Embracing Diversity: A Healthcare Immersion Program for Under-Represented High School Students, Creating a Pipeline for Diversity in Medicine
Cite as: Umeh UO, Li CJ, Beckman JD. Embracing diversity: a healthcare immersion program for under-represented high school students, creating a pipeline for diversity in medicine. ASRA Pain Medicine News 2023;48. https://doi.org/10.52211/asra110123.003.
Despite the increasing diversity of the United States population, racial and ethnic minorities continue to be underrepresented in the health professions. According to the United States Census Bureau, by 2021, only 20.6% of Latinos and 28.1% of African Americans had a bachelor’s degree compared to 41.9% of non-Hispanic whites.1 Although approximately one-third of the United States population is African American and Latino, these groups represent 20% of healthcare professionals and only 15% of physicians (United States Department of Labor, 2019).2 Recent work has found that while the “numbers and proportions of Black, Hispanic, and American Indian or Alaska Native medical school matriculants have increased, they have increased at a rate slower than their age-matched counterparts in the United States population.3 Therefore, the United States medical workforce does not reflect the patient population for which it cares. A diverse healthcare workforce improves cultural competency and patient compliance while creating a better-suited system to address the vast health disparities evident in disadvantaged communities.2,3,4 One approach to address this disparity is by expanding the educational pipeline for students traditionally underrepresented in medicine (URIM).2,4-6 In early 2020 with the onset of COVID-19 pandemic and associated disparities in morbidity and mortality, there has been a resurgent impetus to minimize disparities and improve health outcomes.
One method to accomplish these goals is to continue to diversify the workforce within our health care system. Pipeline and pathway programs aim to accomplish this goal. The Healthcare Immersion Program at Hospital for Special Surgery (HIP at HSS) is a 2-day program with the objective to provide high school students with exposure to different careers in healthcare. Our HIP at HSS program is targeted toward URIM students, a group which has traditionally faced barriers to adequate education, especially in New York City’s public-school systems. Primary barriers to educational equity are disproportionate poverty and a lack of access to high quality early education. Addressing these barriers is a larger societal issue that will take prolonged and determined effort to overcome.
The HIP at HSS program offers an opportunity for students to gain early insight into a career in medicine and hopes to create a pipeline to promote diversity in medicine. For program directors, Dr. Uchenna Umeh and Dr. James Beckman, the goals of the weekend program were threefold: to create an enriched healthcare immersion program for URIM 9-12th-grade students from New York City Public schools; to provide CPR training to empower students to action during healthcare emergencies in their communities; and finally, to strengthen URIM students' desire to pursue careers in healthcare.
The response to our program was overwhelmingly positive. Student feedback via post program surveys revealed that they enjoyed the program and many “wished it was longer.”
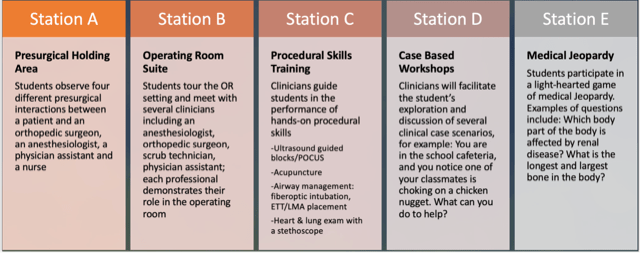
The immersive program was designed to accomplish these goals over 2 days. Students were exposed to healthcare-specific activities, including medical simulations, skills workshops (eg, fiberoptic intubation, ultrasound blocks, and vascular access techniques), acupuncture, POCUS training, problem-based case discussions, Medical Jeopardy, and in-hospital tours and instruction created and led by an HSS team of physicians (attendings, fellows, and residents), physician assistants, nurses, scrub and x-ray technicians. The Saturday curriculum included two lectures and then five stations through which the students could cycle for 50 minutes with 10 minutes to move between stations (Figure 1). Sunday was reserved for a half day of CPR training.
Student selection was a challenging piece of the puzzle. To ensure that the program welcomed students who would benefit most from our program, HIP at HSS partnered with Mentoring in Medicine (MIM) Inc., a non-profit organization based in the Bronx, NY and founded by Dr. Lynne Holden, an emergency room physician. MIM was founded to inspire disadvantaged and low-income students to become health care professionals through academic enrichment, leadership development, civic engagement, and mentoring programs. MIM works with schools serving under-represented populations throughout NYC and beyond. Dr. Holden worked with several high schools in the Bronx and Manhattan, and each school selected several students to apply to the HIP at HSS Program.

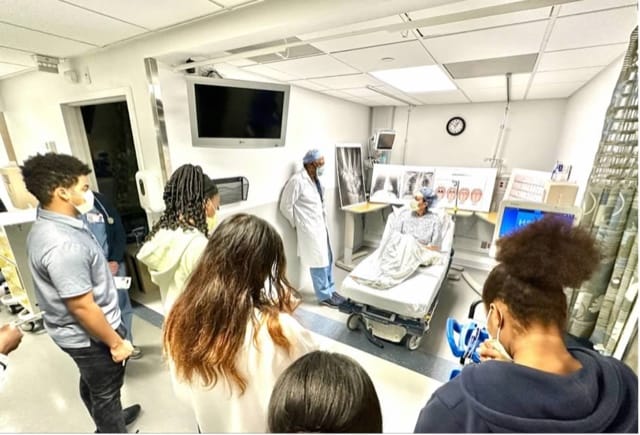
On March 4-5, 2023, HSS welcomed 28 students for the inaugural weekend session with more than 35 volunteer staff members over both days (Figure 2). The morning began with breakfast and two introductory lectures, “Why Healthcare” and “Diversity in Medicine.” The “Why Healthcare” lecture was delivered by Roberta Stack, the assistant vice-president within our anesthesiology department. Her talk emphasized the continued importance and growth of healthcare over the years and highlighted career opportunities in healthcare, including those outside the traditional roles of physician and nurse. The “Why Diversity” lecture was given by Dr. Daphne Scott, an HSS sports medicine physician. Dr. Scott highlighted the disparities in representation in medicine and methods to close the gap. Students then began the immersion program and rotated through five distinct 1-hour stations designed to engage and educate them about different aspects of healthcare. Each station was staffed by an interdisciplinary group of HSS staff, including orthopedic surgeons, anesthesiologists, physician assistants, registered nurses, and scrub technicians, etc. The variety of staff exposed the students to numerous avenues for job opportunities in the healthcare sector. The five stations gave the students an opportunity to visit the preoperative holding area and operating room as well as the recovery room where some procedural stations were set up (Figures 3-10).









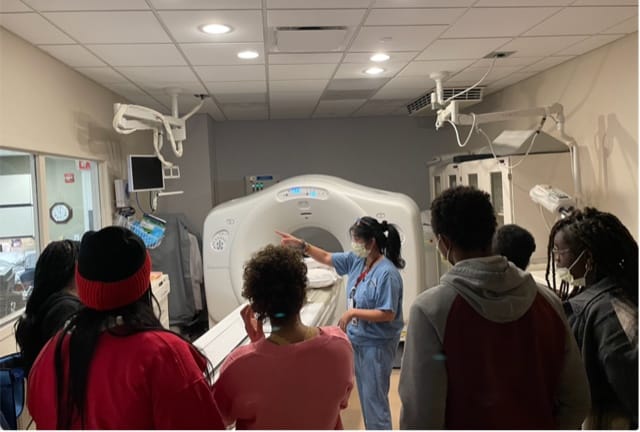
On the second day, all the students returned for CPR training led by two HSS anesthesiologists, Dr. Elaine Yang and Dr. Mandip Kalsi. The morning commenced with breakfast, and then the students were divided into two groups. One group watched a video and had a lecture about CPR followed by a Q & A session with Drs. Yang and Kalsi and then CPR training (Figures 11-12). The second group went on a hospital tour led by additional hospital staff. On the tour, the students had the opportunity to visit the inpatient pediatric unit as well as the radiology and MRI suites (Figure 13). During the tour, students had the opportunity to discuss how x-ray machines, CT scans, and MRIs function with the radiology technician. In the inpatient unit, they spoke to the charge nurse and learned about her role in caring for orthopedic patients after surgery.
The response to our program was overwhelmingly positive. Student feedback via post program surveys revealed that they enjoyed the program and many “wished it was longer.” We are especially proud of the interdisciplinary nature of our program and understand that engagement and involvement of our colleagues across the institution was critical to the program’s success.
Overall, we hope the HIP at HSS will help catalyze a future career in medicine for the students and increase the diversity of the healthcare workforce as well as address the healthcare diversity gap. We look forward to welcoming another cohort of students.
*We would like to acknowledge and thank Dr. Gregory Liguori, our chief of anesthesia, for his unwavering support; Dr. Stephen Haskins, chief medical diversity officer at HSS for his early support and guidance with building the program. Lindsey Janoskie, HIP at HSS Program coordinator, for the countless hours spent helping organize the program—creating the program brochure and website and coordinating the students and all the weekend of details. Roberta Stack for championing the program from the beginning and getting the necessary support from hospital leadership. Junior Rigby, anesthesia tech, who was onsite for the weekend to ensure everything ran smoothly. And lastly to all the HSS staff that volunteered their time to teach the students.



References
- United States Census Bureau. Census Bureau releases new educational attainment data. https://www.census.gov/newsroom/press-releases/2022/educational-attainment.html. Published February 24, 2022. Accessed August 28, 2023.
- Brownrigg M, Patel S, Roedersheimer K et al. Propelling Adolescents Toward Careers in Healthcare (PATCH): a medical student led pipeline program for high school students underrepresented in medicine. J Health Dispar Res Pract 2020;13(4), Article 1. https://digitalscholarship.unlv.edu/jhdrp/vol13/iss4/1.
- Mora H, Obayemi A, Holcomb K, et al. The national deficit of Black and Hispanic physicians in the US and projected estimates of time to correction. JAMA Netw Open 2022;5(6):e2215485. https://doi.org/10.1001/jamanetworkopen.2022.15485
- Muppala V, Janwadkar R, Rootes A, et al. Creating a pipeline for minority students: medical student led programming. 2021; Cureus 13(4):e14384. https://doi.org/10.7759/cureus.14384
- Danner OK, Lokko C, Mobley F, et al. Hospital-based, multidisciplinary, youth mentoring and medical exposure program positively influences and reinforces health care career choice: “The Reach One Each One Program Early Experience.” Am J Surg 2017;213(4):611-16. https://doi.org/10.1016/j.amjsurg.2016.12.002
- Patel SI, Rodríguez P, Gonzales RJ. The implementation of an innovative high school mentoring program designed to enhance diversity and provide a pathway for future careers in healthcare related fields. J Racial Ethn Health Disparities 2015;2(3):395-402. https://doi.org/10.1007/s40615-015-0086-y