Motivational Interviewing and Brief Action Planning to Promote Health Behavior Change
Cite as: Beckman N. Motivational interviewing and brief action planning to promote health behavior change. ASRA Pain Medicine News 2022;47. https://doi.org/10.52211/asra050122.020
Providers ask patients to make many behavior changes: start or stop taking this medication, get more exercise, follow up with this referral, and the list goes on. But what do you do when patients return, often in the same or worse condition, and have not followed through with the recommendations? Providers often try harder and harder to convince patients, but sometimes nothing seems to work. This is a common scenario. It is estimated that up to half of patients don’t adhere to medical recommendations, leading to poorer clinical outcomes and greater patient and provider frustration,1 but can anything be done about it?
Motivational Interviewing
Years of research on motivational interviewing (MI) has shown that how we talk to our patients can influence their level of motivation.2 MI is a collaborative communication style that recognizes that behavior change is hard, ambivalence is a normal state, and arguing for change with a person who is ambivalent will naturally bring out their counter arguments.2,3 MI posits that motivation occurs when people perceive a discrepancy between where they are and where they want to be, and that they are most persuaded by what they hear themselves say.3 MI labels the “yes, but…” as a clear sign of ambivalence, and discourages repeating the argument or trying harder to convince the patient. Instead, MI guides providers to step back and ask the patient an open-ended question, learn what the patient is thinking, listen for their reasons for wanting to change and for the barriers that stop them, and to reflect those back.2,3 When providers express a desire to really understand and “roll with resistance” in this way, patients tend to be more receptive to information.2 Ample research has shown that MI is effective in promoting health behavior change across conditions and populations and when delivered by providers of many different disciplines (Table 1).2-4
Table 1: The Principles of Motivational Interviewing
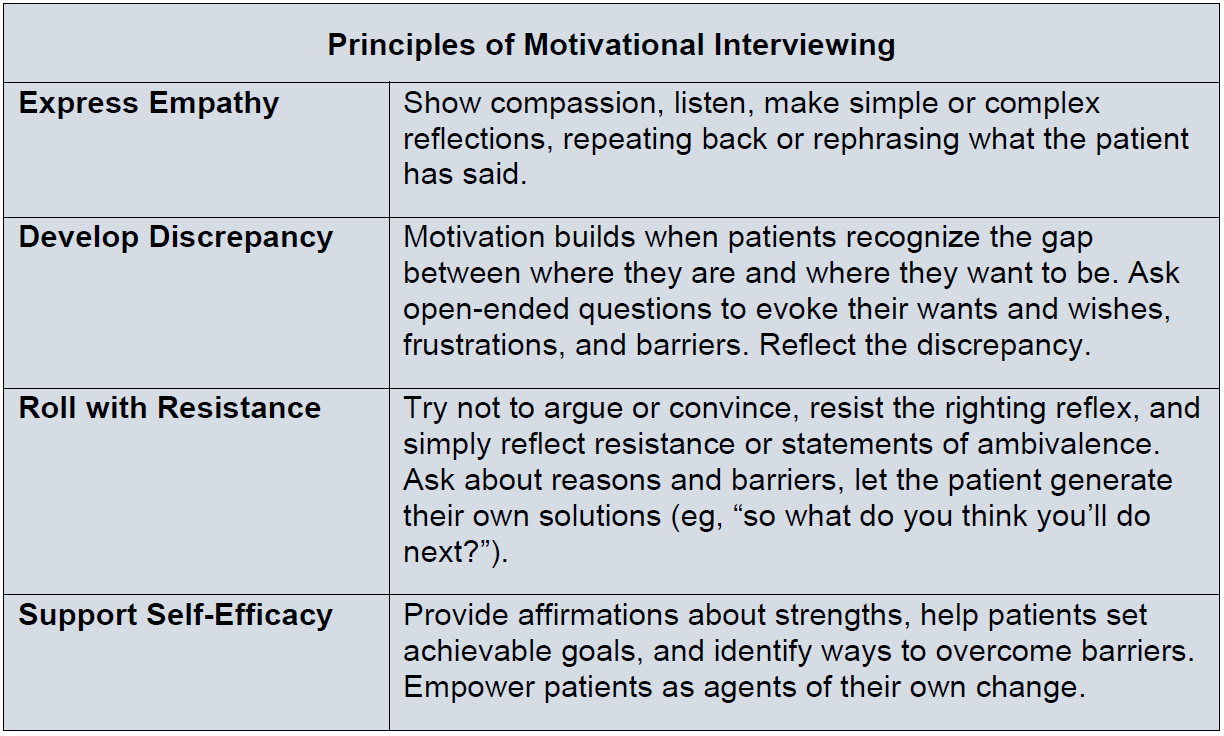
Based on information from Miller WR and Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. Guilford Press; 2012.
The Stages of Change
Asking what patients think about a particular behavior also provides information to help gauge a patient’s level of readiness for change. The Stages of Change Model is useful to consider when using an MI approach because it recognizes the many steps on the road to successful behavior change.5 Considering where a patient is in this model can prevent a lot of frustration as providers now target their interventions to meet their patients at their current level of motivation, information, and skill. The provider’s tasks may differ depending on where a patient is in this model. For example, providing information could move a patient from precontemplation to contemplation. Though the provider might not have seen any tangible action, this is a vital step on the road to change, especially when thinking about patient-provider relationships in the long-run (Figure 1).
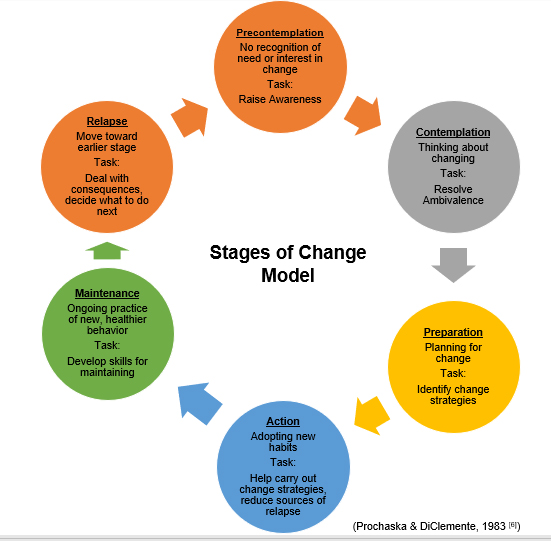
This model describes the six stages people can pass through on their way to make an intentional behavior change. It recognizes that people change when they are ready to do so and that effective interventions meet people at their current state of readiness for change.
Based on information from Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 1983; 51(3):390-5.
The Spirit of Motivational Interviewing
One of the ways to start incorporating an MI style is to adopt the Spirit of MI, which consists of collaboration, evocation, and autonomy.2,3 Acting in the spirit of collaboration means recognizing that the patient is truly the expert of their own lives. A collaborative partnership might include more shared agenda setting: asking patients “What would you like to work on today?”; asking permission: “Is it okay if we also about how things are going with your stress at home?”; and providing information in an ask-tell-ask style instead of a chunk-check-chunk style: “What do you know about the risks of using opioids over a long period of time?“ (patient responds) “Right, there are also risks of… What do you think about those?”.7
Next, the MI spirit of evocation means drawing out the patient’s thoughts and ideas instead of trying to convince them to adopt your opinions. Of course, in healthcare settings, providers are an important source of information and patients ask for their opinion. MI warns of falling into an expert trap and to instead provide options. For example, “Here are some things that other patients in your situation have done…do any of those options seem like they might work for you?” 2 It is important to deliver information in a concise, understandable way, to regularly pause, and to ask an open-ended question to evoke the patient’s thoughts about the information and to check for their understanding.
The last element of the spirit includes respecting a patient’s autonomy. Providers do not have to agree with or lie to their patients, but if providers can accept that patients are not ready to change, they might offer the option of not doing anything or slowing down. In MI, this is the paradox of change, “when people feel accepted for who they are and what they do—no matter how unhealthy—it allows them the freedom to consider change rather than needing to defend against it”.3
Brief Action Planning
Before wrapping up a visit, a last step is to guide the patient toward an action plan. A simple way to do this is through Brief Action Planning (BAP), which is a highly structured, self-management support strategy based on the principles of MI and action planning.8 BAP is designed to be easy to use with patient-centered language and open-ended questions that reflect the MI spirit of respect for autonomy, evocation, and collaboration by having patients choose their next step and leaving space for the provider to respectfully share their expert guidance (Figure 2).
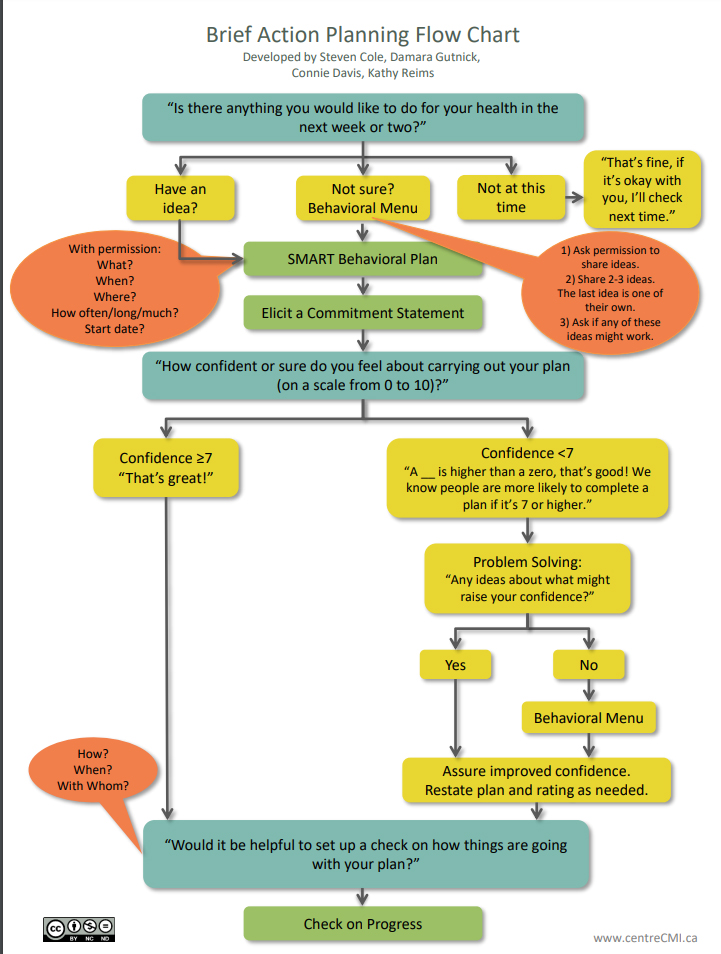
Figure 2: Brief Action Planning Flow Chart
Brief action planning incorporates motivational interviewing in a simple framework that providers can use to guide people toward behavior change.
From Gutnick D, Reims K, Davis C, et al. Brief action planning to facilitate behavior change and support patient self-management. JCOM 2014;21(1):17-29. Used with permission.
As outlined in the flow chart, BAP asks patients three main questions. (A detailed explanation of how to implement BAP can be found in Gutnik et al. 20148 as well as resources for its use on the CCMI website https://centrecmi.ca/brief-action-planning/.9) As illustrated, a provider begins by asking, “Is there anything you would like to do for your health in the next week or two?” Some patients will say no, and, in the spirit of MI, providers would respect this choice and ask permission to check again next time, which sends the message that self-management is an important part of the treatment. Other patients may ask for more guidance, and providers can offer a behavioral menu: “Would it be okay if I shared some ideas of what worked for other patients? Some patients did x, others tried x… Do one of these ideas sound like they would work for you, or do you have an idea of your own?” Other, more self-motivated patients may easily generate an idea.
Once a patient has an idea of what they want to work on, providers would ask questions about “what, when, where, how much, and when will you start“ to help patients make the plan very specific. A SMART behavioral plan is one that is Specific, Measurable, Achievable, Relevant, and Time limited. Providers should help patients construct realistic plans that set them up for success.
The second main question in BAP is a confidence ruler: “How confident or sure do you feel that you can carry out your plan?” Rulers are a useful conversational tool in MI, even outside of action planning, because they elicit reasons (“Why did you say x and not a lower number?”) and barriers (“Why x and not a higher number?”). When confidence ratings are lower than 7 in BAP, it is necessary to problem solve to increase confidence, perhaps offering another behavioral menu of ways to modify the plan.
The last question in BAP asks, “Would be helpful to set up a check on how things are going with your plan?” Follow-up increases accountability and helps patients feel supported. Providers must be creative to allow checks within their clinic demands (eg, another clinic staff can call to check, patient can email an update, provider might set an earlier appointment, etc.). At follow up, always check in with how the patient did with their plan, normalize difficulty with completion, and positively reinforce even small steps. Regular follow up conveys the message that patient behaviors matter to the overall management of disease, they are important to you, and you will be asking about them.
Conclusion
Motivational Interviewing and Brief Action Planning are useful tools to guide providers toward collaborative conversations to enhance patient motivation for health behavior change.

Nancy Beckman, PhD, is an assistant professor in the department of Psychiatry & Behavioral Neuroscience at the University of Chicago in Chicago, IL.
References
- Sabaté E, & World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization. 2005. Available at: https://apps.who.int/iris/handle/10665/42682. Accessed April 25, 2022.
- Rollnick S, Miller, WR, Butler, CC. Motivational Interviewing in Healthcare: Helping Patients Change Behaviors. New York: Guilford Press; 2008.
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York: Guilford Press; 2012.
- Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systemic review and meta-analysis. Brit J Gen Prac. 2005;55 (513): 305-12.
- DiClemente CC, Velasquez MM. Motivational interviewing and the stages of change. In: Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York: Guilford Press; 2002.
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 1983; 51(3):390-5. https://doi.org/10.1037/0022-006X.51.3.390
- Centre for Collaboration Motivation & Innovation. Ask-Tell-Ask: An Effective Way to Give Information and Advice, 2018. Available at: https://centrecmi.ca/wp-content/uploads/2019/03/12-Ask_Tell_Ask_2018-12-21.pdf. Accessed August 1, 2021.
- Gutnick D, Reims K, Davis C, et al. Brief action planning to facilitate behavior change and support patient self-management. JCOM 2014;21(1):17-29.
- Centre for Collaboration Motivation & Innovation. Brief Action Planning. Available at: https://centrecmi.ca/brief-action-planning/. Accessed August 1, 2021.
Leave a commentOrder by
Newest on top Oldest on top