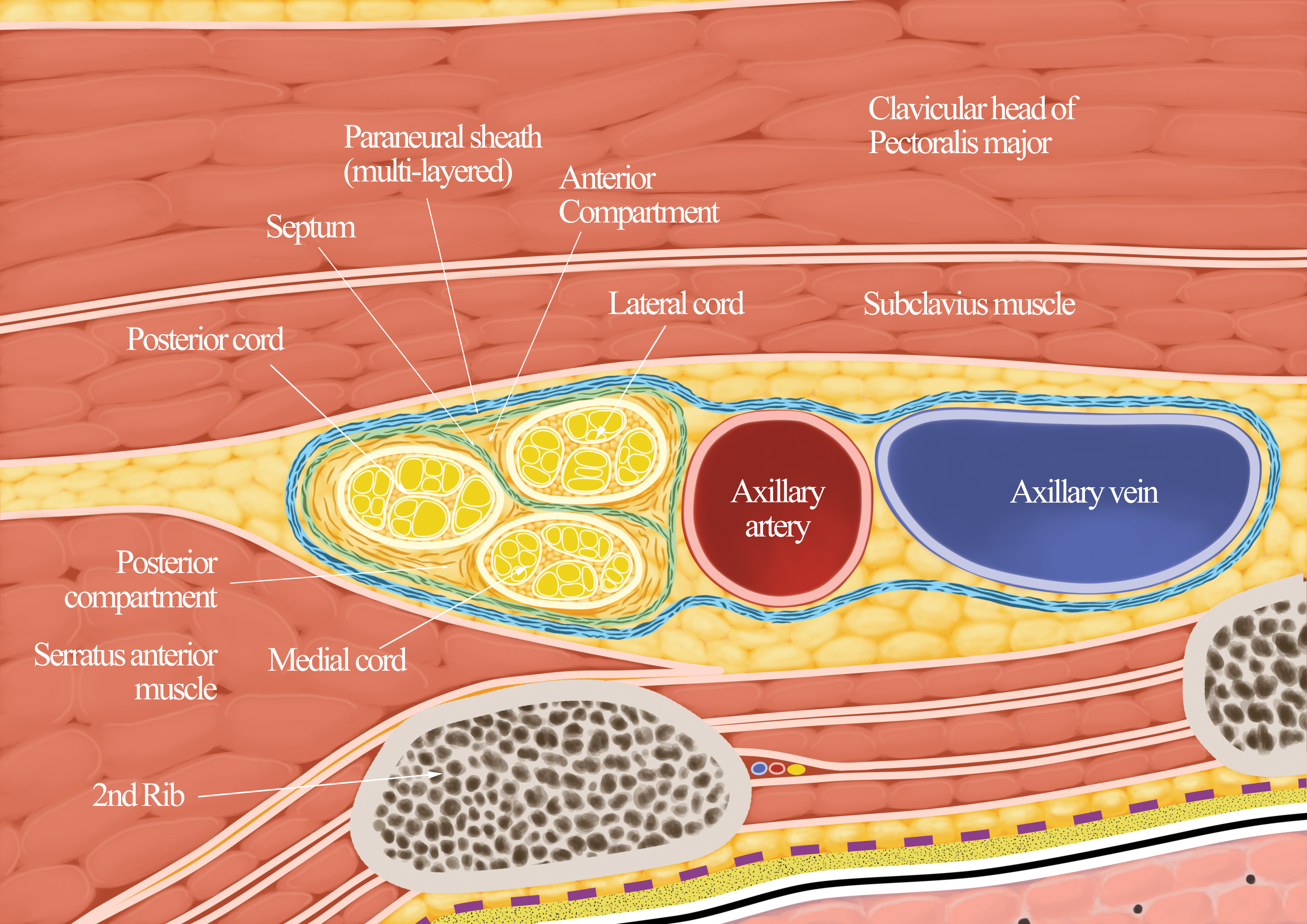
Figure 2. Anatomy of the costoclavicular space showing the cords’ relation to one another and the axillary artery
Note the multilayered paraneural sheath and how it envelopes the neurovascular structures as an all-inclusive neurovascular sheath. Also note the septum of the paraneural sheath and how it divides the subparaneural compartment into an anterior compartment containing the lateral cord and a posterior compartment containing the medial and posterior cords.
(Used with permission from the Department of Anesthesia and Intensive Care of the Chinese University of Hong Kong, https://usgraweb.hk.)
CCBPB Versus Lateral Sagittal ICBPB
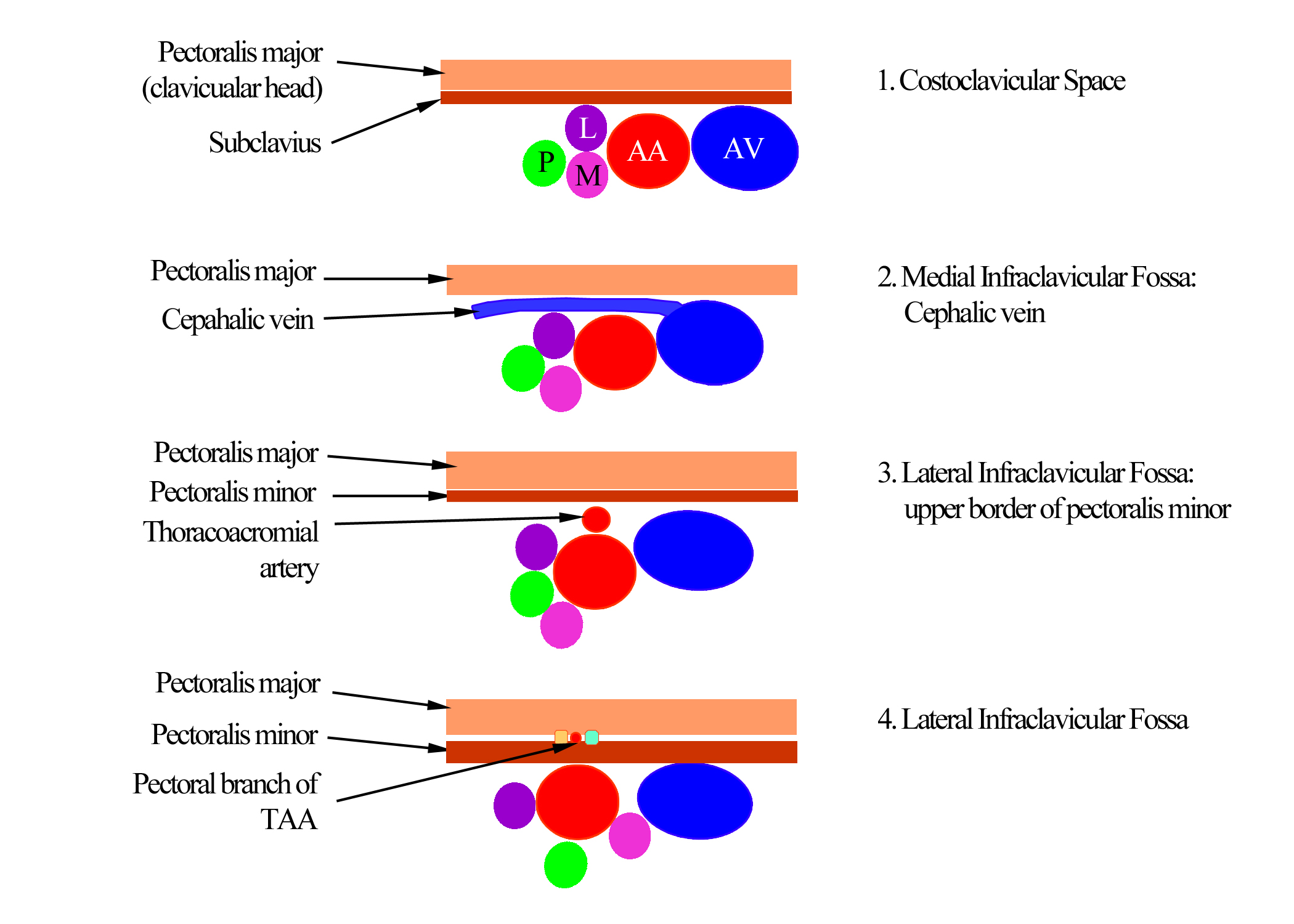
Karmakar and colleagues proposed that the brachial plexus anatomy at the CCS (Figures 1–3) was more suitable for ICBPB than at the lateral infraclavicular fossa (LICF) (Figure 4), despite its history of safety and efficacy.1,10 They based their theory on the understanding that the cords of the brachial plexus at the LICF located deep to the pectoral muscles and at a depth of 3–6 cm11 seem to be separated because they exhibit substantial variation in their position relative to the second part of the axillary artery.12,13 With the position of the arm abducted to approximately 90 degree,14 all three cords are rarely visualized in a single sagittal sonogram during an ultrasound-guided (USG) lateral sagittal ICBPB.13 This may explain why relatively large volumes (35–40 mL) of LA9 or multiple injections15 are frequently successful during a lateral sagittal ICBPB.
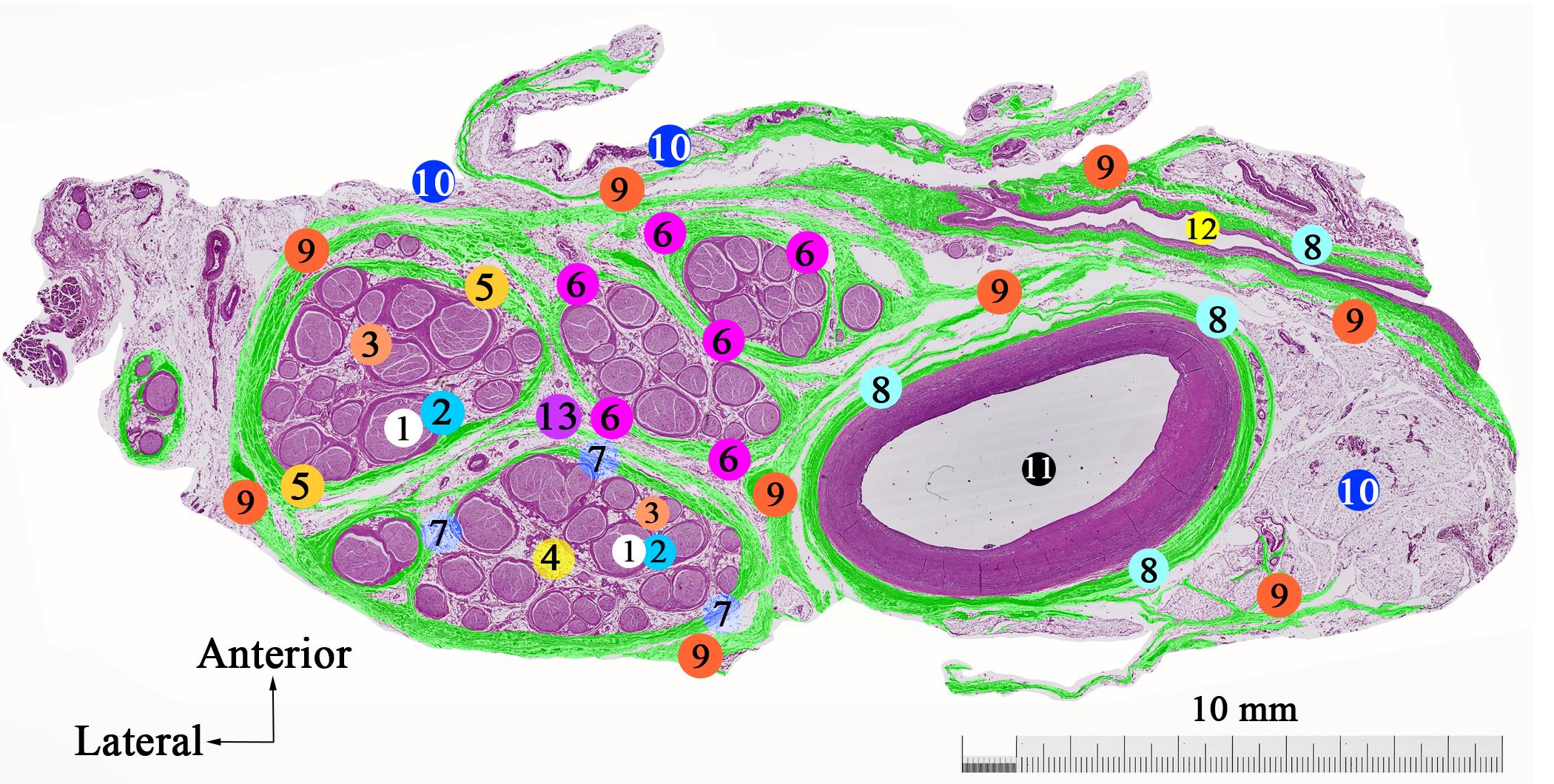
Figure 3. Histological section from the costoclavicular space showing the arrangement of the cords of the brachial plexus and the various fascial layers
After hematoxylin and eosin staining, color was digitally assigned to the various connective tissue elements for clarity. Note that the collagen fibers of the paraneural sheath not only encompass the cords but also the axillary vessels as an all-inclusive neurovascular sheath. Also the septum is well defined. Image is magnified x6.
(1) axons, (2) perineurium, (3) circumfascicular collagen fiber layer, (4) interfascicular connective tissue, (5) epineurium of posterior cord, (6) epineurium of lateral cord, (7) epineurium of medial cord, (8) adventitia of the blood vessel, (9) paraneural sheath, (10) adipocytes, (11) axillary artery, (12) axillary vein, (13) septum
(Used with permission from Dr. Miguel Angel Reina, Madrid, Spain.)
Figure 4. Position and relations of the brachial plexus cords to one another and the axillary artery at the costoclavicular space and medial and lateral infraclavicular fossa
AA, axillary artery; AV, axillary vein; L, lateral; M, medial; P, posterior; TAA, thoracoacromial artery
(Used with permission from the Department of Anesthesia and Intensive Care of the Chinese University of Hong Kong, https://usgraweb.hk.)
The tip of an indwelling catheter placed at the LICF is unlikely to lie close to all the three cords (Figure 4), which may explain why secondary blocks fail with continuous ICBPB.16 In contrast, the cords of the brachial plexus at the CCS are relatively superficial, clustered together lateral to the first part of the axillary artery (Figures 1–4),2–4,17 exhibit a triangular arrangement,17 share a consistent relationship with one another and to the axillary artery (Figures 2–3),3,4,17 and are all visualized in a single transverse sonogram of the medial (proximal) infraclavicular fossa (Figures 5–6).2,4
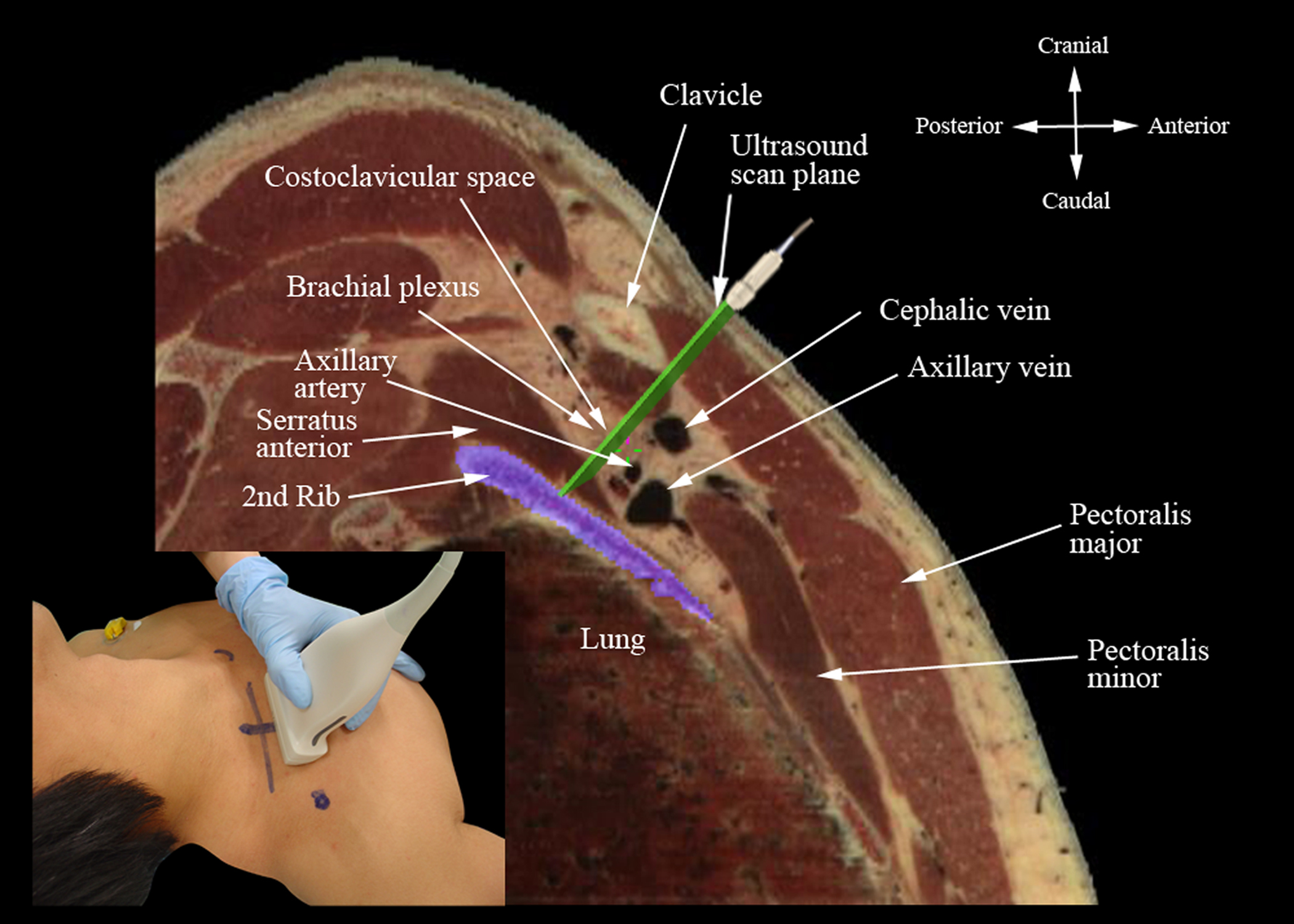
Figure 5. Sagittal anatomic section illustrating the structures imaged during a transverse oblique ultrasound of the costoclavicular space from below the clavicle midsection
The inset image shows the position and orientation of the ultrasound transducer and how it is tilted slightly cephalad
(Anatomical section used with permission from Visible Human Server at Ecole Polytechnique Fédérale de Lausanne, http://visiblehuman.epfl.ch, and Gold Standard Multimedia, www.gsm.org.)
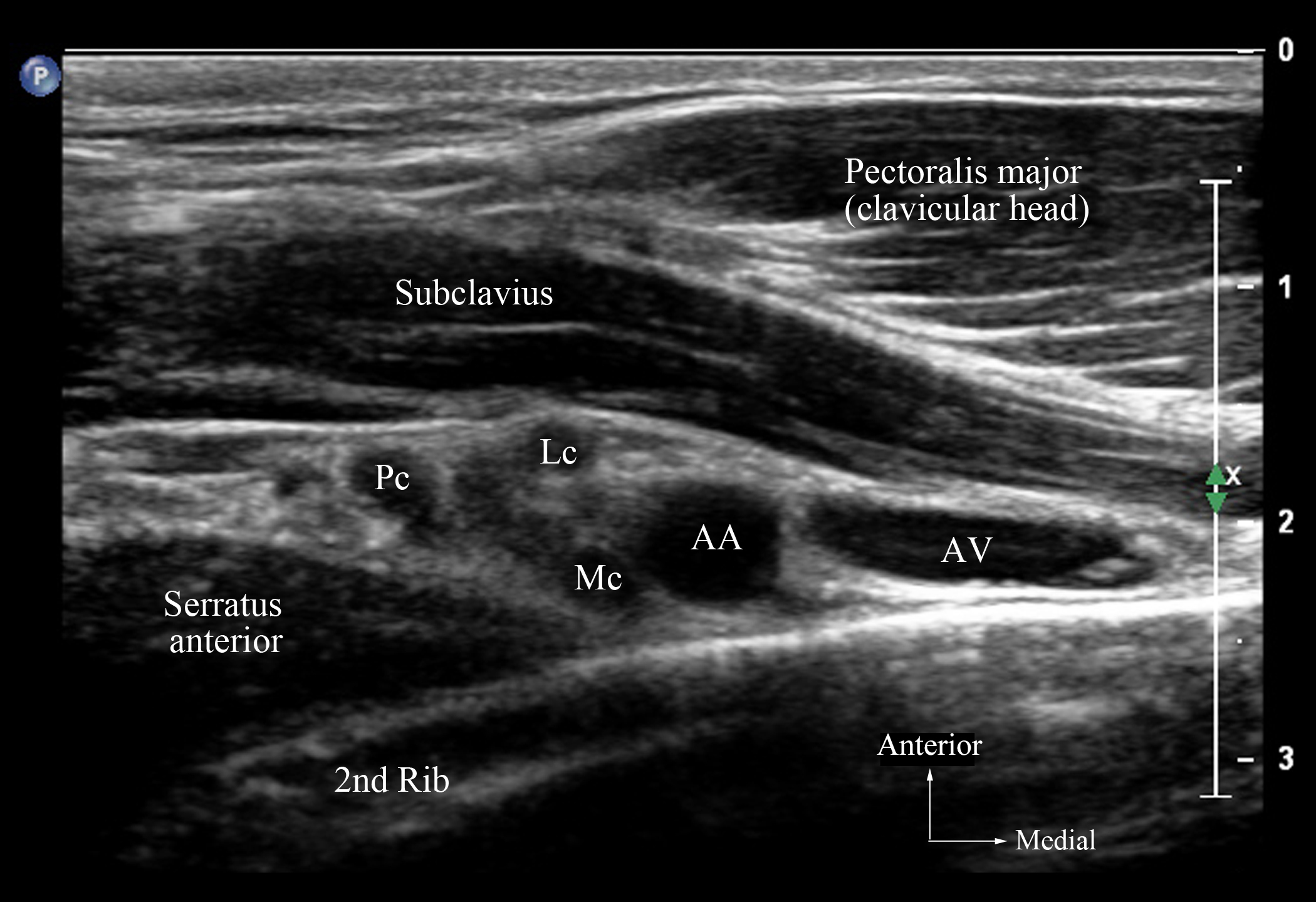
Figure 6. Transverse oblique sonogram of the medial infraclavicular fossa immediately below and posterior to the clavicle midsection demonstrating the brachial plexus cords in the costoclavicular space
Note the relationship of the cords to one another and the axillary artery.
AA, axillary artery; AV, axillary vein; LC, lateral cord; MC, medial cord; PC, posterior cord
Published data also indicate that CCBPB produces an onset of brachial plexus block (BPB)2 4,6–9 faster than a lateral sagittal ICBPB2 and significantly reduces incidence of ipsilateral hemidiaphragmatic paralysis than supraclavicular5 or interscalene18 BPB. Other data show that CCBPB affects the axillary18,19 and suprascapular18,19 nerves and is effective for postoperative analgesia after arthroscopic shoulder surgery.18 Furthermore, a 2020 cadaveric study demonstrated that colored dye injectate after CCBPB spread to the three trunks of the brachial plexus and the suprascapular nerves but not to the phrenic nerve.19 Therefore, CCBPB is emerging as an attractive alternative technique for BPB.
Anatomy
The CCS is an intermuscular space located between the posterior surface of the midsection of the clavicle and the anterior chest wall.3,17,19 It is bound by the clavicular head of the pectoralis major and subclavius muscle anteriorly and the upper slips of the serratus anterior muscle and second rib posteriorly.1,3,4,17 The CCS is part of the axillary tunnel20 and continuous cranially with the supraclavicular fossa and interscalene groove3,19 and caudally with the axilla via the LICF (Figures 1 and 2).3
The cords of the brachial plexus and the axillary vessels traverse the CCS, with the cords lying parallel and lateral to the axillary artery (Figures 1 and 2). The lateral cord is the most superficial of the three and always lies anterior to both the medial and posterior cords. The medial cord is directly posterior to the lateral cord but medial to the posterior cord. The posterior cord is the lateral most of the three cords at the CCS, positioned immediately lateral to the medial cord but posterolateral to the lateral cord. The topography of the cords, relative to the axillary artery and to one another at the CCS, is generally consistent (Figures 1–3).3
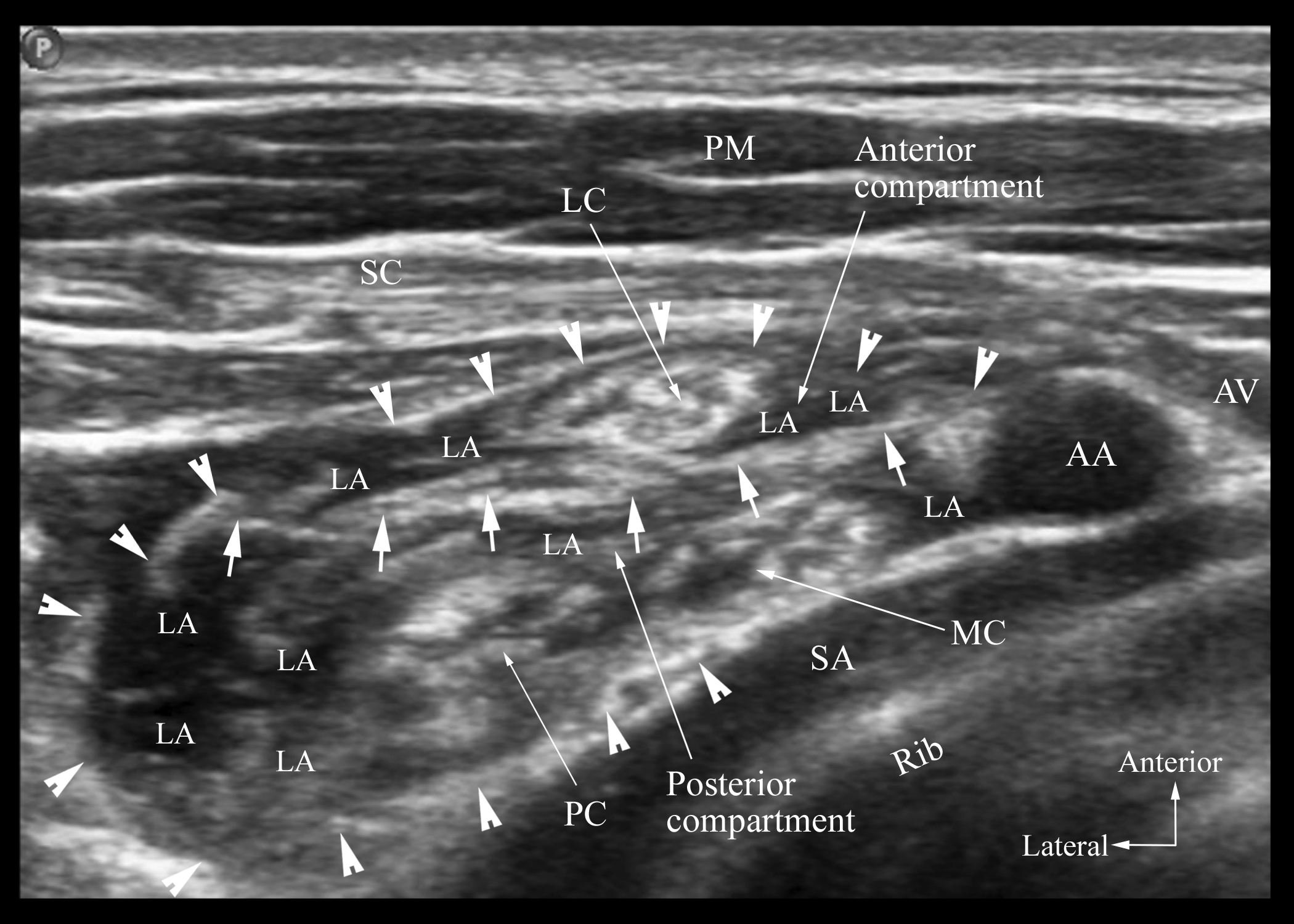
The cords of the brachial plexus at the CCS are also surrounded by a multi-layered interlacing network of collagen fibers (Figure 3),21–23 known as the paraneural sheath,24 analogous to that seen with the sciatic nerve at the popliteal fossa.25 The paraneural sheath is interposed between the epimysium of the surrounding muscles and the epineurium of the cords (Figure 7).24 The paraneural sheath encompasses not only the cords but also the adjacent axillary vessels as an all-inclusive neurovascular sheath (Figure 3).24 It is densely packed around the cords and becomes more loosely arranged as it extends away from the cords (Figure 3).24Furthermore, a connective tissue septum21,24 that extends laterally from the axillary artery21,24 subdivides the subparaneural compartment into an anterior (superficial) compartment containing the lateral cord and a posterior (deep) compartment containing the medial and posterior cords (Figures 2 and 7).24
Figure 7. Transverse oblique sonogram of the brachial plexus just distal to the site of injection at the costoclavicular space and after LA injection
The paraneural sheath (arrow heads) can be seen surrounding the brachial plexus cords. The septum (small white arrows) is an additional hyperechoic layer of connective tissue between the LC anteriorly and the MC and PC posteriorly. It appears to divide the subparaneural compartment into an anterior and a posterior compartment.
AA, axillary artery; AV, axillary vein; LA, local anesthetic, LC, lateral cord; MC, medial cord; PC, posterior cord; PM, pectoralis major; SA, serratus anterior; SC, subclavius
(Used with permission from the Department of Anesthesia and Intensive Care of the Chinese University of Hong Kong, https://usgraweb.hk.)
Ultrasound Scanning Technique
- Position
- Patient: Position the patient supine with the ipsilateral arm abducted (90 degrees) and the head turned slightly to the contralateral side (Figure 8A).
- Operator and ultrasound equipment: For a right-sided block, a right-handed operator stands at the patient’s head and the ultrasound machine is placed on the contralateral side (Figure 8A). The operator’s and ultrasound machine’s positions are changed for a left-sided block.
- Transducer selection: High-frequency linear array transducer (12–15 MHz)
- Scan technique: Position the transducer directly over the clavicle midsection in the transverse orientation. Gently move it caudally until it slips off the clavicle’s inferior border and the axillary artery (first part) and vein are visualized (Figure 6). It may be necessary to gently tilt the transducer cephalad to direct the ultrasound beam toward the CCS (Figure 8B). Optimize the ultrasound image until all three cords of the brachial plexus are clearly visualized lateral to the axillary artery (Figure 6). If the cords’ visibility is less than optimal, gently pivot the medial end of the transducer caudally to try and direct the ultrasound beam at right angles to the cords.
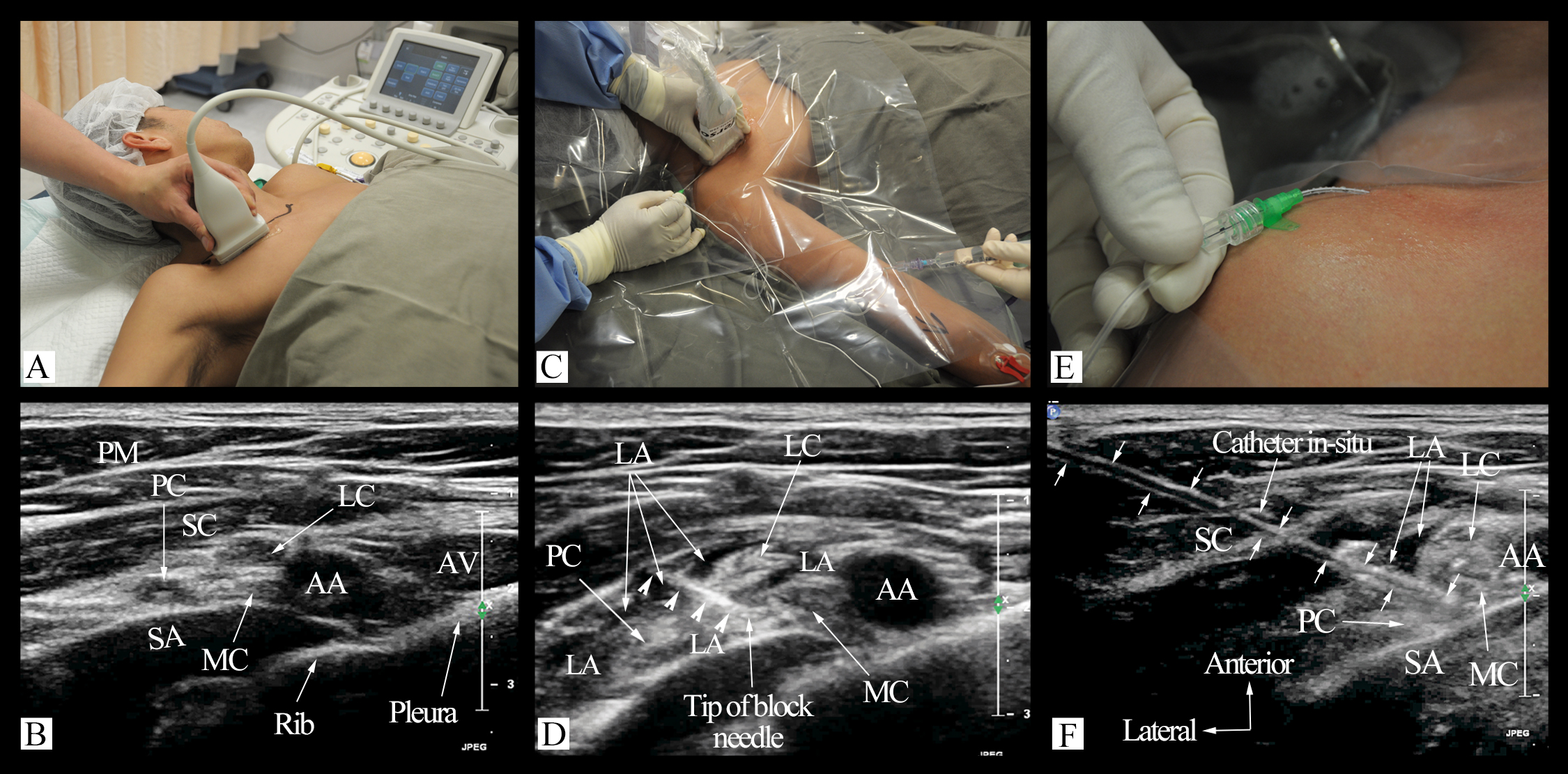
Figure 8. Ultrasound-guided catheter placement for continuous costoclavicular brachial plexus block
(A) patient position and orientation of the ultrasound transducer (linear, 12–15 MHz), (B) transverse sonogram demonstrating all three cords of the brachial plexus in the costoclavicular space, (C) the block needle (catheter-over-needle) inserted in plane and from a lateral to medial direction, (D) the tip of the needle positioned at the center of the cord and nerve cluster before the LA bolus is injected at a single site, (E) an indwelling catheter assembly positioned in the costoclavicular space, (F) transverse oblique sonogram showing the indwelling catheter with its tip close to all the three cords
AA, axillary artery; AV, axillary vein; LA, local anesthetic; LC, lateral cord; MC, medial cord; PC, posterior cord; PM, clavicular head of pectoralis major muscle; SA, serratus anterior muscle; SC, subclavius muscle
(Used with permission from the Department of Anesthesia and Intensive Care of the Chinese University of Hong Kong, https://usgraweb.hk.)
Sonoanatomy
During a transverse ultrasound of the upper medial infraclavicular fossa immediately below the clavicle midsection, the CCS1,4 is visualized as an intermuscular space between the pectoralis major’s clavicular head, the subclavius muscle anteriorly, and the serratus anterior muscle overlying the second rib. The axillary artery (first part) and the axillary vein appear as two hypoechoic, round-to-oval structures in the CCS. The axillary artery is pulsatile and located lateral to the axillary vein. Deep to the axillary artery, the upper slips of the serratus anterior muscle, second rib, intercostal muscles, and parietal pleura are visualized. The three cords of the brachial plexus are clustered together lateral to the axillary artery in a consistent triangular topographical arrangement (Figure 6).1,4
Immediately distal to the CCS, the cephalic vein can be seen arching over the cords, from a lateral to medial direction, to join the axillary vein. Therefore, if the cephalic vein is visualized in the transverse sonogram it usually indicates that the ultrasound scan is being performed distal to the CCS and requires manipulation of the transducer cranially. For the same reason it is also imperative to visualize the subclavius muscle in the target ultrasound window as without it the scan is distal to the CCS.4
Sonographically, the paraneural sheath is visualized as a hyperechoeic layer of connective tissue between the epineurium of the cords and the epimysium of the surrounding muscles and most visible after LA injection. The septum extends laterally from the axillary artery as an additional hyperechoic layer of connective tissue in the paraneural sheath that subdivides the subparaneural compartment into an anterior compartment containing the lateral cord and a posterior compartment containing the posterior and medial cords (Figure 7).24
Needling Technique
CCBPB is performed with the patient supine and the arm abducted to elevate the clavicle and extend the space below its midsection, facilitating transducer placement and in-plane needle insertion lateral to the transducer (Figure 8A).4 If the patient is unable to abduct their ipsilateral arm, CCBPB can be performed using a medial approach.26
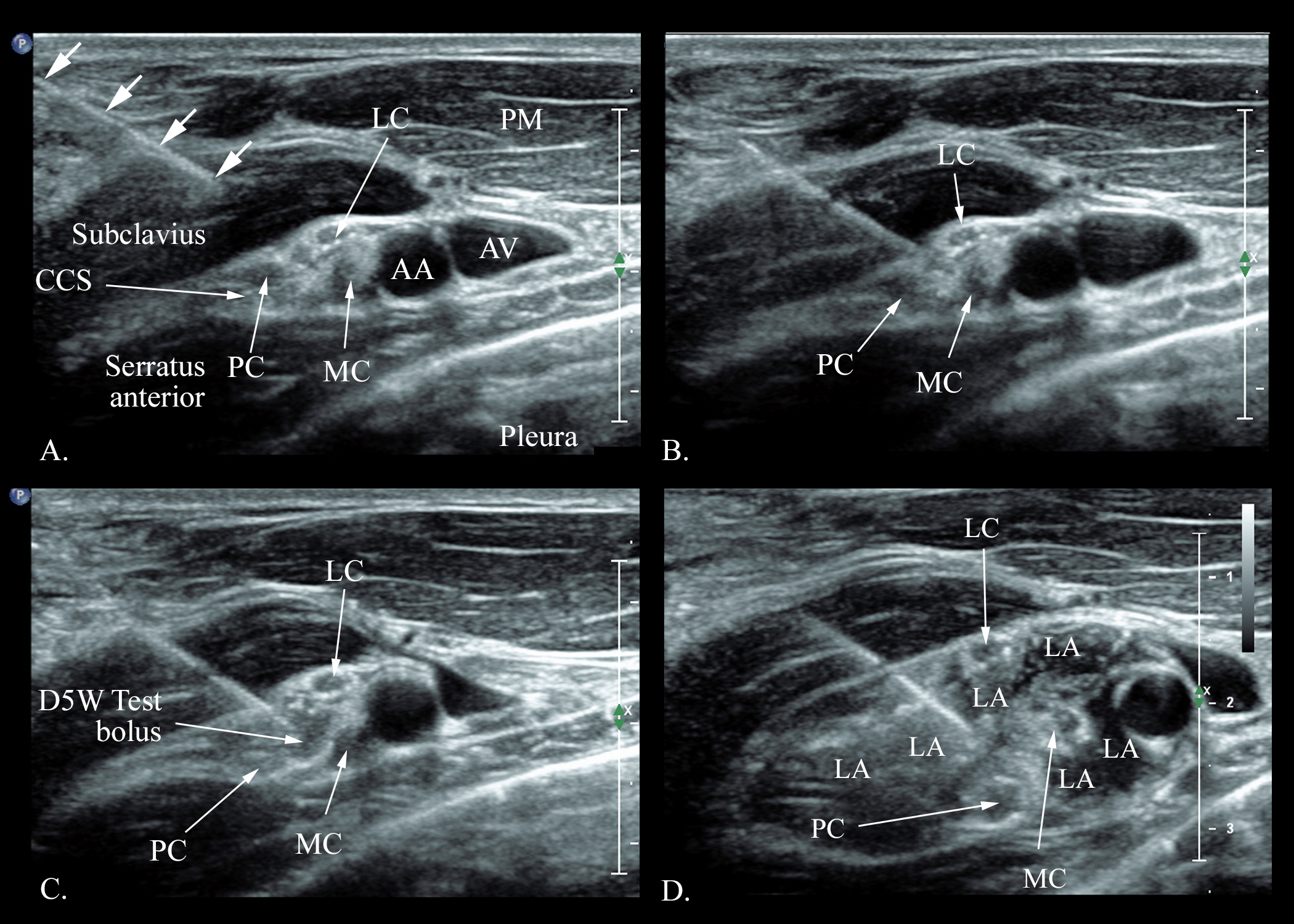
For the traditional lateral approach, once the target transverse ultrasound window (Figure 6) is acquired, the block needle is inserted under strict aseptic precautions, in-plane from a lateral to medial direction (Figure 8C). By advancing the needle tip through the gap between the lateral and posterior cords and placing it close to the medial cord, the needle tip is positioned at the center of the cords in the CCS (Figure 9).1,2,4 Then, 1–2 m of normal saline or 5% dextrose (if using nerve stimulation) is injected as a test bolus (Figure 9C). Correct needle tip position is confirmed by (a) visualization of the needle tip between the cords within the CCS (Figure 9C)4 and (b) spread of a test bolus injection (anechoic fluid) between, but not within the cords, without any obvious swelling of the brachial plexus cords (Figure 9C).4 Once successfully placed, the total LA dose (25 mL) is slowly injected in small aliquots at a single site without any needle redirection (Figure 9D).
Figure 9. Transverse oblique sonograms illustrating single-injection costoclavicular brachial plexus block
(A) in-plane needle insertion from a lateral to medial direction (lateral approach), (B) the needle tip advanced through the gap between the lateral and posterior cords of the brachial plexus, (C) a test bolus (1–2 ml) of normal saline or 5% dextrose to confirm correct needle tip position before the LA is injected, (D) sonogram acquired after completion of the LA injection (20 ml in this case)
AA, axillary artery; AV, axillary vein; CCS, costoclavicular space; LA, local anesthetic; LC, lateral cord; MC, medial cord; PC, posterior cord; PM, clavicular head of pectoralis major muscle
(Used with permission from the Department of Anesthesia and Intensive Care of the Chinese University of Hong Kong, https://usgraweb.hk.)
Drug and Dosage
Currently, data on the optimal volume of LA required for USG CCBPB is sparse. Our research group has demonstrated that 21 mL (95% confidence interval [CI] = 20.7–21.8 mL) is the minimum effective volume (MEV90) of 0.5% ropivacaine in 90% of patients for USG CCBPB.7 This is in agreement with the ED95 of 0.5% ropivacaine, 18.9 mL (95% CI = 17.9–27.5 mL), reported by Kewlani et al. for USG CCBPB.27 However, and in contrast to that evidence, Sotthisopha et al.6 reported that the MEV90 of lidocaine 1.5% with 5 mcg/mL epinephrine is 34 mL (95% CI = 33.4–34.4 mL).6 The variation may be related to differences in study methodology, drugs used, and criteria for the definition of block success.6,7,27 In our clinical practice, we rarely use more than 25 mL of LA for CCBPB and it consistently produces rapid onset of surgical anesthesia of the upper extremity.1,2,4
Single- or Multiple-Injection CCBPB
Data are also currently limited on the optimal technique for CCBPB (ie, whether to perform a single injection or multiple injections targeting the individual cords). Research has also not demonstrated whether the multicompartmented paraneural sheath at the CCS24 affects LA spread and block dynamics after CCBPB. That said, the original method of injecting the LA between the cords of the brachial plexus,1,2,4 which is inherently a subparaneural injection,24 produces rapid onset of ipsilateral brachial plexus blockade.2,4,9
Layera et al.28 performed a double-injection CCBPB, using 35 mL of 1% lidocaine and 0.25% bupivacaine with epinephrine and dexamethasone, and demonstrated that it produces faster onset of surgical anesthesia (onset time = 16.6 min vs 23.4 min; 95% CI = 3.3–9.7 min) than its single-injection counterpart.28 Lee and colleagues29 also demonstrated that a triple-injection CCBPB, targeting the individual cords using a mixture of 10 mL of 2% lidocaine, 10 mL of 0.75% ropivacaine, and 5 mL of normal saline (total volume = 25 mL), produces a higher rate of sensory-motor blockade of all four terminal nerves of the brachial plexus at 30 minutes than single-injection CCBPB (85.3% vs 52.9%).29 The limited available evidence suggests that a multiple-injection CCBPB targeting the individual cords may be more successful;28,29 however, given the paucity of data and our current understanding of a multicompartmented paraneural sheath at the CCS, future research should determine whether two injections into the anterior and posterior compartments produces improved block dynamics than a single injection between the cords or a triple injection targeting individual cords.
Continuous CCBPB
A catheter placed at the center of the CSS cord and nerve cluster (Figure 8) is not only subfascial but also in close proximity to all the three cords of the brachial plexus (Figure 8D).1,24 The intermuscular CCS1,3,4 may also help secure a catheter in situ and reduce the risk of accidental dislodgement, commonly seen with supraclavicular catheters. Current published data on continuous CCBPB are limited, but it is our clinical experience that an infusion of 4–6 mL/h of a low-concentration LA, like 0.125% levobupivacaine, is usually adequate for extended analgesia in the postoperative setting.
Indications, Contraindications, and Complications
CCBPB targets the cords of the brachial plexus and blocks all five terminal nerves: axillary, musculocutaneous, radial, ulnar, and median. Thereby, it provides excellent anesthesia and analgesia for upper-extremity surgery below the mid arm.4 Published data also suggest that CCBPB affects the suprascapular nerve.18,19 Because CCBPB affects the axillary (posterior cord),18,19 upper subscapular (posterior cord), and lateral pectoral (lateral cord) nerves, it is effective in providing postoperative analgesia, noninferior to an interscalene BPB,18 after arthroscopic shoulder surgery. In this context, the significantly lower incidence of ipsilateral hemidiaphragmatic paralysis with CCBPB (0%–5%)5,18 compared to interscalene BPB (100%)18 is encouraging. Future research should establish CCBPB’s role in shoulder surgery and whether it provides surgical anesthesia of the entire ipsilateral upper extremity except for the area innervated by the intercostobrachial nerve (T2), like a selective trunk block.30,31
Additionally, it has no specific absolute contraindications. Relative contraindications include previous surgery over the medial infraclavicular fossa and the presence of aberrant vascular anatomy in the cord cluster.32 We consider coagulopathy and anticoagulant medications a contraindication for CCBPB because the CCS is not easily compressible and BPB has safer alternatives. Data on the safety and complications after a CCBPB are lacking; however, because the cords of the brachial plexus at the CCS are closely related to the axillary artery, parietal pleura and the apex of the lung, accidental vascular puncture, LA systemic toxicity, and pleural puncture are possible complications.
Conclusion
CCBPB is a proximal infraclavicular BPB technique that targets the cords of the brachial plexus at the CCS. Sensory-motor blockade after a CCBPB is rapid in onset and significantly faster than a lateral sagittal ICBPB. It provides effective anesthesia and or analgesia for ipsilateral upper-extremity surgery below the mid arm, but growing evidence suggests that it is also effective for postoperative analgesia after arthroscopic shoulder surgery. CCBPB produces significantly lower incidence of ipsilateral hemidiaphragmatic paresis than the supraclavicular or interscalene approach. Continuous CCBPB using low volumes of LA via a catheter placed at the CCS is a viable option and warrants future research.
This work was locally funded by the Department of Anaesthesia and Intensive Care, Faculty of Medicine, Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, New Territories, Hong Kong, SAR, China.
Ranjith Kumar Sivakumar, MD, is a regional anesthesia fellow in the department of Anesthesia and Intensive Care at the Chinese University of Hong Kong and Prince of Wales Hospital in Shatin, Hong Kong, China.

Manoj Kumar Karmakar, MD, FRCA, is a professor and consultant anesthesiologist in the department of Anesthesia and Intensive Care at the Chinese University of Hong Kong and Prince of Wales Hospital in Shatin, Hong Kong, China.
References
- Karmakar MK, Sala-Blanch X, Songthamwat B, et al. Benefits of the costoclavicular space for ultrasound-guided infraclavicular brachial plexus block: description of a costoclavicular approach. Reg Anesth Pain Med 2015;40(3):287–8. https://doi.org/10.1097/aap.0000000000000232
- Songthamwat B, Karmakar MK, Li JW, et al. Ultrasound-guided infraclavicular brachial plexus block prospective randomized comparison of the lateral sagittal and costoclavicular approach. Reg Anesth Pain Med 2018;43(8):825–31. https://doi.org/10.1097/aap.0000000000000822
- Sala-Blanch X, Reina MA, Pangthipampai P, et al. Anatomic basis for brachial plexus block at the costoclavicular space: a cadaver anatomic study. Reg Anesth Pain Med 2016;41(3):387–91. https://doi.org/10.1097/aap.0000000000000393
- Li JW, Songthamwat B, Samy W, et al. Ultrasound-guided costoclavicular brachial plexus block sonoanatomy, technique, and block dynamics. Reg Anesth Pain Med 2017;42(2):233–40. https://doi.org/10.1097/aap.0000000000000566
- Sivashanmugam T, Maurya I, Kumar N, et al. Ipsilateral hemidiaphragmatic paresis after a supraclavicular and costoclavicular brachial plexus block: a randomised observer blinded study. Eur J Anaesthesiol 2019;36(10):787–95. https://doi.org/10.1097/eja.0000000000001069
- Sotthisopha T, Elgueta MF, Samerchua A, et al. Minimum effective volume of lidocaine for ultrasound-guided costoclavicular block. Reg Anesth Pain Med 2017;42(2):571–4. https://doi.org/10.1097/aap.0b013e31820d4266
- Wong MH, Karmakar MK, Mok LYH, et al. Minimum effective volume of 0.5% ropivacaine for ultrasound-guided costoclavicular brachial plexus block: a dose finding study. Eur J Anaesthesiol 2020;37(9):780–6. https://doi.org/10.1097/eja.0000000000001287
- Leurcharusmee P, Elgueta MF, Tiyaprasertkul W, et al. A randomized comparison between costoclavicular and paracoracoid ultrasound-guided infraclavicular block for upper limb surgery. Can J Anesth 2017;64(6):617–25. https://doi.org/10.1007/s12630-017-0842-z
- Tran DQH, Dugani S, Dyachenko A, et al. Minimum effective volume of lidocaine for ultrasound-guided infraclavicular block. Reg Anesth Pain Med 2011;36(5):190–4. https://doi.org/10.1097/aap.0b013e3182289f59
- Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth 2002;89(2):254–9. https://doi.org/10.1093/bja/aef186
- Bigeleisen P, Wilson M. A comparison of two techniques for ultrasound-guided infraclavicular block. Br J Anaesth 2006;96(4):502–7. https://doi.org/10.1093/bja/ael024
- Sauter AR, Smith HJ, Stubhaug A, et al. Use of magnetic resonance imaging to define the anatomical location closest to all three cords of the infraclavicular brachial plexus. Anesth Analg 2006;103(6):1574–6. https://doi.org/10.1213/01.ane.0000242529.96675.fd
- Di Filippo A, Orando S, Luna A, et al. Ultrasound identification of nerve cords in the infraclavicular fossa: a clinical study. Minerva Anestesiol 2012;78(4):450–5 https://pubmed.ncbi.nlm.nih.gov/22240617
- Ruiz A, Sala X, Bargallo X, Hurtado P, et al. The influence of arm abduction on the anatomic relations of infraclavicular brachial plexus: an ultrasound study. Anesth Analg 2009;108(1):364–6. https://doi.org/10.1213/ane.0b013e31818c94da
- Gaertner E, Estebe JP, Zamfir A, et al. Infraclavicular plexus block: multiple injection versus single injection. Reg Anesth Pain Med 2002;27(6):590–4. https://doi.org/10.1053/rapm.2002.36456
- Ahsan ZS, Carvalho B, Yao J. Incidence of failure of continuous peripheral nerve catheters for postoperative analgesia in upper extremity surgery. J Hand Surg Am 2014;39(2):324–9. https://doi.org/10.1016/j.jhsa.2013.11.011
- Demondion X, Herbinet P, Boutry N, et al. Sonographic mapping of the normal brachial plexus. AJNR Am J Neuroradiol 2003(7):1303–9. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc7973677
- Aliste J, Bravo D, Layera S, et al. Randomized comparison between interscalene and costoclavicular blocks for arthroscopic shoulder surgery. Reg Anesth Pain Med 2019;44:472–7. https://doi.org/10.1136/rapm-2018-100055
- Koyyalamudi V, Langley NR, Harbell MW, et al. Evaluating the spread of costoclavicular brachial plexus block: an anatomical study. Reg Anesth Pain Med 2020;46(1):31–4. https://doi.org/10.1136/rapm-2020-101585
- Cornish PB, Leaper CJ, Hahn JL. The "axillary tunnel": an anatomic reappraisal of the limits and dynamics of spread during brachial plexus blockade. Anesth Analg 2007;104(5):1288–91. https://doi.org/10.1213/01.ane.0000260322.67439.b5
- Monzo E, Boezaart AP, Tubbs RS, et al. A reliable septum exists between the lateral cord and medial and posterior cords in the costoclavicular region. Clinical and microanatomical considerations in brachial plexus anesthetic blockade. Clin Anat 2021;34(3):411–9. https://doi.org/10.1002/ca.23665
- Reina MA, Boezaart AP, Tubbs RS, et al. Another (internal) epineurium: beyond the anatomical barriers of nerves. Clin Anat 2020;33(2):199–206. https://doi.org/10.1002/ca.23442
- Reina MAS-B X, Arriazu R, Machés, F. Microscopic morphology and ultrastructure of human peripheral nerves. In: Tubbs RS, Rizk E, Shoja M, et al. eds. Nerves and nerve injuries. 1st ed. London: Elsevier, 2015.
- Areeruk P, Karmakar MK, Reina MA, et al. High-definition ultrasound imaging defines the paraneural sheath and fascial compartments surrounding the cords of the brachial plexus at the costoclavicular space and lateral infraclavicular fossa. Reg Anesth Pain Med 2021;46(6):500–6. https://doi.org/10.1136/rapm-2020-102304
- Karmakar MK, Shariat AN, Pangthipampai P, et al. High-definition ultrasound imaging defines the paraneural sheath and the fascial compartments surrounding the sciatic nerve at the popliteal fossa. Reg Anesth Pain Med 2013;38(5):447–51. https://doi.org/10.1097/aap.0b013e31829ffcb4
- Nieuwveld D, Mojica V, Herrera AE, et al. Medial approach of ultrasound-guided costoclavicular plexus block and its effects on regional perfusion. Rev Esp Anestesiol Reanim 2017;64(4):198–205. https://doi.org/10.1016/j.redar.2016.09.010
- Kewlani A, Bhatia N, Makkar JK, et al. Median effective volume of 0.5% ropivacaine for ultrasound-guided costoclavicular block. Anesthesiology. 2021;134():617–25. https://doi.org/10.1097/aln.0000000000003731
- Layera S, Aliste J, Bravo D, et al. Single- versus double-injection costoclavicular block: a randomized comparison. Reg Anesth Pain Med 2020;45(3):209–13. https://doi.org/10.1136/rapm-2019-101167
- Lee MG, Jung WS, Go DY, et al. Efficacy of a single injection compared with triple injections using a costoclavicular approach for infraclavicular brachial plexus block during forearm and hand surgery: a randomized controlled trial. Medicine (Baltimore). 2020;99(43):e22739. https://doi.org/10.1097/md.0000000000022739
- Karmakar MK, Areeruk P, Mok LYH, et al. Ultrasound-guided selective trunk block to produce surgical anesthesia of the whole upper extremity: case report. A A Pract 2020;14(9):e01274. https://doi.org/10.1213/xaa.0000000000001274
- Sivakumar RK, Areeruk P, Karmakar MK. Selective trunk block (setb): a simple alternative to hybrid brachial plexus block techniques for proximal humeral fracture surgery during the COVID-19 pandemic. Reg Anesth Pain Med 2020;46(4):376–8. https://doi.org/10.1136/rapm-2020-101733
- Areeruk P, Sivakumar RK, Karmakar MK. Brachial plexus blockade with anomalous location of the t1 ventral ramus at the supraclavicular fossa. Br J Anaesth 2020;125(5):e412–4. https://doi.org/10.1016/j.bja.2020.07.023
Leave a commentOrder by
Newest on top Oldest on top