How I Do It: Ultrasound-Guided Rectus Sheath Blocks
Cite as: Grzybowski J, Schroeder K. How I do it: ultrasound-guided rectus sheath blocks. ASRA Pain Medicine News 2023;48. https://doi.org/10.52211/asra050123.012.
Background
The history of the rectus sheath block (RSB) dates to 1899 when it was first described by Schleich as a technique that results in muscle relaxation and analgesia to the abdominal wall through blockade of thoracolumbar nerves within the substance of the rectus abdominis muscle (RAM).1 Originally, the blocks were performed using a blind, loss-of-resistance technique. The accuracy and safety of a RSB is now greatly increased through the utilization of ultrasound-guidance and echogenic needles.2,3 Identification of vasculature within the vicinity of the rectus sheath, careful needle advancement reducing the risk of damage to visceral structures, and confirmation of correct injectate location are all improved with the use of ultrasound technology.
Identification of vasculature within the vicinity of the rectus sheath, careful needle advancement reducing the risk of damage to visceral structures, and confirmation of correct injectate location are all improved with the use of ultrasound technology.
Indications
A bilateral RSB provides analgesia to the anteromedial abdominal wall supplied by the ventral rami of the thoracolumbar spinal nerves (T7-L1). An RSB targets the anterior cutaneous branches (Figure 1) of the intercostal nerves as they pierce the posterior rectus sheath. An RSB may be a suitable analgesic option for patients undergoing midline abdominal surgeries with contraindications or as an alternative to neuraxial analgesia. For example, an RSB may be more appropriate in patients receiving anticoagulation therapies or where the hemodynamic perturbations associated with thoracic epidural analgesia would be poorly tolerated.
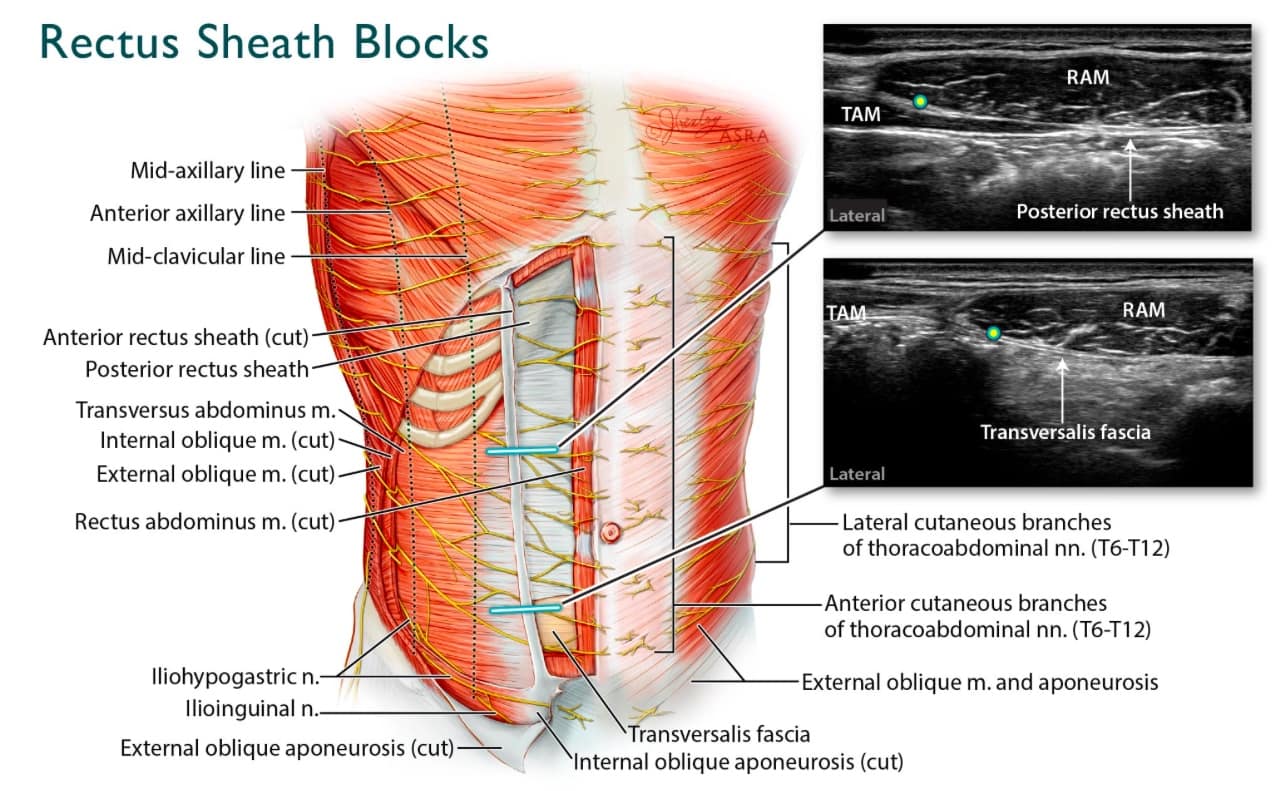
Figure 1. Rectus Sheath Block Overview: The sonograms in this figure illustrate the anatomical differences between scanning at the costal margin versus below the arcuate line (absence of posterior rectus sheath). Additionally, the anatomic diagram highlights the anterior cutaneous branches of the thoracoabdominal nerves, which are targeted in RSBs.
M=muscle, n=nerve, RAM=rectus abdominus muscle, TAM=transversus abdominus muscle
Numerous observational studies and meta-analyses support the inclusion of RSBs as an efficacious component of perioperative analgesia in surgeries ranging from gynecologic abdominal surgeries and adult and pediatric umbilical herniorrhaphy to laparoscopic surgeries and emergency midline laparatomies.4-10 In addition to reduced pain scores and decreased opioid consumption, one study demonstrated decreased opioid-related side effects (nausea/vomiting and constipation) in patients receiving bilateral RSBs.10 A randomized prospective study in pediatric umbilical hernia repair demonstrated superior perioperative analgesia in patients receiving an ultrasound-guided RSB compared with surgical site infiltration.11 Additional randomized controlled trials (RCTs) have yielded variable findings supporting the utilization of ultrasound-guided RSBs in the perioperative period. Notable findings for patients receiving RSBs include transiently improved pain scores for the first 3 hours post-operatively,12 decreased morphine requirements without significant change in pain scores compared to local wound infiltration,13 and lower post anaesthesia care unit (PACU) pain scores without significant change in analgesic use in PACU or at home.14
Clinically Relevant Anatomy
Three lenticular muscles, the external oblique muscle (EOM), internal oblique muscle (IOM), and transversus abdominis muscle (TAM), comprise the anterolateral abdominal wall. All three taper into aponeuroses as they approach the midline and ultimately form the tendinous rectus sheath that encases the RAM. These aponeuroses blend in the midline with the aponeuroses of the other side to form the linea alba. The RAM is a paired muscle that originates on the pubic symphysis and ascends vertically to insert on the xiphoid process and fifth to seventh costal cartilages. The posterior rectus sheath compartment, unlike the anterior, which is divided by transverse tendinous attachments impeding craniocaudal injectate spread, is unsegmented and represents a logical target for local anesthetic injection.15 In the superior three-quarters of the RAM, the anterior layer of the rectus sheath is formed by the EOM and IOM aponeuroses. After splitting, the IOM aponeurosis also contributes to the posterior layer of the sheath together with the TAM aponeurosis (Figure 2A).16 Inferior to the arcuate line (level of the anterior superior iliac spine), all three aponeuroses pass anterior to the RAM, forming the anterior rectus sheath. The inferior quarter of the RAM does not have a posterior rectus sheath and is lined posteriorly only by its epimysium and the transversalis fascia (Figure 2B).16
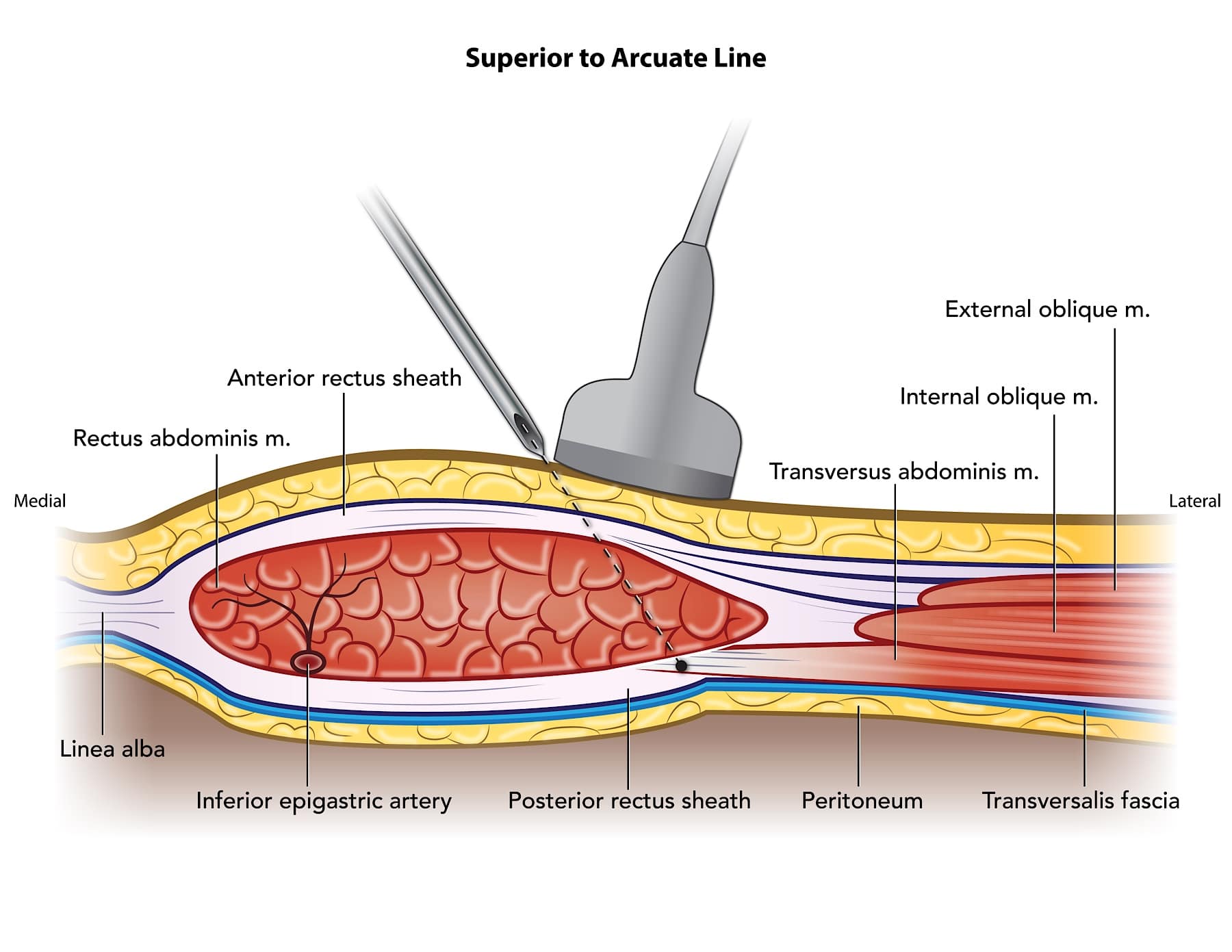
Figure 2A. Rectus Sheath Anatomy Above Arcuate Line: This diagram (above the arcuate line) represents the recommended medial to lateral needle approach that minimizes risk of visceral trauma as the TAM terminates deep to the lateral edge of the posterior rectus sheath. Care should be taken to locate epigastric vessels with color doppler ultrasound prior to needle advancement.
M=muscle
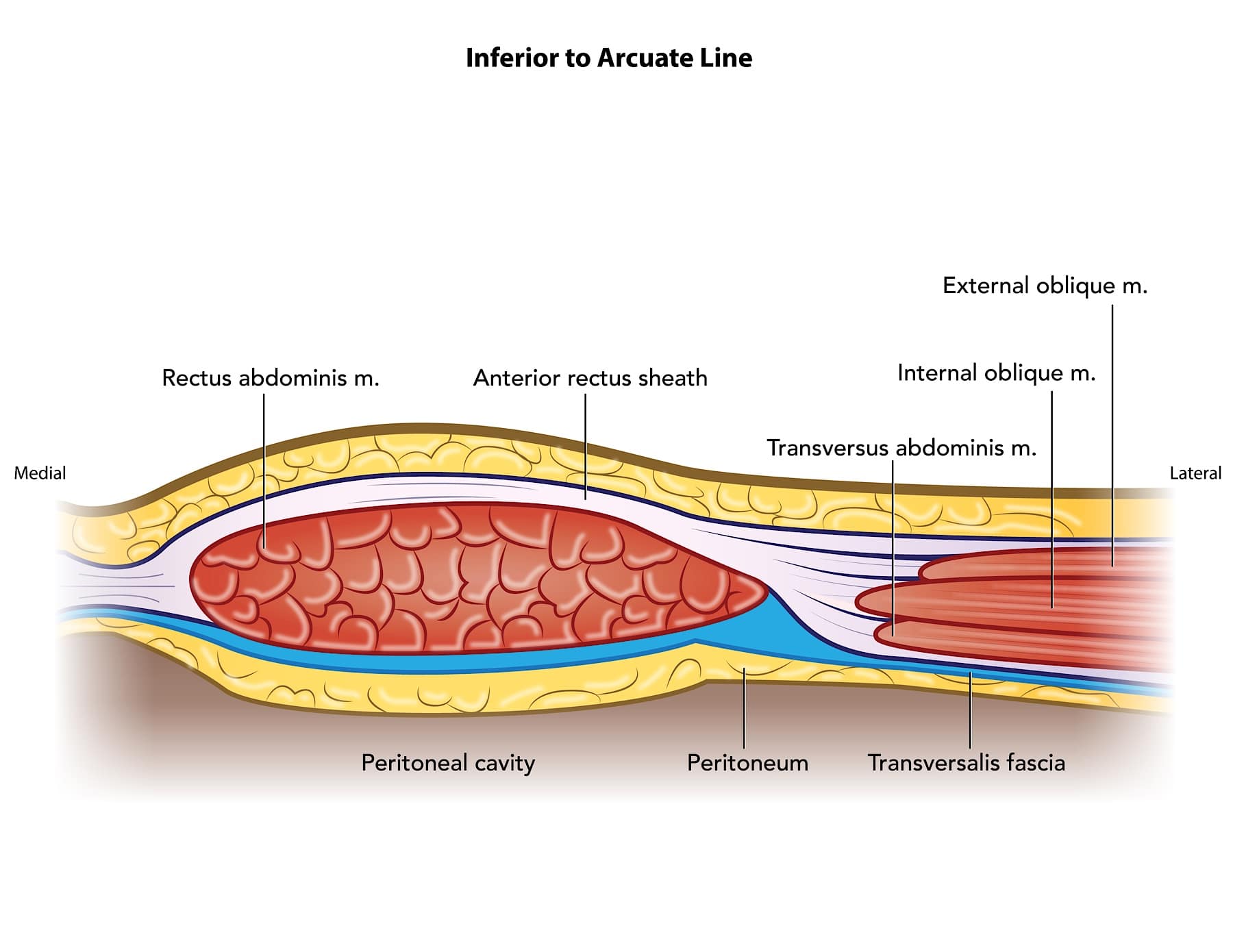
Figure 2B (Rectus Sheath Anatomy Below Arcuate Line): In contrast, this diagram illustrates all three aponeuroses contributing to the anterior rectus sheath. Thus, at points inferior to the arcuate line, the posterior rectus sheath does not exist.
M=muscle
Sonoanatomy and Technique
The goal of the rectus sheath block is to deposit local anesthetic between the RAM and the posterior rectus sheath. With the patient in the supine position, the ultrasound transducer should be placed in a transverse orientation above the umbilicus, centered approximately 1 cm from the midline (Figure 3). In obese individuals, we often prefer a low-frequency (8-3 MHz) curvilinear probe to improve visualization in the far field. However, some obese individuals exhibit thin, rather stretched out RAMs. In normal to thin individuals, a linear transducer (13-6 MHz) is adequate.

Figure 3. Ultrasound Probe Placement: With the patient in the supine position, the ultrasound transducer should be held in the transverse plane above the umbilicus, centered approximately 1 cm from the midline. The needle is advanced in-plane from medial to lateral.
The RAM and posterior rectus sheath should be identified (Figure 4) as a thick, lenticular-shaped muscle with a hyperechoic fascial covering deep to the muscle. The TAM is identified by scanning laterally and visualizing what is typically the thinnest and most hypoechoic lateral abdominal wall muscle. Ideally, the medial aspect of the TAM continuing deep to the intended target can be visualized and acts as a guide for needle trajectory (Figure 5). The needle (the authors use either a 100 mm/21-gauge or a 50 mm/22-gauge echogenic nerve block needle) is inserted using an in-plane technique and directed from medial-to-lateral as this trajectory may reduce the risk of iatrogenic visceral injury.
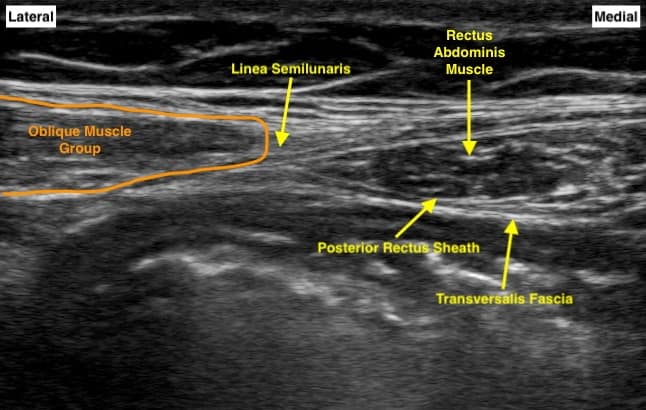
Figure 4. Rectus Sheath Block Sonoanatomy: This sonogram illustrates the double hyperechoic lines that should be visualized when performing ultrasound-guided rectus sheath blocks. The transversalis fascia is seen just deep to the posterior rectus sheath.
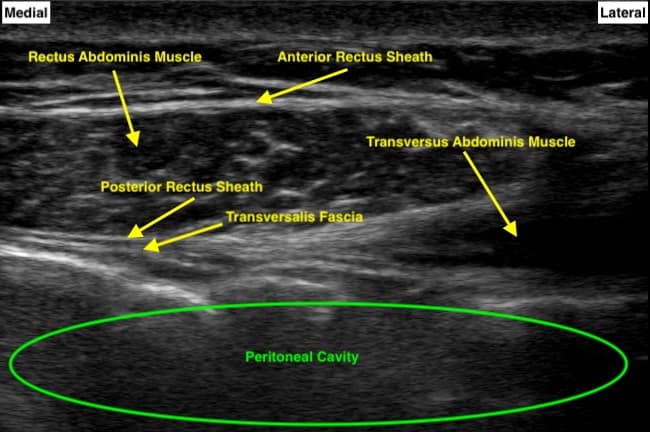
Figure 5. Rectus Sheath Block Sonoanatomy with Transversus Abdominis: This image illustrates how the underlying transversus abdominus muscle can act as a protective backstop to the viscera below when performing a rectus sheath block.
Accordingly, the TAM acts to shield the peritoneal cavity. Care should be taken to identify the superior epigastric artery with color Doppler when possible. Avoidance of needle advancement into the deep aspect of the RAM near its midpoint should minimize the risk of potential vascular trauma. A previous description of RSBs suggests a lateral to medial approach from the lateral edge of the rectus sheath for this reason.17 Once the needle tip is advanced posterior to the RAM and anterior to the posterior sheath, a small aliquot of saline is administered to hydrodissect and confirm needle tip placement prior to the injection of local anesthetic (see video).
Use of a three-way stopcock at the proximal end of the injection tubing allows for a simple transition from saline hydrodissection to local anesthetic administration. Large volume injections of local anesthetic, at least 20 mL per side, increase cephalo-caudad spread within the compartment and extend the analgesic coverage of the procedure. The block should be repeated on the contralateral side. As a single-shot RSB is likely to provide less than 24 hours of analgesia, peripheral nerve catheters (PNC) can be placed within the posterior rectus sheath using the previously described technique for when anticipated severe pain will be of a substantially longer duration. Potential risks and limitations include catheter site infection, migration of the PNC into vasculature, catheter dislodgment, and the need for postoperative catheter management and infusion pumps.
While there are no RCTs assessing RSBs with liposomal bupivacaine to date, Patzkowski et al demonstrated improved functional recovery in a patient undergoing open hemicolectomy, who received bilateral RSBs with liposomal bupivacaine.18 The authors frequently utilize a mixture of 10 mL 1.33% liposomal bupivacaine and 15 mL 0.25% bupivacaine per side when prolonged analgesia is desired without continuous nerve catheter placement. Alternatively, plain local anesthetic or mixtures with additives can be injected to prolong analgesia. This may allow bridging the time gap until proper coagulation status can be ascertained prior to thoracic epidural placement if indicated.
A RSB may be performed pre-, intra-, or post-operatively, and block timing is impacted by patient/surgeon preference and other logistical factors. In the pre-operative setting, management of desired patient sedation and respiratory variability can increase difficulty with block placement. Controlled ventilation may facilitate block placement by providing more predictable abdominal movements. In the post-operative phase of care, abdominal pain, post-surgical changes, and dressing placement may hinder block placement. Whereas a true peripheral nerve block may be more safely completed if a patient is capable of reporting paresthesia or intraneural injection, this compartment block is safe to perform in the anesthetized patient.
Continuous Catheter Technique
Rectus sheath catheter (RSC) placement represents an alternative to epidural analgesia. Both ultrasound-guided techniques performed similarly to the single shot technique above and surgeon placement of catheters under direct visualization have been described.17,19 Tsui noted that while the continuous rectus sheath block may adequately provide somatic analgesia, multimodal agents are typically needed to address visceral pain.18 The optimal RSC dosing regimen is currently unclear. Given the desired spread throughout the posterior sheath compartment, large volume, intermittent bolus dosing may be beneficial. Rucklidge et al recommend initial and subsequent dosing to each RSC of 20 mL of 0.2% ropivacaine every 6 hours.20 At the authors’ institution, programmed intermittent bolus dosing occurs to both catheters every 2 hours, with a volume of 10 mL of 0.2% ropivacaine per side, not to exceed 0.5 mg/kg/hr of ropivacaine based on ideal body weight.
Clinical Pearls
- Medial to lateral needle insertion may minimize the risk of intraperitoneal needle advancement and possible visceral injury, but deep needle placement within the mid rectus muscle might risk injury to the epigastric artery.
- Lateral to medial needle insertion might minimize possible arterial puncture and facilitate the insertion of a catheter.
- A stopcock with saline syringe attached to one port and local anesthetic attached to the other (Figure 6) allows for verification of needle position and quick transition to local anesthetic administration once appropriate needle placement is confirmed.
- Injection deep to the posterior rectus sheath and superficial to the transversalis fascia can result in a subcostal TAP spread pattern, extending laterally beyond the border of the RAM (Figure 7).
- A paucity of prospective studies on additives in fascial plane blocks is available; however, off-label use of dexamethasone and dexmedetomidine have demonstrated some ability to prolong duration of analgesia.21-22
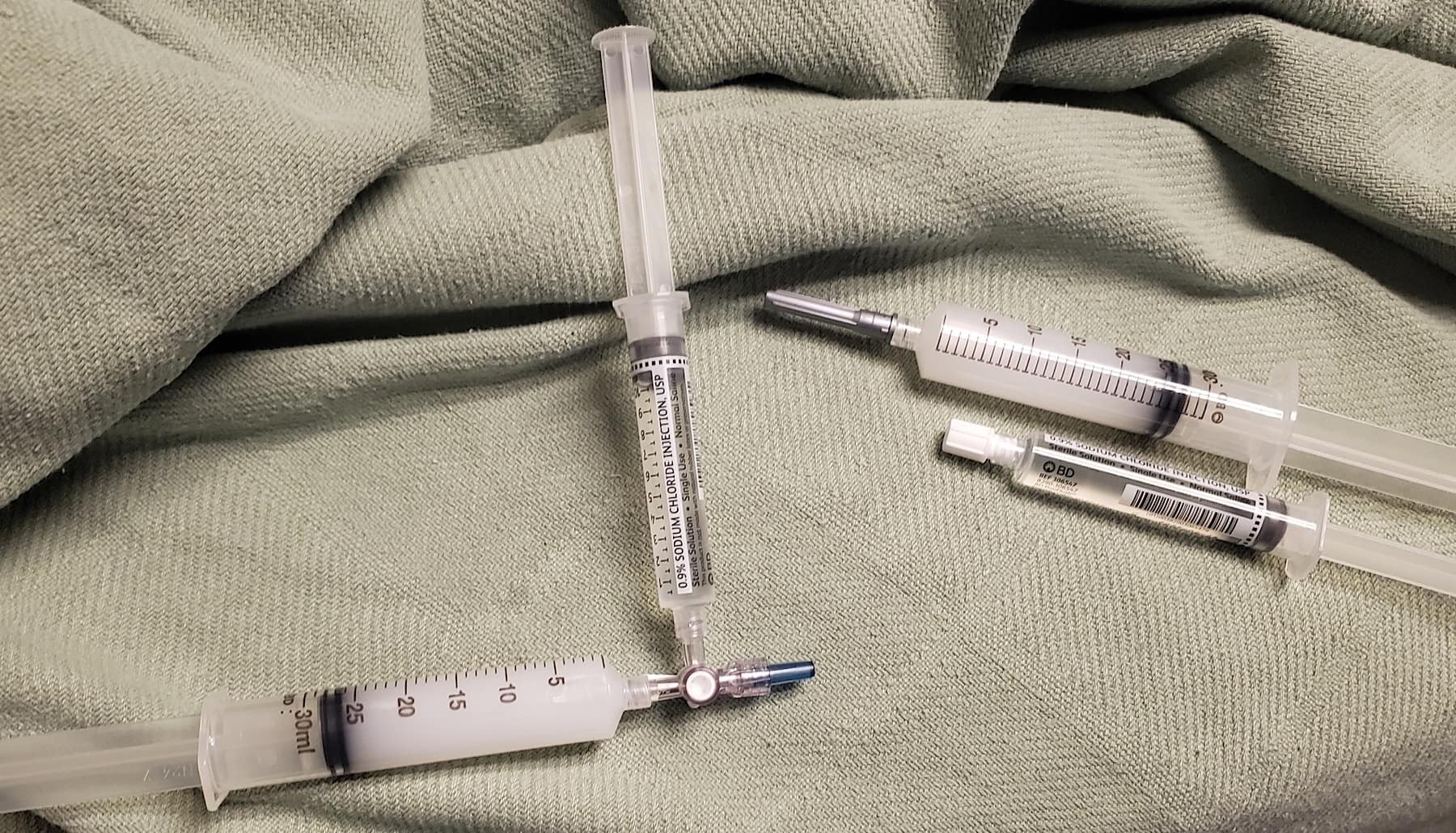
Figure 6. Medication and Equipment: A 30 mL syringe is filled with a mixture composed of 15 mL 0.25% bupivacaine and 10 mL 1.33% liposomal bupivacaine. One syringe of the 25 mL mixture is injected on each side. A saline flush syringe is attached to the other port of a three-way stopcock for initial hydrodissection prior to local anesthetic administration.
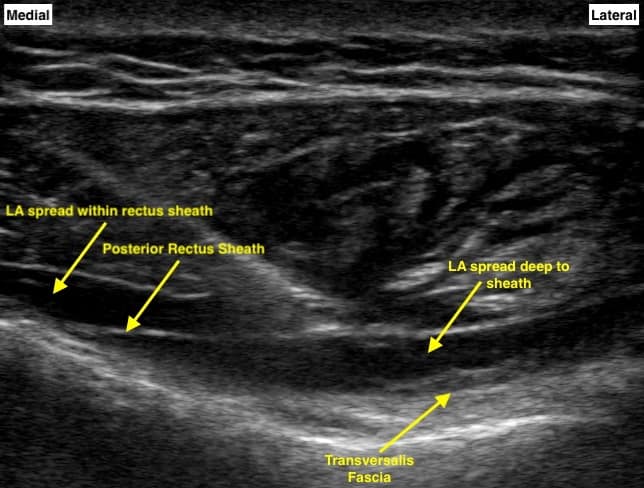
Figure 7. Post-Injection Ultrasound Imaging: This image illustrates a portion of the local anesthetic injected in the desired space, lifting the rectus abdominus muscle. Additional hypoechoic injectate is seen deep to the posterior rectus sheath, resulting in a subcostal transversus abdominis plane block.
Jeffrey S. Grzybowski, MD, is an assistant professor in the Department of Anesthesiology at the University of Wisconsin School of Medicine and Public Health in Madison, WI.
Kristopher M. Schroeder, MD, is a professor in the Department of Anesthesiology at the University of Wisconsin School of Medicine and Public Health in Madison, WI.
References
- Schleich CL. Schmerzlose Operationen. 4th ed. Berlin: Springer; 1899.
- Dolan J, Lucie P, Geary T, et al. The rectus sheath block: accuracy of local anesthetic placement by trainee anesthesiologists using loss of resistance or ultrasound guidance. Reg Anesth Pain Med 2009;34(3):247-50. https://doi.org/10.1097/AAP.0b013e31819a3f67
- Dolan J, Smith M. Visualization of bowel adherent to the peritoneum before rectus sheath block: another indication for use of ultrasound in regional anesthesia. Reg Anesth Pain Med 2009;34(3):280-1. https://doi.org/10.1097/AAP.0b013e31819a4f84
- Willschke H, Bösenberg A, Marhofer P, et al. Ultrasonography-guided rectus sheath block in paediatric anaesthesia—a new approach to an old technique. Br J Anaesth 2006;97(2):244–9. https://doi.org/10.1093/bja/ael143
- Karaarslan E, Topal A, Avcı O, et al. Research on the efficacy of the rectus sheath block method. Agri 2018;30(4):183-8. https://doi.org/10.5505/agri.2018.86619
- Kartalov A, Jankulovski N, Kuzmanovska B, et al. The effect of rectus sheath block as a supplement of general anesthesia on postoperative analgesia in adult patient undergoing umbilical hernia repair. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2017;38(3):135-42. https://doi.org/10.2478/prilozi-2018-0014
- Teshome D, Hunie M, Essa K, et al. Rectus sheath block and emergency midline laparotomy at a hospital in Ethiopia: a prospective observational study. Ann Med Surg (Lond) 2021;68:102572. https://doi.org/10.1016/j.amsu.2021.102572
- Xu L, Hu Z, Shen J, et al. Efficacy of US-guided transversus abdominis plane block and rectus sheath block with ropivacaine and dexmedetomidine in elderly high-risk patients. Minerva Anestesiol 2018;84(1):18-24. https://doi.org/10.23736/S0375-9393.17.11538-5
- Yentis SM, Hills-Wright P, Potparic O. Development and evaluation of combined rectus sheath and ilioinguinal blocks for abdominal gynaecological surgery. Anaesthesia 1999;54(5):475-9. https://doi.org/10.1046/j.1365-2044.1999.00805.x
- Hamid HKS, Ahmed AY, Alhamo MA, et al. Efficacy and safety profile of rectus sheath block in adult laparoscopic surgery: a meta-analysis. J Surg Res 2021;261:10-17. https://doi.org/10.1016/j.jss.2020.12.003
- Gurnaney HG, Maxwell LG, Kraemer FW, et al. Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair. Br J Anaes 2011;107(5):790-5. https://doi.org/10.1093/bja/aer263
- Hamill JK, Liley A, Hill AG. Rectus sheath block for laparoscopic appendicectomy: a randomized clinical trial. ANZ J Surg 2015;85(12):951-6. https://doi.org/10.1111/ans.12950
- Flack SH, Martin LD, Walker BJ, et al. Ultrasound-guided rectus sheath block or wound infiltration in children: a randomized blinded study of analgesia and bupivacaine absorption. Paediatr Anaesth 2014;24(9):968-73. https://doi.org/10.1111/pan.12438
- Dingeman RS, Barus LM, Chung HK, et al. Ultrasonography-guided bilateral rectus sheath block vs local anesthetic infiltration after pediatric umbilical hernia repair: a prospective randomized clinical trial. JAMA Surg 2013;148(8):707-13. https://doi.org/10.1001/jamasurg.2013.1442
- Chin KJ, McDonnell J, Carvalho B, et al. Essentials of our current understanding: abdominal wall blocks. Reg Anesth Pain Med 2017; 42(2):133-83. https://doi.org/10.1097/AAP.0000000000000545
- Salinas FV. How I do it: ultrasound-guided bilateral rectus sheath blocks. ASRA Pain Medicine News 2014;14(4):5-8.
- Tsui BC, Green JS, Ip VH. Ultrasound-guided rectus sheath catheter placement. Anaesthesia 2014;69(10):1174-5. https://doi.org/10.1111/anae.12849
- Patzkowski MS, Stevens G. Multimodal analgesia in abdominal sepsis: a case report of liposome bupivacaine in ultrasound-guided rectus sheath blocks after unexpected open hemi-colectomy. Mil Med 2015;180:e728-31. https://doi.org/10.7205/MILMED-D-14-00512
- Cornish P, Deacon A. Rectus sheath catheters for continuous analgesia after upper abdominal surgery. ANZ J Surg 2007;77(1-2):84. https://doi.org/10.1111/j.1445-2197.2006.03982.x
- Rucklidge M, Beattie E. Rectus sheath catheter analgesia for patients undergoing laparotomy. BJA Educ 2018;18(6):166-72. https://doi.org/10.1016/j.bjae.2018.03.002
- Ammar AS, Mahmoud KM. Effect of adding dexamethasone to bupivacaine on transversus abdominis plane block for abdominal hysterectomy: a prospective randomized controlled trial. Saudi J Anaesth 2012;6(3):229-33. https://doi.org/10.4103/1658-354X.101213
- Salem WT, Alsamahy KA, Ibrahim WA, et al. Effect of adding dexmedetomidine to bupivacaine in ultrasound guided rectus sheath block: a randomized controlled double-blinded study. The Open Anesthesia Journal 2019;13:25-30.

