Peripheral Nerve Blocks for Urologic Procedures
Opioid analgesia is associated with adverse effects such as nausea and vomiting, sedation, respiratory depression, and urinary retention caused by detrusor tone relaxation while sphincter tone is maintained.1 Systemic opioid use is linked to prolonged postanesthesia care unit stays, increased costs, and decreased patient satisfaction.1 Regional anesthesia can be a satisfactory alternative or adjunct for various types of surgeries, including orthopedic, gynecologic or obstetric, open abdominal, thoracic, and breast surgery. However, it is used less often for urologic surgery. This may be because urologic nerve blocks are less frequently studied and can be more technically complex in men than in women.2 The following review of regional anesthesia techniques for urologic procedures may help physicians expand the patient population benefiting from regional anesthesia.
Dorsal Penile Blocks
Anatomy
The pudendal nerve (S2–S4) divides into the right and left dorsal nerves of the penis that pass under the pubis symphysis and travel below Buck’s fascia (deep fascia of the penis) to supply sensory innervation to the penis.
Indications
Dorsal penile blocks are used for circumcision,3,4 zipper entrapments,5 urethral surgery,6 catheter-related bladder discomfort,6 priapism,5 and repair of penile lacerations.5
Procedural technique
Anatomical/landmark approach: Dorsal penile blocks are more commonly performed using landmark techniques. With the patient in the supine position, the right and left dorsal penile nerves may be anesthetized near the base of the penis. First, retract the penis gently in a caudate direction. Insert a needle (often 27 gauge) on either side of the midline (10 and 2 o’clock positions) immediately distal to the inferior ramus of the pubic bone. Advance the needle approximately 0.5 cm in a slightly medial and caudal direction until a pop is felt as it passes through Scarpa’s fascia.4 Aspirate to verify that the needle is not intravascular, and then inject approximately 2 mL of local anesthetic on each side. An alternative approach is to inject 2 mL of local anesthetic on either side of the midline while avoiding the superficial dorsal penile vein. In adults, ropivacaine 0.33% has also been used successfully for catheter-related bladder discomfort.6 See Figure 1.
Historically, investigators have found that more than 50% of cancer patients have inadequate pain control.
In neonates and children (under 10 kg), a 30-gauge needle can be used to perform bilateral injections of 0.2–0.4 mL 1% lidocaine (at the 10 and 2 o’clock positions). To avoid systemic toxicity in a neonatal population, no more than 4.5 mg/kg lidocaine should be injected.
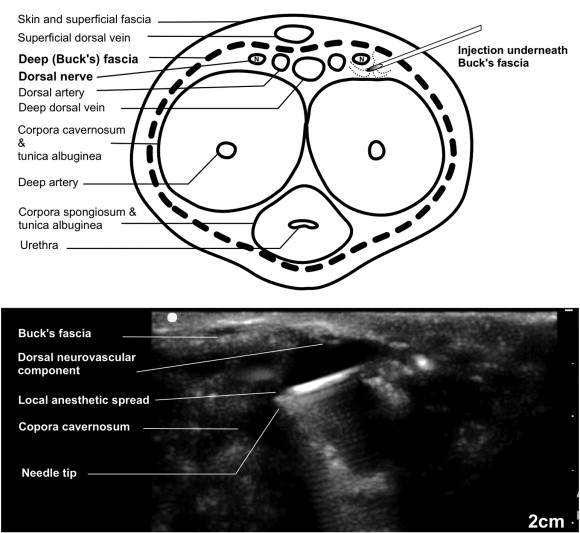
Figure 1. Dorsal penile nerve block Reprinted from Flores S, Herring AA. Ultrasound-guided dorsal penile nerve block for ED paraphimosis reduction. Am J Emerg Med. 2015;33(6):863.e3–e5. https://doi.org/10.1016/j.ajem.2014.12.041
Ultrasound-guided approach: Real-time ultrasound guidance may also be used to facilitate the correct deposition of local anesthetic. With the patient in the supine position, place a high-frequency probe transversely at the base of the dorsal aspect of the penis. Landmarks include the deep dorsal vein, paired dorsal arteries, and deep (Buck’s) fascia. Under ultrasound guidance, advance a 22-gauge needle until it is visualized piercing Buck’s fascia at the base of the penis. Depending on the duration of analgesia required, different local anesthetics may be selected. For a medium duration block, approximately 5 mL of 1% lidocaine may be injected into the potential space between Buck’s fascia and the tunica albuginea. Of note, injecting with epinephrine can cause penile ischemia and necrosis. With this technique, both dorsal penile nerves are anesthetized from a single injection.5
Ilioinguinal and Iliohypogastric Blocks
Anatomy
Traveling anterior to the psoas, quadratus lumborum, and iliacus muscles, the ilioinguinal and iliohypogastric nerves (anterior division of L1) penetrate the transversus abdominis near the anterior portion of the iliac crest. The ilioinguinal nerve then pierces the internal oblique muscle and travels with the spermatic cord through the superficial inguinal ring. The anterior division of the iliohypogastric nerve provides sensation to the skin of the pubic region as it penetrates the internal and external oblique muscles above the superficial inguinal ring.7
Indications
Ilioinguinal and iliohypogastric blocks can be used for anesthesia and postoperative analgesia for inguinal crease and hernia repair,8 groin surgeries,8 surgeries in the pubic region,7 orchidopexy,2 or surgeries in the anterior part of the scrotum.2
Procedural technique
Anatomic/landmark approach: The needle entry point is approximately 2 cm medial and 2 cm superior to the anterior superior iliac spine (ASIS). Insert a 22-gauge needle in a cephalolateral direction and advance until it contacts the inner surface of the ileum. Inject local anesthetic (eg, 0.5% levobupivacaine) into the muscular layers of the abdominal wall while withdrawing the needle. Alternatively, a needle can be inserted at a site 2 cm medial and 2 cm cephalad to the ASIS. On insertion, the needle may lose resistence as it passes through the external oblique and remains superficial to the internal oblique muscle; inject local anesthetic into this plane. Further advance the needle until a subsequent loss of resistance positions the needle tip between the internal oblique and transversus abdominus muscle, and again inject ocal anesthetic into this plane. For this technique, a small volume of local anesthetic (2 mL) can be injected into each plane with a perpendicular needle insertion as well as with needle repositioning to medial and lateral locations. Single injections of larger volumes of local anesthetic in each location (10 mL) may also result in spread of local anesthetic sufficient to produce satisfactory analgesia.8
The landmark technique often requires an experienced physician with adequate palpation skills to appreciate the pops of loss of resistance as the needle moves through the aponeurosis of the external and internal oblique muscles to confirm that the anesthetic is injected in the correct fascial plane.7
Ultrasound-guided approach: With the patient in the supine position, palpate the ASIS and place the ultrasound probe obliquely on the abdomen, on a line joining the ASIS with the umbilicus. The abdominal wall medial and superior to the ASIS has three muscle layers: the external oblique (EOM), internal oblique (IOM), and transversus abdominis muscles (TAM). The iliohypogastric and ilioinguinal nerves are located in the plane between the TAM and the IOM and pierce the TAM above the ilium. They often appear as hypoechoic ovals that are up to 1 cm apart. The deep circumflex iliac artery is evident on color Doppler and lays adjacent to the nerves in the same plane. To perform the block, insert a needle in plane to the ultrasound probe in a medial to lateral orientation through the subcutaneous tissue, EOM, and IOM. Advance the needle toward the ilioinguinal and iliohypogastric nerves until the needle tip is positioned between the IOM and TAM.
In an adult patient, 10 mL of local anesthetic (eg, ropivacaine 0.5%) per side is usually satisfactory. In children, a volume of 0.15 mL/kg per side is adequate. If the nerves cannot be visualized, Doppler testing can help identify the branch of the deep circumflex artery, which runs parallel to the ilioinguinal nerve in the same plane.7
Pudendal Nerve Blocks
Anatomy
The pudendal nerve arises from the sacral plexus with contributions from the ventral rami of S2–S4. It exits through the greater sciatic foramina inferior to the piriformis muscle, crosses the posterior aspect of the sacrospinous ligament at the level of the ischial spine, and reenters the pelvis through the lesser sciatic foramina. It then travels posteroinferiorly through Alcock’s canal (pudendal canal) and divides into the inferior rectal nerve, perineal nerve, and dorsal nerve of the clitoris or penis.9 This provides innervation to the urethral muscles, clitoris, penis, perineum and pelvic floor sphincter, urethra, and bladder triangle.10
Indications
Pudendal nerve blocks can be used in obstetric vaginal delivery,9 vaginal repairs,10 sphincterotomy,10 anorectal procedures such as hemorrhoidectomy,9 urologic procedures such as urethroplasty for urethral stricture,9 catheter-related bladder discomfort,10 transurethral resection of the prostate,9,10 and diagnosing pudendal neuralgia.9,10
Procedural technique
Anatomic/landmark approach: Transvaginal pudendal nerve blockade is a relatively straightforward procedure that uses the ischial spine as a landmark. In male patients, difficulty appreciating anatomic landmarks often necessitates the use of ultrasound guidance to facilitate block placement.9 In female patients, the ischial spine is easily palpated transvaginally with the patient in the lithotomy position. Local anesthetic is typically injected posterior to the ischial spine at the attachment of the sacrospinous ligament. Injecting anesthetic medial to the ischial spine maximizes the distance between the needle trajectory and important structures such as nerves and the pudendal artery.9
Pudendal nerve blocks can also be performed with a perirectal approach using nerve stimulation with the patient in the recumbent or jack-knife position.11 Insert the index finger of the nondominant hand into the anus to palpate the ischial spine. Inject local anesthetic at the site of needle insertion, between the external anal sphincter and ischial tuberosity. Guide the nerve stimulator needle through the ischiorectal fossa to just under the ischial spine. At the injection point, apply a 22-gauge 10-cm nerve stimulator needle with a stimulating current of 1.0–2.0 mA at 1 Hz. Verify stimulation of the pudendal nerve by ipsilateral contractions of the external anal sphincter. When the stimulating current can be reduced to 0.5–0.6 mA, perform the injection (eg, with 5 mL of 0.25% bupivacaine).11
 Figure 2. Pudendal nerve block Image courtesy of Arun Kalava, MD
Figure 2. Pudendal nerve block Image courtesy of Arun Kalava, MD
Ultrasound-guided approach: With the patient in the dorsal lithotomy position, palpate the ischial tuberosity. The sacrotuberous ligament can be identified medially. Use color Doppler to identify the internal pudendal artery under the sacrotuberous ligament. Insert a stimulating needle in plane to the ultrasound probe and medial to the pudendal artery while applying a current of 1.5–2 mA. The stimulus can be reduced to 0.8–0.6 mA after eliciting a perianal, scrotal, and penile twitch. Inject local anesthetic medial to the pudendal artery, and watch for elimination of muscular contractions. Needle insertion is generally 4–5.5 cm deep, depending on body habitus. Repeat the procedure on the contralateral side.9 See Figure 2.
Paravertebral Blocks
Anatomy
The paravertebral block (PVB) is a block of the mixed nerve after it exits the intervertebral foramen. The paravertebral space is a wedge-shaped area that is bordered posteriorly by the superior costotransverse ligament, anterolaterally by the pleura, and medially by the vertebral body.1 The paravertebral space contains both thoracic spinal nerves and the sympathetic trunk. Local anesthetic injected into the paravertebral spreads laterally to the intercostal space, medially to the epidural space, and cephalad or caudad to adjacent paravertebral spaces.
Indications
Paravertebral blockade can be used in hand-assisted laparoscopic nephrectomy (HALN), 1 percutaneous nephrolithotomy (PCNL),12 and extracorporeal shock wave lithotripsy (ESWL).13
Procedural technique

Figure 3. Anatomic/landmark paravertebral block Image courtesy of Arun Kalava, MD.
Anatomic/landmark approach: To perform a landmark-assisted paravertebral block, position the patient in the sitting, lateral, or prone position; identify the spinous processes of the operative dermatomes; and make a mark 2.5 cm lateral to the spinous processes. Insert a needle perpendicular to the skin until the transverse process is identified. Withdraw the needle, redirect it cephalad, and advance an additional 1 cm beyond where the transverse process was contacted. Loss of resistance and stimulation techniques have also been used in an effort to improve localization of the paravertebral space.1 See Figure 3.
Ultrasound-guided approach: Positioning for ultrasound-guided paravertebral blocks is similar to that used for landmark based approaches. Obtain images of the paravertebral space in the axial/transverse plane with a high-frequency (10–12 MHz) transducer placed lateral to the spinous process. The transverse processes and ribs are seen as hyperechoic structures with acoustic shadowing below them. The paravertebral space can be visualized in this probe orientation as a wedge-shaped hypoechoic layer with the hyperechoic reflections of the pleura below (anterior) and the costotransverse ligamen above (posterior). The hyperechoic line of the pleura can be seen moving with inhalation and exhalation as the visceral and parietal pleura slide against each other. Insert a needle into the paravertebral space and inject local anesthetic, causing a downward or anterior displacement of the pleura. Alternatively, position the ultrasound probe in the sagittal plane. In this orientation, adjacent transverse processes are seen as hyperechoic and squared bony projections. This is in contrast to ribs, which are generally more round in appearance. Deep to the transverse processes, the pleura can generally be easily visualized.
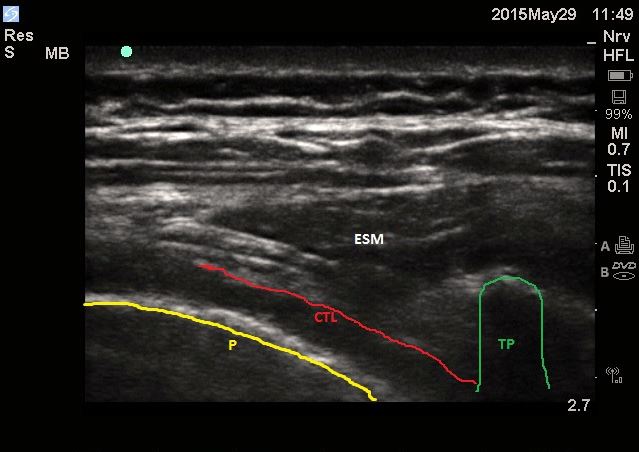 Figure 4. Ultrasound-guided paravertebral block Image courtesy of Arun Kalava, MD
Figure 4. Ultrasound-guided paravertebral block Image courtesy of Arun Kalava, MD
For HALN, use dermatomes T10–L1 and inject about 3–5 mL of local anesthetic (eg, ropivacaine 1%) into each paravertebral space.1 For unilateral PCNL, perform multilevel paravertebral blocks from T10–L1 with approximately 10 mL of 0.5% ropivacaine for each segment.12 For ESWL, unilateral paravertebral block from T8–L1 with injection of about 5 mL 0.5% bupivacaine is adequate.13 See Figure 4.
In conclusion, dorsal penile, ilioinguinal/iliohypogastric, pudendal, and paravertebral nerve blocks can be used as regional techniques in a variety of urologic procedures. Although they may be technically challenging, nerve blocks can be successful in providing analgesia and anesthesia for patients undergoing urologic surgery while decreasing the incidence of adverse events related to systemic opioid administration.
References:
- Clendenen SR, Wehle MJ, Rodriguez GA, Greengrass RA. Paravertebral block provides significant opioid sparing after hand-assisted laparoscopic nephrectomy: an expanded case report of 30 patients. Journal of Endourology.2009;23:1979– https://doi.org/10.1089/end.2009.0095
- Al-Zaben KR, Qudaisat IY, Abu-Halaweh SA, et al. Comparison of ilioinguinal/iliohypogastric nerve blocks and intravenous morphine for control of post-orchidopexy pain in pediatric ambulatory surgery. Middle East J Anaesthesiol. 2014;22(4):393–
- Sandeman DJ, Dilley AV. Ultrasound guided dorsal penile nerve block in children. Anaesth Intensive Care. 2007;35:266–
- O’Sullivan MJ, Mislovic B, Alexander E. Dorsal penile nerve block for male pediatric circumcision—randomized comparison of ultrasound-guided vs anatomical landmark technique. Ped Anesthesia. 2011;21:1214– https://doi.org/10.1111/j.1460-9592.2011.03722.x
- Rose G, Costa V, Drake A, Siadecki S. Ultrasound-guided dorsal penile nerve block performed in a case of zipper entrapment injury. J Clin Ultrasound. 45:589–591. https://doi.org/10.1002/jcu.22459
- Li JY, Yi ML, Liao R. Dorsal penile nerve block with ropivacaine-reduced postoperative catheter-related bladder discomfort in male patients after emergence of general anesthesia. 2016;95:e3409. https://doi.org/10.1097/MD.0000000000003409
- Trainor D, Moeschler S, Pingree M, et al. Landmark-based versus ultrasound-guided ilioinguinal/iliohypogastric nerve blocks in the treatment of chronic postherniorrhapy groin pain: a retrospective study. J Pain Res. 2015;8:767– https://doi.org/10.2147/JPR.S86777
- Demirci A, Efe EM, Türker G, et al. [Iliohypogastric/ilioinguinal nerve block in inguinal hernia repair for postoperative pain management: comparison of the anatomical landmark and ultrasound guided techniques]. Rev Bras Anestesiol. 2014;64(5):350–35 https://doi.org/10.1016/j.bjan.2014.01.001
- Kalava A, Pribish AM, Wiegand LR. Pudendal nerve blocks in men undergoing urethroplasty: a case series. Rom J Anaesth Intensive Care. 2017;24:159– https://doi.org/10.21454/rjaic.7518.242.klv
- Xiaoqiang Li, Xuerong Z, Juan L, et al. Efficacy of pudendal nerve block for alleviation of catheter-related bladder discomfort in male patients undergoing lower urinary tract surgeries. 2017;96(49):1097. https://doi.org/10.1097/MD.0000000000008932
- Kim SH, Song SG, Paek OJ, Lee HJ, Park DH, Lee JK. Nerve-stimulator-guided pudendal nerve block by pararectal approach. Colorectal Dis. 2012;14:61– https://doi.org/10.1111/j.1463-1318.2011.02720.x
- Yang H, Yu X, Hu J, et al. Usage of multilevel paravertebral block as the main anesthesia for mini-invasive PCNL: retrospective review of 45 cases with large stones. Urol Int. 2017;99(3):326– https://doi.org/10.1159/000480094
- Hanoura S, Elsayed M, Eldegwy M, Elsayed A, Ewieda T, Shehab M. Paravertebral block is a proper alternative anesthesia for outpatient lithotripsy. Anesth Essays Res. 2013;7(3):365–3 https://doi.org/10.4103%2F0259-1162.123238
Leave a commentOrder by
Newest on top Oldest on top