Axillary Blockade
Authors
Sean Li, MD
Resident Physician
University of Michigan
Ann Arbor, MI
Hans Sviggum, MD
Resident Physician
Mayo Clinic
Rochester, MN
Paul Hilliard, MD
Lecturer
Division of Pain Medicine
Department of Anesthesiology
University of Michigan
Ann Arbor, MI
Introduction
The axillary brachial plexus block was first described in 1884 by William Halsted, at St. Luke’s-Roosevelt Hospital in New York City. It is one of the most common regional nerve blocks performed for forearm and hand surgery. This approach utilizes superficial and palpable landmarks in localizing the injection site and offers reliable results with few major complications.
Indications
- Anesthesia for surgical procedures at or distal to the elbow
- Anesthesia for closed reduction of fractures at or distal to the elbow
- Analgesia for injuries or post-operative pain control at or distal to the elbow
- Promoting vasodilation after reimplantation/reconstruction at or below the elbow
Contraindications
- Patient refusal
- Surgery/procedure proximal to elbow
- Patient unable to abduct arm
- Infection/open wound in area of proposed injection site
- Coagulopathy
Anatomy
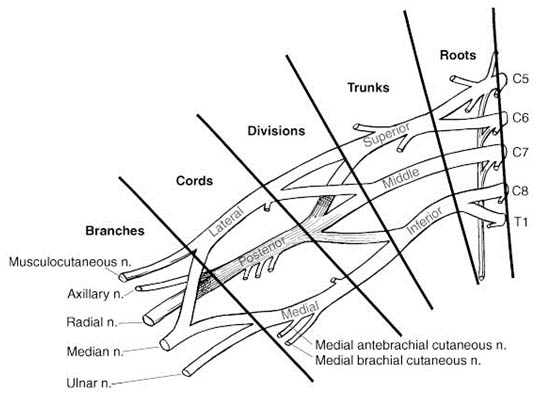
The brachial plexus, consisting of the anterior rami of the lower four cervical and the first thoracic spinal nerves, provides innervation to the upper limb. These five nerve roots (C5−T1) first give rise to three trunks that divide to form divisions and reconstitute into cords that finally split into branches (Figure 1).
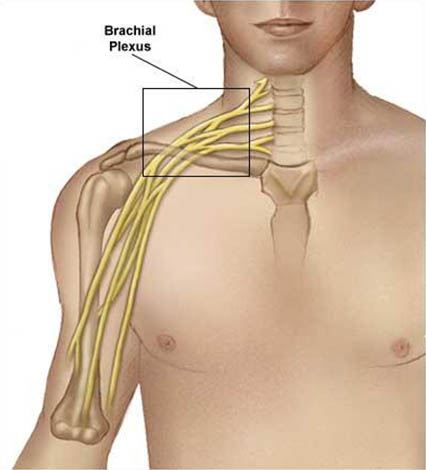
The brachial plexus enters the infraclavicular area as it passes between the clavicle and first rib. Coursing caudad to the coracoid process of the scapula, the brachial plexus then enters the axillary region (Figure 2).
The brachial plexus and axillary artery are contained within a fibrous sheath at the level of the axilla but not necessarily the axillary vein. The goal of the axillary brachial plexus blockade is to deposit an adequate volume of anesthetic solution inside the sheath, allowing it to bathe and anesthetize the terminal nerves of the brachial plexus.
Axillary blockade can reliably anesthetize the median, ulnar, and radial nerves but not the other branches that exit from the brachial plexus and its sheath more proximally. The more proximal branches include the musculocutaneous nerve (motor innervation to the biceps muscle, sensory to the lateral forearm), medial brachial cutaneous nerve (sensory to the lower half of the medial arm), and axillary nerve (sensory to the lateral arm, sensory to the shoulder joint, motor to the deltoid and teres minor muscles). In order to reliably anesthetize these nerves, one must block the brachial plexus at a more proximal level or perform supplemental blocks (see section on supplemental blocks).
Technical Considerations
 Figure 3. Patient and arm position for axillary brachial block
Figure 3. Patient and arm position for axillary brachial block
Patient position
Patient is placed supine with the arm abducted 90 degrees, externally rotated and flexed (Figure 3).
Choice of Local Anesthetic
Common local anesthetics used in axillary blockade include mepivacaine (1-1.5%), lidocaine (1-2%), bupivacaine (0.5%), and ropivacaine (0.5%). Each provides the necessary duration and degree of anesthesia or analgesia when given in sufficient doses. Axillary blockade requires a relatively high volume of local anesthetic (30-40 mL) to achieve complete anesthesia, although the volume can be reduced for ultrasound guided axillary blockade as discussed below.
The alpha-2 agonist clonidine is an important adjuvant to local anesthetics. It is important to weigh the analgesic benefit of clonidine against its potential adverse effects which include sedation, hypotension, and bradycardia, especially at higher doses (> 150 µg). A systematic review by Murphy et. al found that clonidine seemed to provide analgesic benefit without major side effects at doses up to 150 µg. There is little evidence for improved analgesia when opioid is added to brachial plexus blocks. Additionally, there is no apparent difference in opioid induced side effects regardless of the route of administration, peripheral or systemic.
Nerve Localization
Peripheral Nerve Stimulation
- Position the patient supine, with the arm abducted at 90 degrees and elbow flexed. Locate the axillary artery by palpation high in the axilla.
- After a standard sterile prep and drape of the area, infiltrate the skin over the artery with local anesthetic and insert a 22 gauge 5-cm insulated needle either superior or inferior to the artery at a 45 degree angle while palpating the axillary artery pulse with the non-dominant hand (Figure 4).
- Once the needle penetrates the skin, turn on the nerve stimulator at an initial current level of 1-1.2 mA.
- Slowly advance the needle until an appropriate motor response is obtained (often at a depth of 1-2 cm) around 0.5-0.6 mA.
- Evoked motor response (EMR) from stimulation of radial nerve includes extension of the wrist and forearm at the elbow and supination of the forearm. Stimulation of the ulnar nerve causes flexion of the wrist, fourth and fifth digits, and thumb adduction. Stimulation of the median nerve causes flexion of the wrist, second and third digits, thumb opposition, and forearm pronation.
- After negative aspiration, slowly inject 10-20 mL of local anesthetic in 5-mL increments with intermittent aspiration.
- At least two terminal nerves (median, radial, ulnar) should be identified and injected to improve block success.
- Ideally, the nerve innervating the surgical site should be anesthetized first.
- If arterial blood is aspirated during the procedure, conversion to a transarterial technique (described below) is acceptable. Similarly, if a paresthesia is obtained without motor response, injection of local anesthetic after careful assessment of the distribution of the paresthesia is acceptable.
- If the desired motor response is not achieved after advancing 2-3 cm, withdraw the needle and redirect superiorly (laterally) or inferiorly (medially) 10-15 degrees systematically in a stepwise manner.
- The musculocutaneous nerve (forearm flexion or biceps muscle twitch) can be located by directing the needle superior to the artery toward the coracobrachialis muscle. After an appropriate EMR is elicited at 0.5 mA, 5-10 mL of local anesthetic is injected.
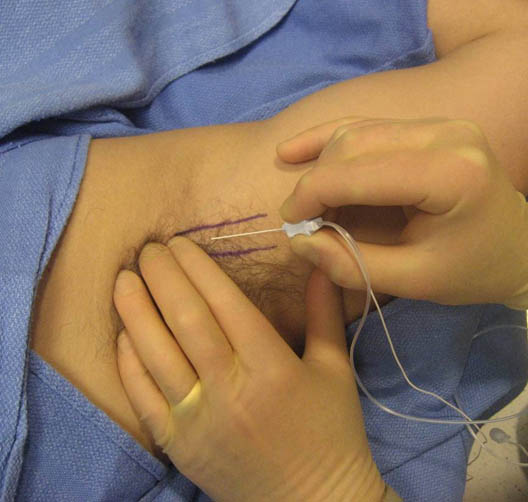 Figure 4. Axillary brachial plexus block using a nerve stimulator needle
Figure 4. Axillary brachial plexus block using a nerve stimulator needle
Trans-arterial Approach
Because the median, ulnar, and radial nerves are located in close proximity to the axillary artery, the axillary artery serves as a reliable guide for local anesthetic injection around these three nerves.
- After a standard sterile prep and drape of the area, infiltrate the skin over the artery and “straddle” the artery with fingers from the non-dominant hand.
- Advance a 25-gauge needle toward and through the axillary artery. Although free flow of arterial blood upon entering the axillary artery should be obvious if one advances the needle slowly enough, many anesthesiologists choose to continuously aspirate while advancing the needle. Once the needle is through the artery, flow of blood through the needle will cease.
- At this posterior position (“behind” the artery), inject 15 – 20 mL of local anesthetic incrementally with intermittent aspiration.
- Withdraw the needle slowly until blood is no longer aspirated again. Inject another 15-20 mL of local anesthetic in the anterior position (“in front of” the artery).
Ultrasound Guidance
Ultrasound (US) guidance has offered an additional technique for axillary blockade. In contrast to more proximal blocks where the nerve structures are “clustered” together, the axillary approach is performed in the upper limb at which individual terminal branches of the brachial plexus can be identified. At the axillary level, the brachial plexus is superficial, thus a high frequency transducer (10-15 MHz) is most suited for neurovascular imaging.
- An in-plane approach is more commonly used than an out-of-plane approach.
- Place the US transducer perpendicular to the long axis of the arm to capture the axillary artery (centered on screen) and individual plexus nerves in cross-section.
- Considerable anatomic variation is noted for all the terminal branches of the brachial plexus; however the most common orientations are shown in Figure 5.
- Median Nerve – anterior lateral to the artery (above and slightly left, at the 10 to 12 o’clock position relative to the artery)
- Ulnar Nerve – anterior medial to the artery (above and to the right, near the axillary vein, 1-3 o’clock position relative to the artery)
- Radial Nerve – posterior medial to the artery (below and to the right, between 3 to 6 o’clock positions relative to the artery)
- Musculocutaneous Nerve – optimal imaging requires more lateral positioning of the transducer as it lies within the coracobrachialis muscle or fascia just below the biceps muscle
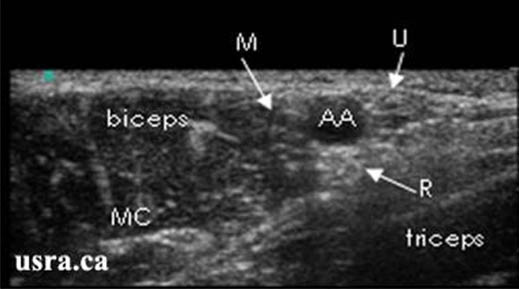 Figure 5. Sonogram of the terminal nerves in the axilla. (M = median nerve, U = ulnar nerve, R = radial nerve, MC = musculocutaneous nerve
Figure 5. Sonogram of the terminal nerves in the axilla. (M = median nerve, U = ulnar nerve, R = radial nerve, MC = musculocutaneous nerve
Downloaded with permission from Ultrasound for Regional Anesthesia (2008)
- After anesthetizing the skin insertion point, insert a 22 gauge 5-cm needle at the edge of the transducer in a superior (lateral) position to the artery and the needle is advanced inferiorly (medially) (Figure 6). It may help to position the needle 1-2 cm from the transducer for an improved angle of incidence, as the mean skin-to-nerve distance is relatively superficial (0.6 ± 0.3 cm) in the axilla.
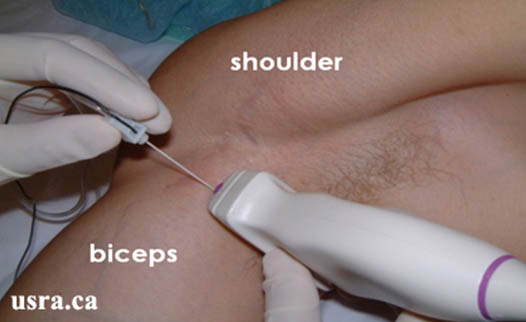 Figure 6. In-plane approach to US guided axillary block
Figure 6. In-plane approach to US guided axillary block
Downloaded with permission from Ultrasound for Regional Anesthesia (2008)
- Direct the needle immediately above or below neural structures to minimize the risk of direct needle trauma.
- Inject 5-10 mL of local anesthetic around each nerve. Although a study by O’Donnell and Iohom demonstrated that US guided axillary blockade could be accomplished with as little as 1 mL of local anesthetic per nerve, higher volumes are recommended to ensure success. Complete circumferential spread may increase the likelihood of a rapid onset and successful block, but is not mandatory.
- The radial nerve, deeper than the other branches, is often injected first by advancing the needle posterior to the artery.
- Following radial nerve injection withdraw the needle and advance anterior to the artery towards the ulnar nerve and then the median nerve in a similar fashion.
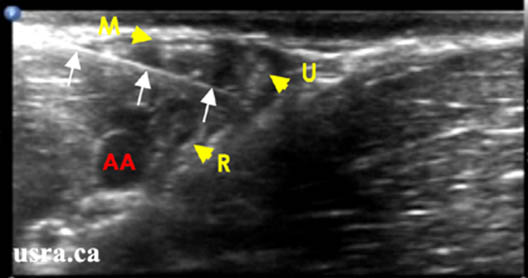 Figure 7. In-plane view of a needle positioned between the ulnar (U) and the radial (R) nerves. Note needle relationship to the median (M) nerve and the axillary artery (AA)
Figure 7. In-plane view of a needle positioned between the ulnar (U) and the radial (R) nerves. Note needle relationship to the median (M) nerve and the axillary artery (AA)
Downloaded with permission from Ultrasound for Regional Anesthesia (2008)
- Withdraw the needle, scan laterally (and possibly more distal) with the transducer to identify the musculocutaneous nerve, and use a similar in-plane injection technique.
- Nerve stimulation may be used in conjunction with ultrasound to verify nerve location.
- Perfect simultaneous viewing of all terminal nerves may be difficult. Proximal or distal scanning with the US transducer may improve nerve imaging.
- Applying pressure with the US transducer to collapse the axillary vein(s) will allow an easier path to the ulnar nerve.
Perivascular Ultrasound-Guided Technique
- A 2012 study (Bernucci et al.) showed that using ultrasound guidance to place the local anesthetic dorsal (6 o’clock position) to the axillary artery was just as successful as individually placing local anesthetic around the radian, ulnar, and median nerves – and resulted in less needle passes and paresthesias. The musculocutaneous nerve is individually anesthetized as above.
- This technique is similar to a transarterial technique in concept, but does involve puncturing the artery and is performed under direct visualization by ultrasound.
- Another 2012 study (Tran et al.) by the same group showed that there was no difference in success rates or complications between injection local anesthetic at the 6 o’clock position, the 12 and 6 o’clock positions, or the 2, 10, and 6 o’clock positions to the artery in addition to a musculocutaneous nerve block when total volumes of local anesthetic were the same.
Alternative Techniques
- Paresthesia technique
- Fascial clicks technique
Supplemental Nerve Blocks
- Musculocutaneous nerve block can be performed by injecting 5-10 mL of local anesthetic into the body of the coracobrachialis muscle in a fanlike manner in a lateral to medial plane. This technique is indicated if the musculocutaneous nerve is not identified by nerve stimulation/ultrasound or if a transarterial approach is used.
- Intercostobrachial and medial brachial cutaneous nerve block helps to prevent tourniquet-related pain because the intercostobrachial nerve (T2) joins the medial brachial cutaneous nerve to innervate the skin of the upper half of the medial and posterior part of the arm. At the site of needle insertion, 5-8 mL of local anesthetic is injected subcutaneously across the axilla both superior and inferior to the artery. The intercostobrachial nerve may be seen on ultrasound imaging, and does not always need a separate supplemental block if performed proximal enough or viewed on ultrasound.
Efficacy of Various Techniques
Successful blockade of the brachial plexus via an axillary approach varies from 60-100% based on the technique and criteria of “success.” Without using ultrasound guidance, most studies suggest that 2-injection transarterial techniques are equivalent to the single paresthesia and single nerve stimulation techniques. However, obtaining multiple nerve stimulations has been shown to be superior to the previously mentioned techniques. Although multiple stimulations require more time, block onset and readiness for surgery may be faster. It is important to keep in mind that the specific nerves targeted may be more important than the overall number of nerves injected depending on the location of surgery. Most studies comparing US guided blocks to nerve stimulation or landmark-guided blocks have shown that US guided axillary blockade either improved block success or had similar success rates.
- Casati et al. found that US guided axillary blockade had a similar success rate and similar patient satisfaction but a faster onset of sensory blockade when compared with a multiple injection nerve stimulation technique.
- Chan et al. showed a shorter procedure time and a faster onset of sensory block with US guided perineural injections than with a multiple nerve stimulation technique. However, the rates of block success for surgery were similar (92% vs. 86%).
- Soeding et al. found a higher rate of successful blocks with US guided blockade when compared with “landmark” techniques.
- As mentioned above, using an ultrasound-guided “perivascular” technique has been shown to have similar efficacy to an ultrasound guided technique aiming to anesthetize the radial, ulnar, and median nerves separately (in addition to separate musculocutaneous injection in both groups).
Complications
As with all regional anesthesia techniques, accidental intravascular local anesthetic injection, systemic local anesthetic toxicity, infection, neural injury, and bleeding are possible complications. Given that a high volume of local anesthetic (30-40 mL) is used for axillary block, it is essential to perform incremental injections to limit local anesthetic toxicity. Transient postoperative dysesthesias may occur in up to 4% of cases, but permanent neurologic injuries are exceedingly rare. The method of neural localization (nerve stimulation, transarterial, paresthesia, or ultrasound guided) has not been shown to influence the rate of complications.
Summary
Axillary blockade is an old anesthetic technique that has stood the test of time. It has been used with great success for anesthesia and analgesia for a variety of procedures in the forearm and hand. This block can be performed by a number of different techniques including nerve stimulation, ultrasound, and transarterial. It offers several advantages over other techniques blocking the brachial plexus, most notably avoiding the possibility of pneumothorax or phrenic nerve blockade. Its efficacy and safety ensure that it will continue to be widely applied.
References
- Neal JM, Hebl JR, Gerancher JC, et al. Brachial Plexus Anesthesia: Essentials of Our Current Understanding. Reg Anesth Pain Med 2002;27:402-428
- Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain-Medicine evidence-based guidelines (third edition) Reg Anesth Pain Med 2010;35:64-101
- Weinberg G. Current concepts in resuscitation of patients with local anesthetic cardiac toxicity. Reg Anesth Pain Med. 2002; 27:568-75
- Kopp SL, Smith HM. Axillary Blockade. In: Hebl JR, Lennon RL ed. Mayo Clinic Atlas of Regional Anesthesia and Ultrasound-Guided Nerve Blockade. New York: Oxford University Press, 2010; 251-70
- Winnie AP, and Håkansson L. Axillary Perivascular Technique of Brachial Plexus Blocks. Plexus Anesthesia. W.B. Saunders.1983:121-143
- Tindinwebwa JB. Axillary Brachial Plexus Block. Update in Anesthesia 1995; 5: Article 4
- Rodziewicz T. Axillary Block. MorCORE Keywords: Peripheral Nerve Blocks. Department of Anesthesia, University of Michigan http://anes.med.umich.edu/index.html
- Wedel D, Horlocker T. Chapter 52: Nerve Blocks. Miller’s Anesthesia, 7th ed. Elsevier; 2009
- Brachial Plexus Anatomy. Wikipedia: 2009http://en.wikipedia.org/wiki/Brachial_plexus.html
- Retzl G, Kapral S, Greher M, et al. Ultrasonographic Findings of the Axillary Part of the Brachial Plexus. Anesth Analg 2001;92:1271-5
- Perias A, Chan V, Simons M. Brachial Plexus Examination and Localization Using Ultrasound and Electrical Stimulation. Anesthesiology 2003;99:429-35
- Murphy D, McCartney C, Chan V. Novel Analgesic Adjuncts for Brachial Plexus Block: A Systematic Review. Anesth Analg 2000;90:1122-28
- Casati A, Danelli G, Baciarello M, et al. A prospective, randomized comparison between ultrasound and nerve stimulation guidance for multiple injection axillary brachial plexus block. Anesthesiology 2007;106:992-6
- Soeding PE, Sha S, Royse CE, et al. A randomized trial of ultrasound-guided brachial plexus anaesthesia in upper limb surgery. Anaesth Intensive Care 2005;33:719-25
- O’Donnell BD, Iohom G. An estimation of the minimum effective anesthetic volume of 2% lidocaine in ultrasound-guided axillary brachial plexus block. Anesthesiology 2009; 111:25-9
- Bernucci F, Gonzalez AP, Finlayson RJ, Tran de QH. A prospective, randomized comparison between perivascular and perineural ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med 2012; 37:473-7
- Tran de QH, Pham K, Dugani S, Finlayson RJ. A prospective, randomized comparison between double-, triple-, and quadruple-injection ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med 2012; 37:248-53
Leave a commentOrder by
Newest on top Oldest on top