How I Do It: Implementing Virtual Reality for Genicular Nerve Radiofrequency Ablation
Cite as: Schmitt K, Miller R, Nelson A, et al. How I do it: implementing virtual reality for genicular nerve radiofrequency ablation . ASRA Pain Medicine News 2024;49. https://doi.org/10.52211/asra020124.012.
Despite rapid advancements in medical technology and treatments, pain and anxiety persist as common features of non-sedative medical procedures. Considering the significant role anxiety and stress play in pain perception, finding modalities to disrupt the sensory experience during procedural interventions offers a potential solution to enhance patient satisfaction and improve clinical outcomes. As technology and healthcare continue to evolve, emerging innovations offer alternatives to pharmaceuticals for managing pain and anxiety during medical procedures. This is noted through the implementation of virtual reality (VR) in medical procedures to address the anxiety, stress, and pain experienced by patients.1 The analgesic advantages observed in VR immersion have been suggested to result from both temporary distraction and enduring neuroplastic changes.2,3
Consisting of a head-mounted display (HMD) with visual and auditory outputs, VR has been successfully implemented in reducing pain for a number of chronic pain conditions, including phantom limb pain and subacromial impingement syndrome.4 However, its potential application in chronic pain procedures has been underutilized and explored to a limited extent.
The Department of Pain Medicine at the University of California Irvine (UCI) Health is currently investigating how VR can be implemented to address procedural pain and anxiety in chronic pain patients. Knee pain secondary to knee osteoarthritis (OA) remains a prevalent cause of decreased quality of life and disability with notable dissatisfaction rates associated with health-related quality of life post-surgical intervention.5 Genicular nerve radiofrequency ablation (GNRFA) serves as an alternative approach as compared to surgery for addressing chronic knee pain, especially for patients with knee OA.6 Studies have shown GNRFA may provide up to 60% relief of knee pain for approximately 6 months.7 However, GNRFA and similar medical procedures may be painful and anxiety-provoking throughout the duration of intervention unless sedation techniques are employed. Our team of researchers and pain specialists is committed to addressing this issue, particularly affecting patients undergoing GNRFA. These individuals include chronic knee pain patients who are not suitable for surgery, those who choose not to pursue surgical recommendations, or individuals who have experienced persistent postoperative knee pain. In this article, we describe the implementation and use of a virtual reality HMD for GNRFA procedures at our institution.
Patient Considerations
When considering a therapeutic approach, identifying the patients who stand to gain the most from an intervention is important for maximizing benefits while preventing unnecessary distress and treatment. Conceivable side effects with VR utilization include "cybersickness," which exhibits similar symptoms to motion sickness, such as disorientation, nausea, and visual discomfort.8 A prevailing explanation for cybersickness is grounded in the Sensory Conflict Theory, which describes the incongruity between the ocular and vestibular systems when an expected motion or acceleration is absent.9 Additionally, neurological concerns, including ocular or vestibulocochlear issues, may decrease noted benefits with the application of VR due to device reliance on visual and auditory outputs. Distinguishing whether patients have a history of motion sickness with or without VR as well as any significant visual or auditory impairments may be important in discerning whether to proceed with VR usage. However, VR therapy has previously been demonstrated to be safe and applicable in the realm of acute and chronic pain management,10-12 with the absolute contraindication being a patient's refusal of VR modalities.
Consisting of a head-mounted display (HMD) with visual and auditory outputs, VR has been successfully implemented in reducing pain for a number of chronic pain conditions, including phantom limb pain and subacromial impingement syndrome.
The Setup: Virtual Reality Intervention
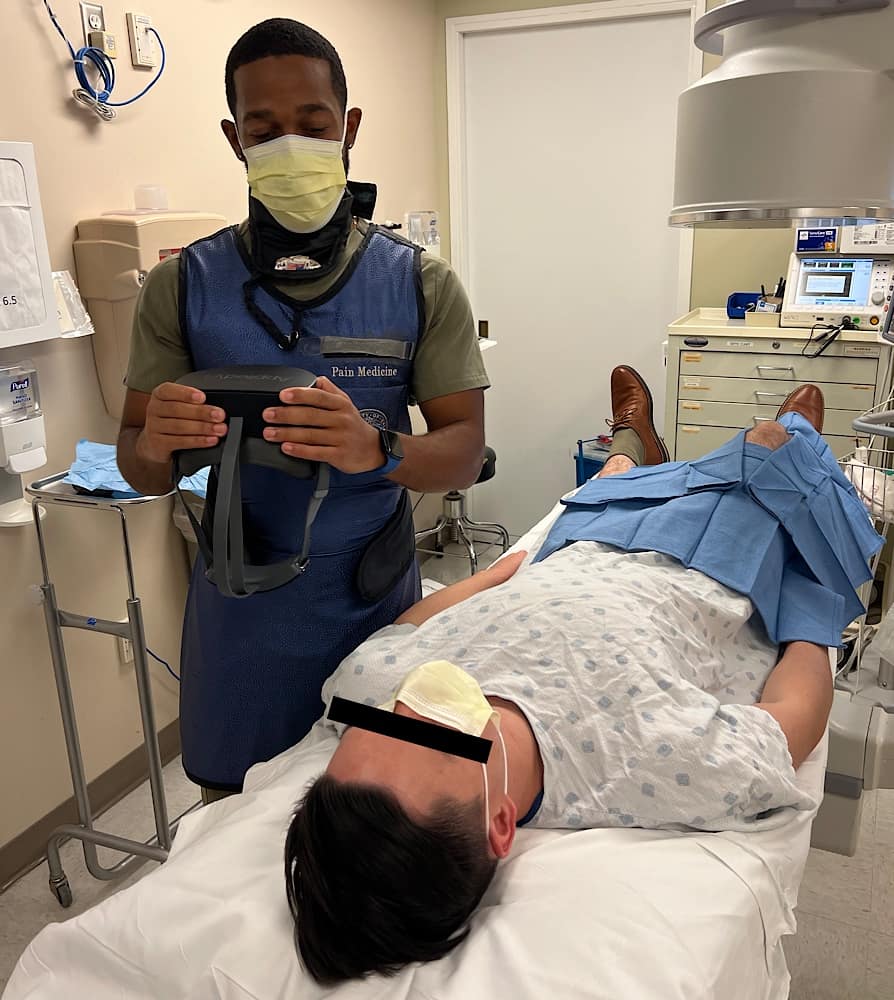
Clinical and research staff underwent training to effectively utilize and implement our VR therapy intervention, AppliedVR's SootheVRx system. This includes an HMD equipped with a high-resolution 4K screen and audio capabilities offering a selection of multiple VR environments to choose from. Before the patient encounter, the system underwent initial cleaning in accordance with institution protocol and device instructions. Subsequently, an assessment of the device's battery life and functionality was conducted followed by a final round of cleaning. Once the patient arrived for the appointed procedural time, the VR device was made available prior to the procedure. This was accompanied by instructions on its usage and time for questions while allowing for acclimation to the device (Figure 1).

Cybersickness has been previously noted to present within the first 10 minutes of usage for a majority of users.13 A preprocedural acclimation period serves the dual purpose of providing familiarity with the device while allowing for observation of symptoms. To assist with the clinical flow, patients were directed to explore two to three specific virtual reality environments. This ranged from soaring over scenic mountain ranges to watching the sunset on a beach (Figure 2). The VR headset was then briefly paused and retrieved from the patient once instructions for procedural preparation and positioning were given.

The Procedure: Genicular Nerve Radiofrequency Ablation
GNRFA generally involves distributing targeted radiofrequency energy to the genicular nerves surrounding the knee, effectively ablating and alleviating symptoms associated with knee OA.14 Literature has detailed considerations and procedural approaches pertaining to GNRFA.14-16 It is worth noting that patients are generally positioned in the supine orientation for GNRFA with preparation and procedural focus primarily directed toward the lower extremities (Figure 3). This provides a favorable environment for VR immersion through an HMD due to minimized disruption of the procedural setup and intervention. Following patient positioning on the procedural bed and in tandem with procedural preparation, the VR device was again made available to the patient for continuous use throughout the procedure (Figure 4). Occipital and cervical support can be modified as needed, considering the patient's comfort and preferences in regard to the use of a VR device. During the procedure, a clinical team member periodically assesses the patient's ability to communicate, comfort level, and any requirements related to VR use (Figure 5). This may involve adjusting volume settings, device positioning, or additional occipital and cervical support. Patients were instructed to avoid making adjustments themselves to minimize patient movement and disruptions throughout the intervention.


Post Procedural Considerations
Upon the conclusion of the procedure, careful monitoring of any lingering effects related to the use of the virtual reality headset is warranted. Residual side effects associated with VR usage may encompass symptoms such as motion sickness, dizziness, eye strain, headaches, or other visual abnormalities.9,13 Hence, before repositioning and transferring the patient from the procedural bed, we inquired about the presence of any of these side effects. Patient postoperative care and discharge are otherwise directed by respective institution guidelines.
Conclusions
VR therapy is an emerging modality under investigation for alleviating pain and anxiety associated with chronic pain procedures. Our newsletter article, supplemented with descriptions and images, serves as a guide for implementing VR in GNRFA procedures while also stimulating further exploration of VR therapy within the broader practice of chronic pain interventions.


References
- Li A, Montaño Z, Chen VJ, et al. Virtual reality and pain management: current trends and future directions. Pain Manag 2011;1(2):147–57. https://doi.org/10.2217/pmt.10.15
- Mahrer NE, Gold JI. The use of virtual reality for pain control: a review. Curr Pain Headache Rep2009;13(2):100-9. https://doi.org/10.1007/s11916-009-0019-8
- Cheung KL, Tunik E, Adamovich SV, et al. Neuroplasticity and virtual reality. In: Weiss P, Keshner E, Levin M. (eds) Virtual Reality for Physical and Motor Rehabilitation. Virtual Reality Technologies for Health and Clinical Applications. New York, NY: Springer, 2014. https://doi.org/10.1007/978-1-4939-0968-1_2
- Wylde V, Dieppe P, Hewlett S, et al. (2007). Total knee replacement: is it really an effective procedure for all? Knee 2007;14(6):417-23. https://doi.org/10.1016/j.knee.2007.06.001
- Pourmand A, Davis S, Marchak A, et al. (2018). Virtual Reality as a clinical tool for pain management.Curr Pain Headache Rep 2018;22(8):53. https://doi.org/10.1007/s11916-018-0708-2
- Kidd VD, StrumSR, Strum DS, et al. Genicular nerve radiofrequency ablation for painful knee arthritis: the why and the how. JBJS Essent Surg Tech 2019;9(1):e10. https://doi.org/10.2106/JBJS.ST.18.00016
- Iannaccone F, Dixon S, Kaufman A. Retrospective review a review of long-term pain relief after genicular nerve radiofrequency ablation in chronic knee osteoarthritis. Pain Physician2017;20(3):E437-44.
- Ahmadpour N, Randall H, Choksi H, et al. Virtual Reality interventions for acute and chronic pain management. Int J Biochem Cell Biol 2019;114:105568. https://doi.org/10.1016/j.biocel.2019.105568
- Smith V, Warty RR, Sursas JA, et al. The effectiveness of virtual reality in managing acute pain and anxiety for medical inpatients: systematic review. J Med Internet Res 2020;22(11):e17980. https://doi.org/10.2196/17980
- Mallari B, Spaeth E, Goh H, et al. Virtual reality as an analgesic for acute and chronic pain in adults: a systemic review and meta- analysis. J Pain Res 2019;12:2053-85. https://doi.org/10.2147/JPR. S200498
- Spiegel B, Fuller G, Lopez M, et al. Virtual reality for management of pain in hospitalized patients: a randomized comparative effectiveness trial. PLoS One 2019:14(8)e0219115. https://doi.org/10.1371/journal.pone.0219115
- Maani C, Hoffman H, Fowler M, et al. Combining ketamine and virtual reality pain control during severe burn wound care: one military and one civilian patient. Pain Med 2011;12(4):673-8. https://doi.org/10.1111/j.1526-4637.2011.01091.x
- Kim YY, Kim HJ, Kim EN, et al. Characteristic changes in the physiological components of cybersickness. Psychophysiology 2005;42(5):616-25. https://doi.org/1111/j.1469-8986.2005.00349.x
- Davis T, Loudermilk E, DePalma M, et al. Prospective, multicenter, randomized, crossover clinical trial comparing the safety and effectiveness of cooled radiofrequency ablation with corticosteroid injection in the management of knee pain from osteoarthritis. Reg Anesth Pain Med 2018;43(1):84-91. https://doi.org/10.1097/AAP.0000000000000690
- Choi WJ, Hwang SJ, Song JG, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain 2011;152(3):481-7. https://doi.org/10.1016/j.pain.2010.09.029
- Kim SY, Le PU, Kosharskyy B, et al. Is Genicular nerve radiofrequency ablation safe? a literature review and anatomical study. Pain Physician 2016;19(5):E697-E705